Pulmonary Infection Caused by Achromobacter xylosoxidans in a Patient with Carcinoma of Epiglottis: A Rare Case
Priyamvada Roy1
1 Senior Resident, Department of Microbiology, Laboratory Medicine, Delhi State Cancer Institute, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Priyamvada Roy, Care of Group Captain D D Roy, Flat Number C-115, Jalvayu Vihar (Near AWHO), Plot Number 8, Pocket P-4, Builder’s Area, Greater Noida, Uttar Pradesh-201310, India.
Phone: 9953820283,
E-mail: priyamvadaroy@yahoo.in
Achromobacter xylosoxidans is an aerobic, motile, oxidase and catalase positive, non-fermenting, gram negative bacillus. It is an opportunistic pathogen which is responsible for various nosocomial and community-acquired infections. However, there are only very few reports of pulmonary infections caused by this bacterium in cancer patients.
We are presenting a case of a patient with carcinoma of epiglottis, who developed pulmonary infection caused by Achromobacter xylosoxidans. According to the available literature, this is the first case of pulmonary infection caused by Achromobacter xylosoxidans, which was detected in a cancer patient in India. Since Achromobacter xylosoxidans demonstrates resistance to many classes of antimicrobials, vigilant and efficient microbiological work-ups and surveillances are needed, to diagnose infections caused by this rare pathogen in clinical settings.
Achromobacter xylosoxidans, Granulocyte colony stimulating factor, Malignancy, Pneumonia
Case Report
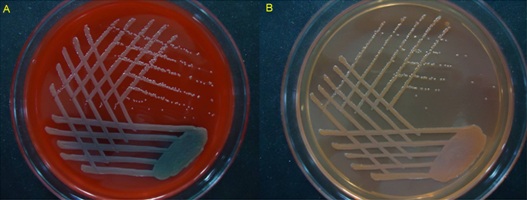
A 60-year-old male patient who had carcinoma of epiglottis, who underwent chemotherapy and radiotherapy at Delhi State Cancer Institute for three months, presented with purulent sputum, fever with chills, breathlessness and weakness on 8th of August, 2013. His haematological parameters showed leucopenia (3040/ μl) with monocytosis (N-54.7%, L-20.9%, M-22.2%, E-2%, B-0.2%). A good quality sputum sample was collected aseptically and it was processed as per standard microbiological procedures. Gram staining of the sputum sample revealed leukocytes and gram negative bacilli. The sample was cultured on blood agar and MacConkey agar and the plates were incubated for 24 hours at 37°C. After overnight incubation, blood agar showed glistening, smooth, pinpoint, non-haemolytic colonies; on MacConkey agar, non-lactose fermenting, low convex colonies were formed [Table/Fig-1]. Colonies were catalase positive and oxidase positive. Gram stained smears obtained from the growth revealed gram negative, non-sporing bacilli. The bacilli were motile in nature. The growth was then subjected to identification by the automated VITEKR 2 Compact (C) (Biomeriux, North Carolina / USA) by using gram negative GN REF 21341 identification (GNID) card. The organism was identified as Achromobacter xylosoxidans, and this was confirmed by promptly culturing a repeat sample from the patient. Antibiotic susceptibility was determined in VITEK by using AST Card N281. The isolate was found to be sensitive to piperacillin (minimum inhibitory concentration or MIC-<=4μg/ml), piperacillin-tazobaztam (MIC-<=4μg/ml), imipenem (MIC-2μg/ml), meropenem (MIC-4 μg/ml), cefoperazone-sulbactam (MIC-<=8μg/ml), trimethoprim/sulfamethoxazole (MIC-<=20μg/ml) and tigecycline (MIC-2μg/ml) and it was found to be resistant to all aminoglycosides (amikacin MIC->=64 μg/ml, gentamicin MIC->=16 μg/ml), ceftriaxone (MIC->=64μg/ml), cefepime (MIC->=32μg/ml), ceftazidime (MIC->=32μg/ml), ciprofloxacin (MIC->=4μg/ml), and tetracycline (MIC->=16μg/ml) . The patient was started on Granulocyte colony stimulating factor (G-CSF) injection, to reverse the myelosuppression which was induced by cytotoxic drugs and on piperacillin-tazobactam 4.5 grams intravenously, every 6 hours. Within a week, the patient’s respiratory complaints subsided and his leucocyte count came back to normal (6610/ μl).
Growth of Achromobacter xylosoxidans obtained after 24 hours of incubation at 37°C on Blood Agar (A) and MacConkey Agar (B). (A) – On Blood agar colonies are glistening, smooth, pinpoint and non-hemolytic. (B)- On MacConkey agar colonies are glistening, smooth, pinpoint, low convex and non-lactose fermenting
Discussion
Being first described by Yabuuchi and Ohyama in 1971, after being isolated from ear discharges obtained from patients with chronic otitis media, Achromobacter xylosoxidans was included in the family, Alcaligenaceae [1]. Achromobacter xylosoxidans, formerly called Alcaligenes xylosoxidans, is an aerobic, non-fermenting, gram-negative bacillus with low virulence [2]. It is rarely isolated from clinical material. Achromobacter xylosoxidans can be confused with other non-fermentative, gram-negative rods, especially Pseudomonas species, in clinical specimens, and so its role as a significant pathogen may be underestimated [3]. A recent reclassification of the bacterium which was done, denoted two subspecies, namely, denitrificans and xylosoxidans, under the species xylosoxidans [4]. Achromobacter xylosoxidans normally inhabits aquatic sources in the environment and hospitals, as well as the human gut, but it may cause nosocomial and community-acquired infections. Achromobacter xylosoxidans is widely considered to be an opportunistic bacterium with low virulence. However, invasive infections caused by this bacterium in immunocompromised individuals and neonates show significant rates of morbidity and mortality [5]. Bacteraemia is the most common manifestation of Achromobacter xylosoxidans infection.
The most common predisposing underlying medical issues observed in the setting of Achromobacter xylosoxidans infections are malignancies, both haematologic and solid organ cancers, cardiac diseases, and immunosuppression [5,6]. Other documented co-morbidities include HIV infection, cystic fibrosis (CF), Diabetes mellitus, chronic renal failure, chronic obstructive pulmonary disease (COPD), cirrhosis, intravenous drug abuse, treatment with high-dose corticosteroids, rheumatoid arthritis with immunomodulation therapy, and underlying urologic abnormalities [1].
While primary, uncomplicated bacteraemia is the most common manifestation of Achromobacter xylosoxidans infection, this organism has been associated with a wide range of clinical infections. Achromobacter xylosoxidans has been isolated from cases of ear and eye infections, urinary tract infections, intra-abdominal infections, liver abscesses, soft tissue infections, osteomyelitis, arthroplasty infections, meningitis, ventriculitis and endocarditis. Pulmonary cases of Achromobacter xylosoxidans infection have been associated with a myriad of underlying medical problems, which include IgM deficiency, haematologic malignancies which include acute myelogenous leukaemia and solid organ malignancies, COPD, and CF [1]. [Table/Fig-2] gives an exhaustive list of published cases of pulmonary Achromobacter xylosoxidans infections in cancer patients till date. To the best of our knowledge, pulmonary infections caused by Achromobacter xylosoxidans in patients with underlying malignancies have been documented in only few publications till date [Table/Fig-2], and such cases have never been reported from India. Though studies on this rare pathogen have been done in our country, as far as oncology patients are concerned, only one case of Achromobacter xylosoxidans infection which occurred in a cancer patient was reported by Eshwara et al., [2], in which the organism was found to cause a local wound infection of metastatic ductal carcinoma of the breast. Hence, this is the first case of pulmonary infection caused by Achromobacter xylosoxidans in a patient with an underlying malignancy in the Indian setting.
Published cases of pulmonary Achromobacter xylosoxidans infections in patients with malignancy
| Serial no. | Study by | Clinical presentation | Comorbidity | Year | Country |
|---|
| 1. | Gomez-Cerezo et al., [6] | Pneumonia (6 cases) | Solid and haematological malignancies | 2004 | Spain |
| 2. | Legrand et al., [10] | Pneumonia (2 cases) | Adenocarcinoma of breast, acute myelogenous leukemia | 1992 | USA |
| 3. | Arroyo et al., [11] | Pneumonia (3 cases) | Prostatic carcinoma, non-Hodgkin’s lymphoma, bronchogenic carcinoma | 1987 | USA |
| 4. | Reverdy et al., [12] | Pneumonia | Acute Myeloblastic Leukemia | 1984 | France |
Achromobacter xylosoxidans is characteristically resistant to all aminoglycosides and rifampin, while it expresses variable resistance to trimethoprim-sulfamethoxazole, ciprofloxacin, and other quinolones [5–7]. Most of the isolates are generally susceptible to carbapenems and antipseudomonal penicillins [5,6]. Currently, there are no specific standardized sensitivities for this organism, although MIC interpretive criteria for “Other Non-Enterobacteriacaea” from CLSI document M100-S23 may be used; there are no disk diffusion interpretive criteria for these organisms [8]. In-vitro data suggests that the most active agents may be minocycline, meropenem or imipenem, piperacillin-tazobactam and chloramphenicol [9]. In the present case report, the patient was successfully treated with piperacillin-tazobactam.
Conclusion
Achromobacter xylosoxidans, being infrequently isolated in clinical microbiology laboratories, faces a delay in identification and adds to the diagnostic dilemma because of its saprophytic nature. Often, it is overlooked as a contaminant. This bacterium demonstrates resistance to many classes of antimicrobials, which may further complicate therapy management and it should always be guided by antibiograms. The present case highlights the significance of this uncommon bacterium in patients with malignancies in the Indian setting and it advocates greater vigilance towards appropriate identification of this organism.
[1]. Claassen SL, Reese JM, Mysliwiec V, Mahlen SD, Achromobacter xylosoxidans infection presenting as a pulmonary nodule mimicking cancerJ Clin Microbiol July 2011 49(7):2751-4. [Google Scholar]
[2]. Eshwara VK, Mukhopadhyay C, Mohan S, Prakash R, Pai G, Two unique presentations of Achromobacter xylosoxidans infections in clinical settingsJ Infect Dev Ctries 2011 5(2):138-41. [Google Scholar]
[3]. Shie SS, Huang CT, Leu HS, Characteristics of Achromobacter xylosoxidans Bacteremia in Northern TaiwanJ Microbiol Immunol Infect 2005 38:277-82. [Google Scholar]
[4]. Garrity GM, Brenner DJ, Kreig NR, Staley JT, Bergey’s Manual of Systematic Bacteriology 2005 22nd edSpringer-VerlagNew York-Berlin-Heidelberg:658-9. [Google Scholar]
[5]. Aisenberg G, Rolston KV, Safdar A, Bacteremia caused by Achromobacter and Alcaligenes species in 46 patients with cancer (1989-2003)Cancer 2004 101:2134-40. [Google Scholar]
[6]. Gomez-Cerezo J, Suarez I, Rios JJ, Pena P, Garcia de Miguel MJ, de Jose M, Achromobacter xylosoxidans bacteremia: a 10-year analysis of 54 casesEur J Clin Microbiol Infect Dis 2003 22:360-3. [Google Scholar]
[7]. Teng SO, Ou TY, Hsieh YC, Lee WC, Lin YC, Lee WS, Complicated Intra-abdominal Infection Caused by Extended Drug Resistant Achromobacter xylosoxidansJ Microbiol Immunol Infect 2009 42:176-80. [Google Scholar]
[8]. Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing; Twenty third Informational supplement. CLSI document. M100-S23, 2013 [Google Scholar]
[9]. Saiman L, Chen Y, Tabibi S, Gabriel PS, Zhou J, Liu Z, Identification and antimicrobial susceptibility of Alcaligenes xylosoxidans isolated from patients with cystic fibrosisJ Clin Microbiol 2001 39:3942-5. [Google Scholar]
[10]. Legrand C, Anaissie E, Bacteremia due to Achromobacter xylosoxidans in patients with cancerClin Infect Dis 1992 14:479-84. [Google Scholar]
[11]. Arroyo JC, Jordan W, Lema MW, Brown A, Diversity of plasmids in Achromobacter xylosoxidans isolates responsible for a seemingly common-source nosocomial outbreakJ Clin Microbiol 1987 25:1952-5. [Google Scholar]
[12]. Reverdy ME, Freney J, Fleurette J, Coulet M, Surgot M, Marmet D, Nosocomial colonization and infection by Achromobacter xylosoxidansJ Clin Microbiol 1984 19:140-3. [Google Scholar]