Dilaceration and Eruption Disturbances in Permanent Teeth: A Sequelae of Trauma to Their Predecessors-Diagnosis and Treatment Using Cone Beam CT
Mahesh R1, Kanimozhi IG2, Sivakumar M3
1 Senior Lecturer, Department of Paediatric Dentistry, Saveetha Dental College, Chennai, India.
2 Senior Lecturer, Department of Pedodontics and Preventive Dentistry, Sree Ramachandra University, India.
3 Senior Lecturer, Department of Oral Pathology, Madha Dental College, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mahesh R, Senior Lecturer, Department of Paediatric Dentistry, Saveetha Dental College, Poonamalle High Road, Vellapanchavadi, Chennai-600 072, India.
Phone: 9840322728,
E-mail: maheshpedo@gmail.com
Alterations in the morphology of permanent teeth following trauma to their predecessors is a challenging task for diagnosis and it may require advanced imaging techniques. Newer imaging modalities have replaced the conventional radiological procedures, as they allow 3D reconstruction images and views which are free of superimposition. Cone Beam CT (CBCT) offers a three-dimensional view, which the conventional two-dimensional dental radiography fails to provide. The current article highlights the advantages of CBCT which are seen in evaluation of the morphological variations and eruptive disturbances in the permanent teeth, as sequelae to trauma in their predecessors.
Sequelae of trauma, Cone beam CT, Dilaceration
Case Report
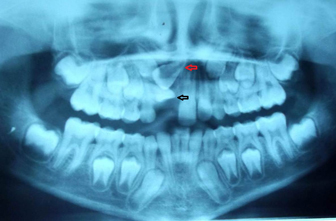
A 10-year-old boy was referred to our Paediatric Dentistry Department with complaint of non-eruption of the permanent maxillary right central and lateral incisors (tooth 11 and tooth 12). Patient history revealed intrusive injuries to the deciduous maxillary teeth (teeth 51, 52, and 61) that had led to their extractions when the child was 4-year-old. Intraoral examination showed that he had a mixed dentition, with clinically missing maxillary right central and lateral incisors (tooth 11 and tooth 12) and retained maxillary primary lateral incisor (tooth 52) [Table/Fig-1]. Orthopantogram showed impacted tooth 11 and associated possibility of root dilaceration; tooth 12 was found to be displaced horizontally, thus blocking the eruption of tooth 11 [Table/Fig-2].
Photograph showing missing maxillary right central incisor.

Panoramic radiograph shows horizontal impaction in tooth 12 (Black arrow) and root dilaceration in tooth 11 (Red arrow).
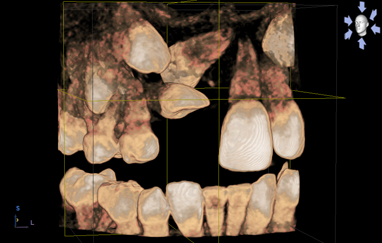
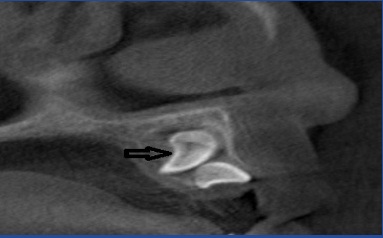
A cone-beam CT scan (Galileos, Sirona Dental Systems, Germany) at 120 KV and 55 mAs was performed to assess the extent of dilaceration, if any, and to aid in the creation of a suitable treatment plan. The three-dimensional view from the CT scan [Table/Fig-3,4]. Revealed horizontal impaction in tooth 12, which was in close proximity to the crown of tooth 11 and maxillary right canine (tooth 13). The crown tip of the maxillary right first premolar (tooth 14) was found to touch the root surface of tooth 12, thus causing some root resorption, which was confirmed in the sequential trans-axial views of the CT scan [Table/Fig-5a]. Tooth 11 showed palatal displacement of the crown and a gradual curvature in the apical 1/3rd of the root [Table/Fig-5b and 6].
3-D view of cone-beam computed tomography (CT) scan reveals the position of impacted tooth 11 (Red arrow) and horizontally placed tooth 12 (Black arrow)

3D reconstructed image demonstrates inverted tooth 11 and its relationship with tooth 12.
Transaxial CT view in the right maxillary region shows external root resorption in tooth 12 (Black arrow)

Sequential Transaxial CT view reveals dilaceration in tooth 11 and close relationship with tooth 12 (Black arrow)

Cross-sectional CT view demonstrates tooth 12 blocking the eruption of tooth 11 (Black arrow)
The treatment plan included extraction of tooth 22, to facilitate surgical exposure for orthodontic bonding, followed by extrusion of tooth 11. Tooth 13 was allowed to erupt in the position of tooth 12.
Discussion
Developmental disturbances in permanent teeth, which are caused by trauma to their predecessors, have a frequency that ranges from 12% to 74% [1]. The highest frequency of malformations was found following subluxation injuries. Among the luxation injuries, intrusion injuries were associated with the more severe malformations [2]. The severity depends on the age of the child at the time of injury, the grade of root resorption of the traumatized deciduous tooth, the type and extension of the injury and the development stage of the successor at the time of injury [3].
Among the developmental disturbances, impaction and alteration in tooth morphology represent a clinical challenge with regards to diagnosis, treatment plan, and prognosis. These situations imply the need for advanced imaging techniques rather than the conventional radiographs. New imaging modalities such as CBCT result in better diagnosis and more efficient management of the complex malformations. Hence, advanced imaging techniques are an essential requirement, to arrive at the correct diagnosis and for choosing optimal treatment plan, as well as to monitor and document the treatment progress and final outcome [4].
The information obtained from imaging studies can enhance the dentist’s ability to localize impacted or transposed teeth, as well as identify pathological conditions and root resorption. This can help in planning surgical access and bond placement, as well as in defining the optimal and most efficient path for extrusion into the oral cavity, that avoids or minimizes collateral damage [5].
Trauma in the primary dentition has the potential to cause some damage to the tooth germs of permanent successor. The close relationship between the root apex of primary teeth and the permanent tooth germ explains the easy occurrence of disturbances in the permanent teeth [6]. Intrusive injury to the primary tooth often results in it being driven deeply into the alveolar bone, invading the follicle of the permanent germ and possibly destroying the enamel matrix. As ameloblasts are irreplaceable and as no further cell division occurs, localized arrest of crown development is likely to occur after trauma [6]. The degree of germ malformation is directly related to the development stage at the time of the trauma and the direction of the traumatic forces [2,6].
Root dilaceration is characterized by angulation or curvature of the root of the permanent tooth, following trauma to their primary predecessors and it has a prevalence rate of 4.7% [7]. The prevalence of eruption disturbances in the permanent anterior teeth, following trauma to their predecessors, is seen in 17.9% of the cases [1]. These cases present a wide range of diagnostic challenges to the clinicians. The situation is more complicated in mixed dentition stage, where any surgical removal of impacted teeth demands precise knowledge on the tooth location in the jaw and its relationship with other teeth and surrounding anatomical structures.
Not all of these can be addressed by conventional dental radiography alone. Traditional radiographs offer only a two-dimensional view of three-dimensional structures [8]. CBCT overcomes this major limitation by allowing us to visualize the third dimension view, while eliminating superimpositions at the same time [9]. It is useful in identification of morphological variations of a tooth and in localization of the impacted tooth. Such information is essential for planning restorations that involve orthodontic / surgical repositioning. CBCT has the potential to evaluate the amount of bone which overlies the impacted teeth, an application that can be developed to reduce operating room occupation time. While SLOB technique can only indicate the positioning of the tooth, the exact curvature of the root, the amount of bone covering the tooth should be estimated before treatment planning, which can only be analyzed by using CBCT. Orthographic tomographic slices and panoramic reconstructions are superior to conventional panoramic radiographs in determining the location, orientation of an impacted tooth, and its relationship to adjacent vital structures in the maxilla and the mandible [8].
The introduction of CBCT has represented an important new development in dento-maxillofacial radiology, and it has also precipitated a shift from two-dimensional to three-dimensional data acquisition, image reconstruction, and visualization [10]. In the present case, CBCT has been useful in analyzing the dental-osseous structures, determination of position of the impacted tooth, angulation, degree of crown-root dilaceration, and morphological alteration. The information which was thus obtained was helpful in treatment planning and exact localization of the impacted tooth for surgical extrusion.
Though the amount of radiation exposure to the patient, which is seen during conventional radiography is lower than that which is seen during other imaging modalities, when better and advanced imaging modalities for diagnosis are required, CBCT should be considered as an option. Clinicians should have up-to-date knowledge on the use of conventional and advanced imaging modalities, for providing the best health-to-risk ratio for the patient.
Conclusion
In conclusion, CBCT offers an additional advantage over conventional radiographs in analyzing the three dimensional morphologies of impacted teeth. CBCT imaging is likely to provide valuable diagnostic information for identifying the exact location of the impacted tooth and to aid in better surgical planning.
[1]. do Espirito Santo Jacomo DR, Campos V, Prevalence of sequelae in the permanent anterior teeth after trauma in their predecessors: a longitudinal study of 8 yearsDent Traumatol 2009 25:300-4. [Google Scholar]
[2]. Scerri E, Gatt G, Camilleri S, Mupparapu M, Morphologic and developmental disturbances of permanent teeth following trauma to primary dentition in a selected group of Maltese childrenQuintessence Int 2010 41:717-24. [Google Scholar]
[3]. Borum MK, Andreasen JO, Sequelae of trauma to primary maxillary incisors. I. Complications in the primary dentitionEndod Dent Traumatol 1998 14:31-44. [Google Scholar]
[4]. Shortliffe EH, Perreault LE, Wiederhold G, Fagan LM, Medical informatics: Computer applications in health care and biomedicine 2001 2nd ednNew YorkSpringer [Google Scholar]
[5]. Kapila S, Conley RS, Harrell WE Jr, The current status of cone beam computed tomography imaging in orthodonticsDentomaxillofac Radiol 2011 40:24-34. [Google Scholar]
[6]. Andreasen JO, Injuries to developing teethIn: Traumatic injuries of the teeth 1981 CopenhagenMunksgaard:273-320. [Google Scholar]
[7]. Ben-Bassat Y, Brin I, Zilberman Y, Effects of trauma to the primary incisors on their permanent successors: multidisciplinary treatmentASDC J Dent Child 1989 56:112-6. [Google Scholar]
[8]. Bouwens DG, Cevidanes L, Ludlow JB, Phillips C, Comparison of mesiodistal root angulation with post treatment panoramic radiographs and cone-beam computed tomographyAm J Orthod Dentofacial Orthop 2011 139:126-32. [Google Scholar]
[9]. Cohenca N, Simon JH, Roges R, Morag Y, Malfaz JM, Clinical indications for digital imaging in dento-alveolar trauma. Part 1: traumatic injuriesDent Traumatol 2007 23:95-104. [Google Scholar]
[10]. Bornstein MM, Wölner-Hanssen AB, Sendi P, von Arx T, Comparison of intraoral radiography and limited cone beam computed tomography for the assessment of root-fractured permanent teethDent Traumatol 2009 25:571-7. [Google Scholar]