Multicentric Aggressive Mammary Fibromatosis with Cytological Features and Review of Literature
Parul Garg1, Sanjay Singh Chufal2, Nilakshi Gupta3, Prabhat Pant4, Naveen Chandra Thapliyal5
1 Assistant Professor, Department of Pathology, Maharishi Markandeshwar Medical College and Hospital, Solan, India.
2 Assistant Professor, Department of Pathology, Government Medical College, Haldwani, India.
3 Junior Resident, Department of Pathology, Government Medical College, Haldwani, India.
4 Assistant Professor, Department of Pathology, Government Medical College, Haldwani, India.
5 Professor, Department of Pathology, Government Medical College, Haldwani, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Parul Garg, M/S Meera Thread Factory, Near Raman Cinema, Mansa District Mansa, Punjab-151505, India.
Phone: 8628830845,
E-mail: dr_gargparul48@yahoo.co.in
Fibromatosis is a fibroblastic lesion composed of uniform fibroblasts and collagen with an infiltrative growth pattern but lacking malignant cytological features. It is a rare entity and is even more unusual when found in the breast. Multicentricity in fibromatosis has been reported in 10% cases. Multicentricity in breast cancer has been defined as the presence of two or more tumor foci within different quadrants of the same breast. Considering this definition of multicentricity for fibromatosis, we herein report a case of recurrent multicentric aggressive mammary fibromatosis and its cytological features with review of literature because of limited literature of (FNAC) in mammary fibromatosis.
Mammary Fibromatosis, Multicentricity, Aggressive, FNAC
Case Report
A 35-year-old female presented in the Out Patient Department (OPD) with a mass in left breast since one year. On clinical examination, three lobulated masses were seen which were firm, poorly circumscribed, involving almost the whole of breast. A scar mark was present with absence of nipple and areola. No skin involvement was seen. Left axillary lymph nodes were palpable. Mammography showed suspicious opacity. The right breast was normal. There was a past history of surgery on the same breast.
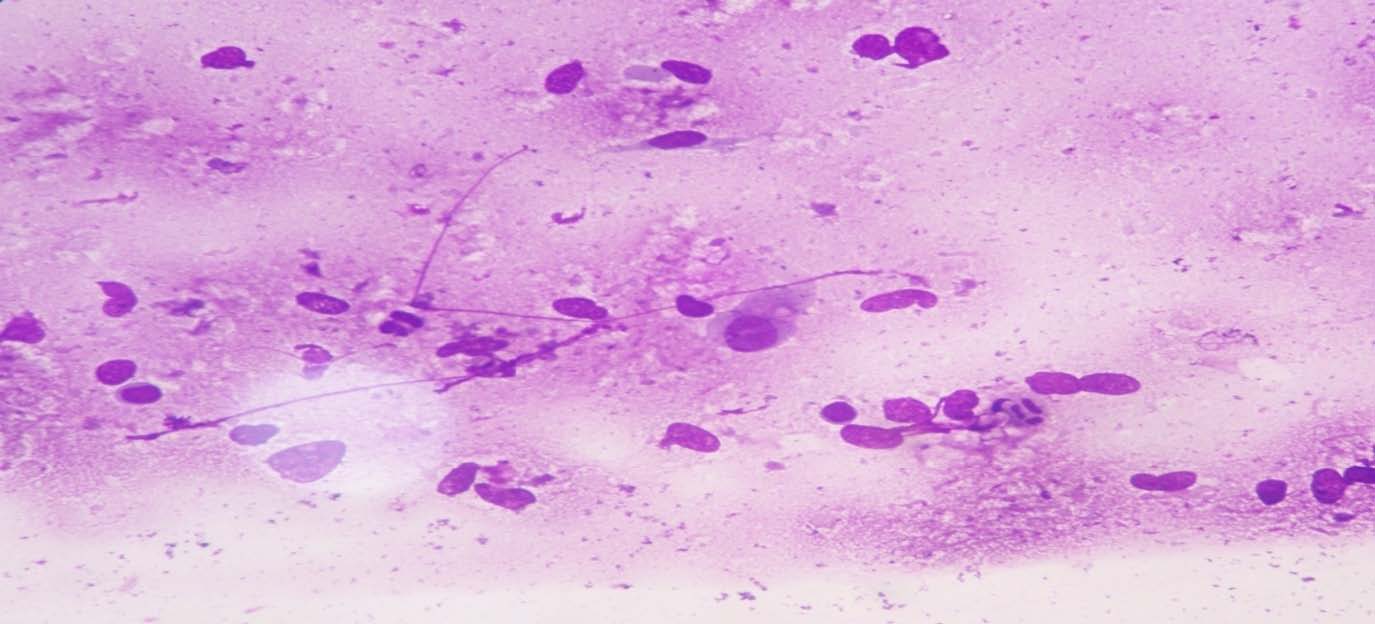
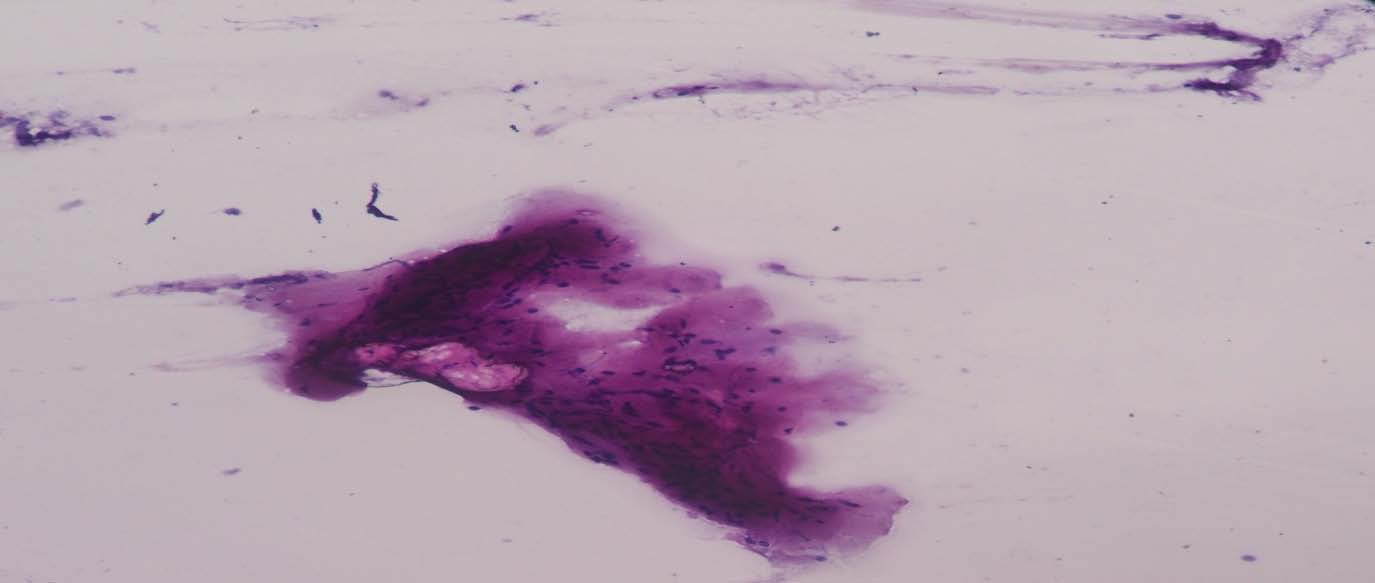
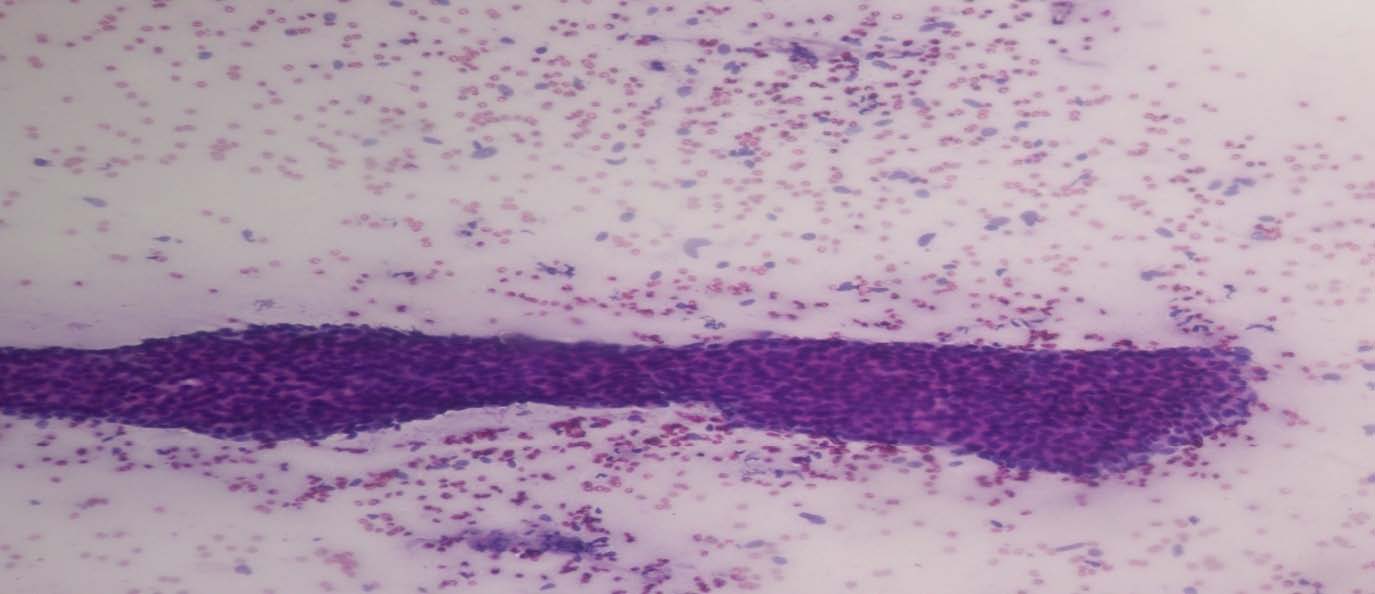
FNAC was done from left breast lump and left axillary lymph nodes. Smears prepared were stained with May Grunwald Giemsa (MGG), Papanicolaou (PAP) and Hematoxylin & Eosin (H&E). Smears were moderately cellular and showed fair number of scattered ovoid to spindle cells, some polyhedral myofibroblast like cells with cytoplasmic extension [Table/Fig-1a], occasional stromal fragments [Table/Fig-1b], sheets of ductal epithelial cells [Table/Fig-1c] and collagen matrix material. The cells were oval to spindle in shape with indistinct cytoplasmic borders and elongated mildly pleomorphic nuclei having blunt or pointed ends with fine nuclear chromatin.Nucleoli, hyperchromasia or mitotic activity was not seen. Some of the nuclei were stripped of cytoplasm [Table/Fig-1c]. Based on cytological features a diagnosis of benign spindle cell lesion was given. FNA smears from enlarged left axillary lymph nodes showed reactive pathology.
Cytological smears showing scattered ovoid to spindle cells along with myofibroblast like cells and stripped nuclei (MGG, x400)
Cytological smears showing stromal fragments (MGG, x400)
Cytological smears showing sheets of ductal epithelial cells along with stripped nuclei (MGG, x100)
Since the lesion was large with suspicious mammography, the patient was offered surgery. Modified radical mastectomy was done.
Pathological Findings
The mastectomy specimen measured 25 × 14 × 5.5 cm and showed three lobulated masses in upper outer, lower outer and lower inner quadrants of the breast [Table/Fig-2a], ranging from 6 cm × 5 cm to 4cm × 4 cm. Nipple areola complex was not identified. A linear scar mark measuring 7.5 cm was present. Serial cut sections through the parenchyma showed grayish white firm circumscribed area involving the whole breast [Table/Fig-2b] as well as the base [Table/Fig-2c].
Gross showing mastectomy specimen with three lobulated masses in different quadrants of breast

Cut section shows grayish white firm circumscribed areas involving whole of the breast

Gross showing involvement of base of the specimen

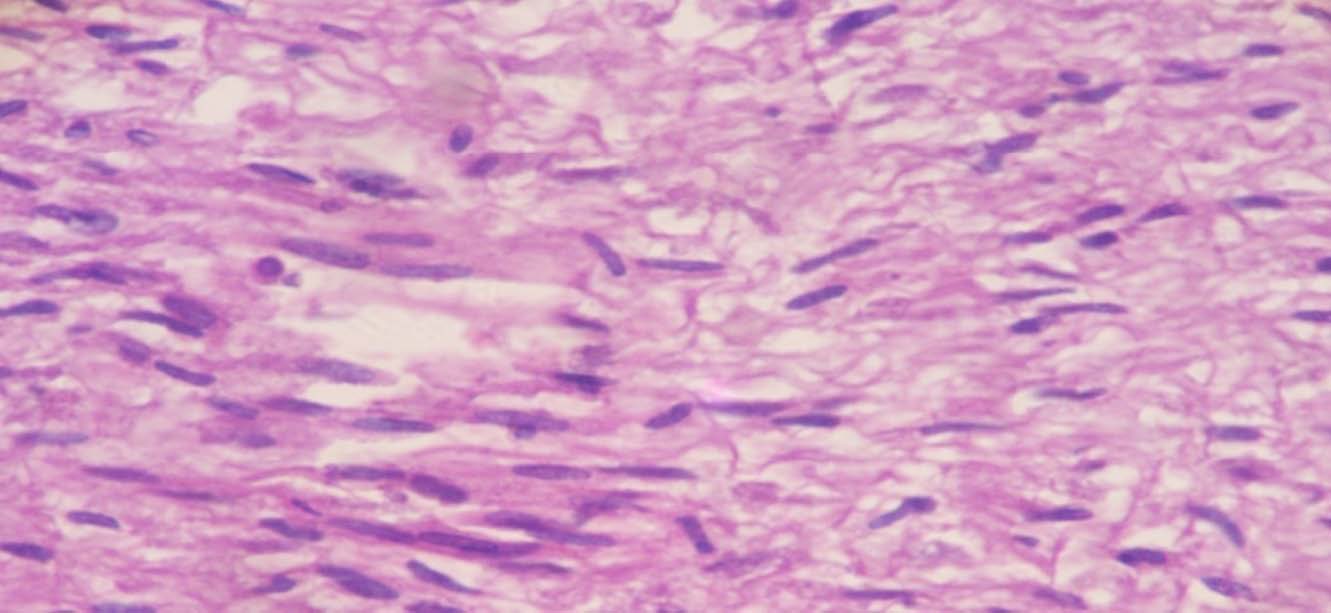
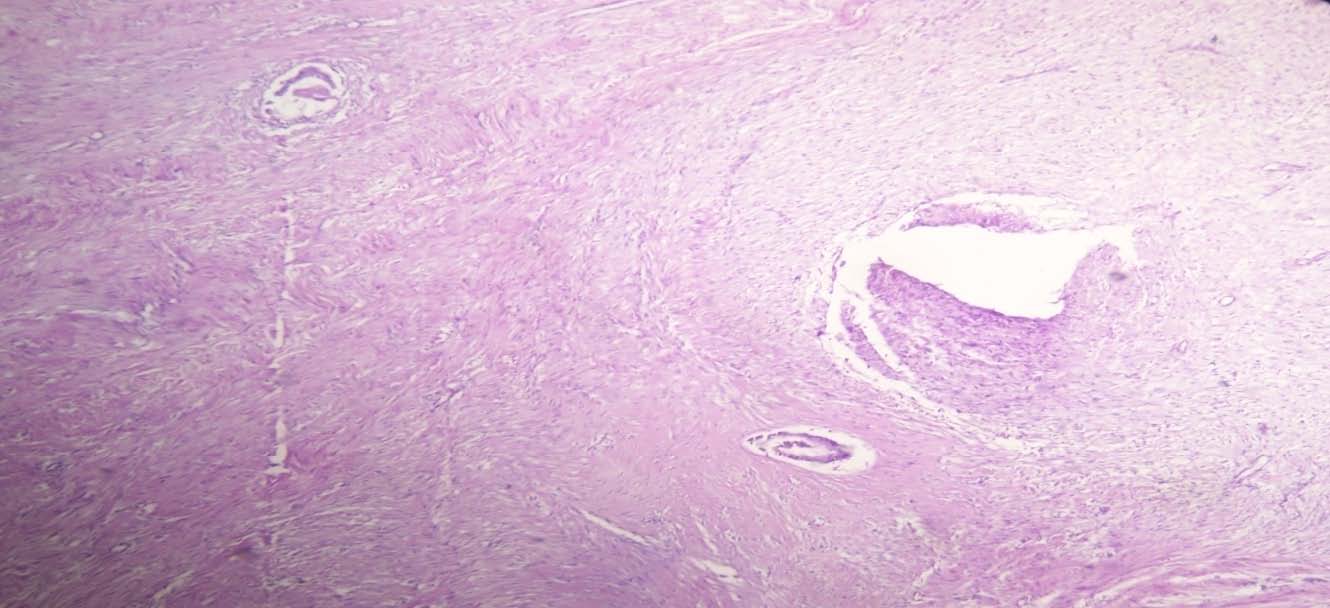
H&E stained sections showed uniform spindle shaped fibroblasts forming interlacing fascicles and at places arranged in storiform pattern [Table/Fig-3a] with mild to moderate amounts of collagen.The fibroblasts were well differentiated, uniform in size without hyperchromasia or pleomorphism [Table/Fig-3b]. Occasional mitotic figures were seen. Infiltration of fibroblasts into surrounding fat was present. Ductal and lobular structures were pushed towards periphery and were seen entrapped within fibroblastic proliferation [Table/Fig-3c]. Aggregates of lymphocytes and congested capillaries were present around the periphery of lesion. Thirteen lymph nodes resected from axillary tail showed features of reactive lymphadenitis. Based on histological findings, a diagnosis of infiltrative fibromatosis was made.
Sections show storiform spindle shaped fibroblasts forming interlacing fascicles and at places arranged in storiform pattern (H&E, x100)
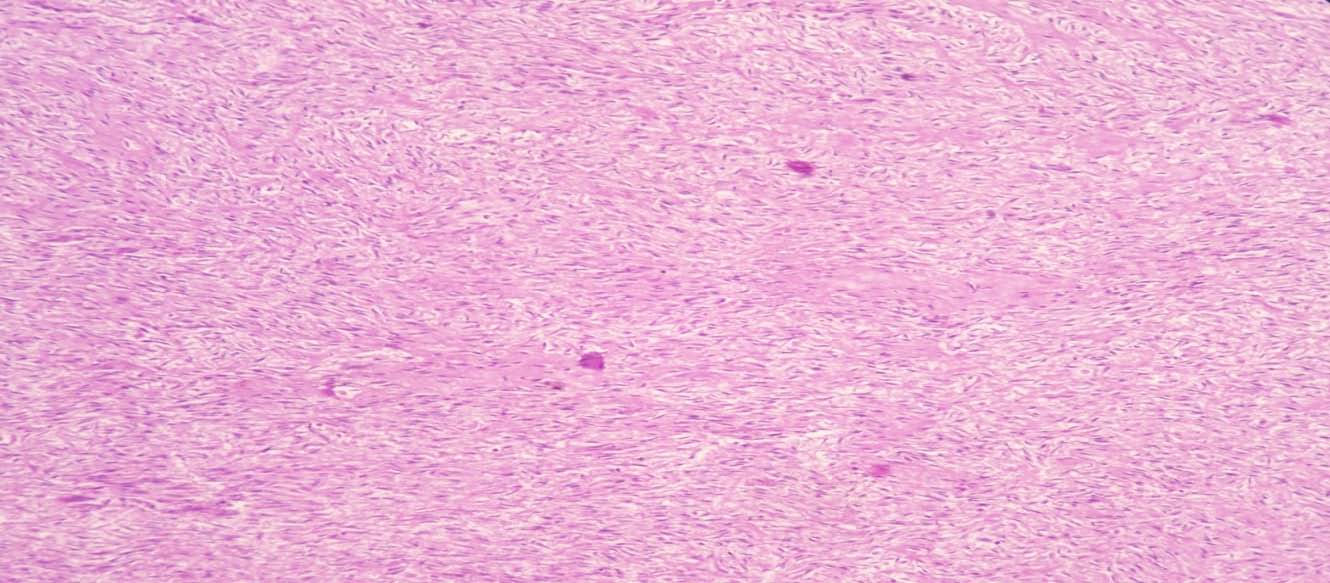
Section showing fibroblasts-uniform in size with no hyperchromasia or pleomorphism (H&E, x400)
Section showing occasional ducts entrapped within proliferating fibroblasts (H&E, x100)
Discussion
Mammary fibromatosis account for 0.2% of all breast tumors [1]. Usual age at presentation is 20-35 years [2]. Most of the cases are sporadic but 10-20% cases are associated with Familial Adenomatosis Polyposis and 30% have prior history of trauma [3]. or high estrogen state [4]. There was no family history or hormone intake except for previous surgical scar.
Mammary fibromatosis is difficult to diagnose as it mimics carcinoma clinically and radiologically. However cytology can be an early source of important information as it can rule out carcinoma. Cytological findings of mammary fibromatosis by various authors were reviewed. Tani et al., mentioned numerous stromal cells of fibroblastic type, without atypia, with a background of granular amorphous material and small fragments of collagen. Clusters of benign epithelial cells were occasionally observed [5]. Pettinato et al., also observed bland-appearing isolated spindle cells along with small groups of benign ductal cells and lymphocytes [6]. Zanella et al., revealed scant cellularity with oval and spindle cells having bland nuclei and occasional larger polygonal cells with high nuclear cytoplasmic ratio [7]. Roshini et al., described that bland spindle cells were haphazardly arranged in a collagenous matrix. The individual cells showed indistinct cytoplasmic borders and elongated nuclei with blunt or pointed ends having fine nuclear chromatin, no nucleoli, hyperchromasia, mitotic activity or pleomorphism. Ductal epithelial cells were conspicuously absent [8]. Our case also showed similar features consisting of fair number of scattered benign looking spindle to fusiform cells, some polyhedral myofibroblast like cells with cytoplasmic extension, occasional stromal fragments, occasional sheet of ductal epithelial cells and collagen matrix material.
Differential Diagnosis
Cytologically, fibromatosis should be differentiated from scar or keloid, nodular fasciitis, schwannoma, leiomyoma, solitary fibrous tumor (SFT), spindle cell lipoma, myofibroblastoma, myoepithelioma, low-grade fibromyxoid sarcoma and low grade fibrosarcoma.[9]. Presence of spindle cells admixed with epithelial cells should be differentiated from cellular fibroadenoma, phyllodes tumour or metaplastic spindle cell carcinoma.
Smears from scars are less cellular and more cohesive and are commonly associated with hemosiderin deposition, fat necrosis, foamy macrophages, and foreign body giant cells.
In nodular fascitis, smears are cellular with spindle shaped cells showing nuclear pleomorphism, myxoid background, ganglion-like cells and inflammatory cells. Intercellular collagen and history of recurrence as seen in fibromatosis; is not seen in nodular fascitis.
In schwannoma nuclei are comparatively longer and wavier. Smears of leiomyoma are paucicellular with blunted or cigar shaped nuclei, whereas those of fibromatosis have pointed, bipolar ends.
Spindle cell lipoma includes a mixture of mature adipocytes, uniform spindle cells and collagen bundles in varying proportion.
Myofibroblastoma shows spindle cells with nucleus having fine granular chromatin that may be divided by nuclear grooves, small inconspicuous nucleoli and eosinophilic cytoplasm in a background of collagenous fibrous tissue.
Myoepithelioma consists of monomorphic myoepithelial cells of spindle cell type. Binucleated cells and cells with pseudonucleoli can be found. There is a sparse collagenous stroma and/or mucoid ground substance.
Malignant tumours like low grade fibrosarcoma display increased cellularity, cytological atypia and mitosis. Low-grade fibromyxoid sarcoma has alternating myxoid and fibrous areas.
Hypercellularity of stromal fragments instead of scattered spindle cells and presence of atypia differentiate phyllodes tumor from fibromatosis. Tightly cohesive epithelial cells along with fibromyxoid stroma differentiate cellular fibroadenoma from fibromatosis.
Increased cellularity, nuclear pleomorphism, frequent mitosis are generally clues to the diagnosis of spindle cell carcinoma. A peculiar variant of spindle cell carcinoma called low grade fibromatosis-like carcinoma is composed of predominantly bland spindle cells closely resembling reactive fibroblasts as seen in fibromatosis. In such cases, IHC for cytokeratin is required to rule out carcinoma. In our case cytokeratin expression was negative hence low grade; fibromatosis-like carcinoma was ruled out.
Thus, careful observation of cytological findings, keeping in mind various other differentials along with a complete clinical history (recurrence in this case) can help reach a diagnosis and guard against an unnecessary drastic surgical approach; as a complete localized excision is all that is required.
[1]. Glazebrook KN, Reynolds CA, Mammary fibromatosisAJR Am J Roentgenol 2009 193(3):856-60. [Google Scholar]
[2]. Goel NB, Fibrous lesions of the breast: imaging-pathologic correlationRadiographics 2005 25(6):1547-59. [Google Scholar]
[3]. Schlemmer M, Desmoid tumors and deep fibromatosesHematol Oncol Clin North Am 2005 19(3):565-71. [Google Scholar]
[4]. Lewis JJ, The enigma of desmoid tumorsAnn Surg 1999 229(6):866-72. [Google Scholar]
[5]. Tani EM, Stanley MW, Skoog L, Fine needle aspiration cytology presentation of bilateral mammary fibromatosis. Report of a caseActa Cytol 1988 32(4):555-8. [Google Scholar]
[6]. Pettinato G, Manivel JC, Petrella G, Fine needle aspiration cytology, immunocytochemistry and electron microscopy of fibromatosis of the breast. Report of two casesActa Cytol 1991 35(4):403-8. [Google Scholar]
[7]. Zanella M, Falconieri G, Della Libera D, The Value of Fine Needle Aspiration Cytology in Breast Fibromatosis: Study of Two New Cases and Review of the LiteratureBreast J 1999 5(4):264-68. [Google Scholar]
[8]. Chinoy RF, Beotra A, Naresh KN, Fibromatosis of the breast: Diagnosis by fine needle aspiration cytologyActa Cytologica 1998 42(3) [Google Scholar]
[9]. Tanwar P, Gupta N, Vasishta RK, Singh G, Fine needle aspiration cytology in fibromatosisJ Cytol 2012 29(1):66-8. [Google Scholar]