Tuberculosis, a contagious bacterial disease which is caused by Mycobacterium tuberculosis, primarily involves the lungs.Though Pulmonary tuberculosis (PTB) is the commonest clinical presentation, there is a need for alertness towards uncommon presentations which involve other organs. Tuberculous otitis media (TOM) is one such rare presentation seen in paediatric practice. It is characterized by painless otorrhoea which fails to respond to the routine antibacterial treatment. TOM usually occurs secondary to PTB. Here is a case of tuberculous otitis media with Proteus mirabilis co-infection, with no evidence of PTB. In the sample of ear discharge obtained from the patient, acid fast bacilli were demonstrated on direct microscopy after Ziehl-Neelsen staining. Culture done on Lowenstein-Jensen medium demonstrated slow-growing Mycobacterium. Bacteriological culture and identification helped in isolating Proteus mirabilis. PCR, followed by Line- Probe Assay for early identification and susceptibility testing to primary drugs, was done. Further, patient tested negative for the Mantoux test. Patient was enrolled in National Tuberculosis programme- RNTCP. This case emphasizes on one of the less common presentations of a common disease. A high clinical suspicion and laboratory confirmation are required for appropriate patient management.
Case Report
A 6-year-old girl presented with a painless, purulent discharge from right ear, of 10 days duration, to the Out Patients Department (OPD) of Paediatrics, at a tertiary care hospital in Pune, in March 2013.It was associated with low grade fever of duration of 4-5 days and dry cough of duration of 3 days. She did not complain of loss of hearing and since past 5-6 months, she had recurrent otorrhoea from the same ear, which varied from a scanty to a profuse discharge. She was treated with antibiotics (both oral and ear drops) on OPD basis. As there was no clinical improvement, she was admitted for further investigations. Her immunization history was complete and all her milestones had been reached at appropriate ages. There was no history of tuberculosis in the family.
On examination, she was found to be apparently healthy. Submandibular and supraclavicular lymph nodes on right side were palpable, non-tender. Systemic examination revealed no abnormality. Otoscopy of right ear revealed thick purulent pus in the external auditory canal (EAC). On removal of pus, a pulsatile tympanic membrane (TM) with a single perforation and granulation tissue was noted. Left ear was full of wax, but it was otherwise normal.
Laboratory investigations revealed Hb to be 11.9 gm/dl; WBC-11,000, with 54% neutrophils, 41% lymphocytes 3% eosinophils and 2% monocytes. ESR was 10 mm of Hg. Serology for HIV and HBsAg was negative. C-reactive protein was positive. Mantoux test was negative. X-ray chest and mastoid region were insignificant.
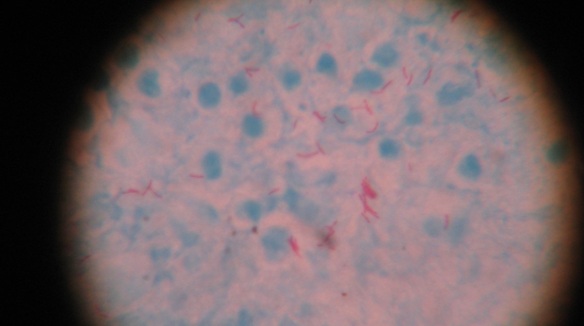
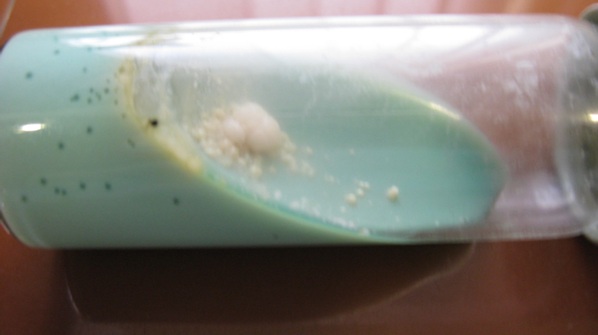
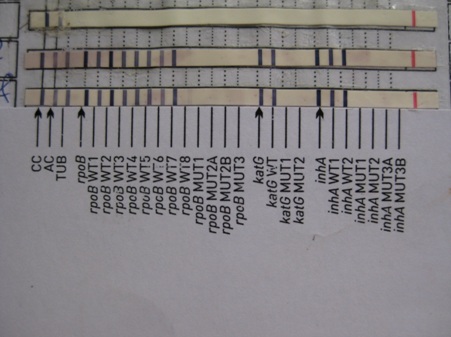
Microbiology: Specimen of EAC discharge was received for routine culture and sensitivity. Ziehl Neelsen (ZN) staining smear from ear discharge revealed beaded acid fast bacilli (AFB) [Table/Fig-1]. Repeat samples were obtained, which showed similar findings. Bacteriological and mycobacteriological cultures of the discharge were set up. Proteus mirabilis was isolated in bacteriological culture which was carried out on MacConkey’s and blood agar petri plates. Growth of AFB was observed on Lowenstein Jensen’s medium in 3rd week [Table/Fig-2]. Repeated sputum samples were negative for AFB microscopy and culture. A repeat sample which was collected, also gave the same result. PCR, followed by Line Probe Assay, was carried out for early identification and drug susceptibility. It was positive for M. tuberculosis complex, with Isoniazid sensitivity and Rifampicin resistance [Table/Fig-3]. Family members were screened for pulmonary and extra pulmonary tuberculosis (EPTB), both PTB and EPTB and they were found to be negative. She was registered under RNTCP for DOTS and managed with anti-tubercular drugs, as Category I. She responded well to the above therapy, with complete cessation of ear discharge.
Direct microscopy showing presence of Acid Fast Bacilli (ZN stain)
Growth on Lowenstein Jensen medium
Line probe assay of sample
Discussion
Tuberculosis mainly affects the lungs and lymph nodes. Involvement of the middle ear, which occurs usually secondary to pulmonary focus, is uncommon, with primary cases being extremely rare [1]. The incidence of Tuberculous Otitis Media (TOM) is difficult to assess, as most of the reported cases were from hospital subgroups [2,3]. 0.04% of all cases of chronic supportive otitis media in children could be TOM [4].
The presence of tubercle bacilli in an otitic discharge was first documented by Esche [5]. The incidence of TOM was quite high in the pre-antibiotic era, accounting for 2-8% of all cases of CSOM [6]. This incidence reduced with the advent of Anti-tubercular treatment and childhood immunization programmes. PTB (active or inactive) is present in 14-93% cases of TOM, but TOM is manifested in only 2% cases of active PTB [7]. The present report seemed to be a case of primary TOM, as she lacked evidence of tuberculosis infection at any other body site.
TOM is caused by M. tuberculosis, M. hominis and M. bovis. The pathogenesis involves (a) aspiration of mucus through the Eustachian tube (b) blood borne dissemination (c) direct implantation through EAC and TM perforation and (d) congenital transmission [5,8]. In children, the anatomy of the Eustachian tube permits an easy reflux of material into the middle ear cavity. This may be the reason for more common TOM cases being seen among children than among adults [2]. TOM is unilateral, although a possible route for spread of infection is pharyngotympanic tube, which is bilateral. Loss of hearing is variable and it may be conductive, sensori-neural or mixed deafness [7]. Multiple TM perforations are also observed, though they are rare. Nishike et al., reported that none of their patients had multiple perforations, facial nerve palsy or bone erosions [9].
The classical feature of TOM is painless otorrhoea which does not respond to antibiotics. TM perforations, abundant granulation tissue, bone necrosis and severe hearing loss are seen less and in the early stages, the TM is thickened and hyperaemic and its landmarks obliterated [10]. Otorrhoea, though it is painless, can sometimes be painful, due to formation of granulation tissue and secondary bacterial infections [5].
The present case presented with unilateral, painless recurrent otorrhoea of 5-6 months duration, which did not respond to antibiotics. Otoscopy done during a previous admission showed a dilated, pulsatile TM with granulation tissue. The otoscopic findings revealed a single perforation. There was no facial nerve palsy, bony involvement or hearing loss.
Culture of EAC discharge showed positivity for TB in 5-44 % cases and smear positivity in 0-20% cases [5]. A high rate of secondary bacterial infections (70%) may also prevent identification of tuberculosis on staining or culture. Secondary bacterial infections caused by Staphylococcus, PseudomonasKlebsiella, Proteus and Streptococcus spp. interfere with growth of M. tuberculosis, thus making diagnosis difficult and delayed [1,2]. In the present case, Proteus mirabilis was also isolated. Once diagnosed, response to drug treatment was excellent and surgical treatment was avoided. However, TOM, being a rare clinical presentation, is usually not considered in the initial differential diagnosis, thus causing missing out of chances of early case detection, until a severe damage to middle ear has occurred. Repeated specimens of ear discharge should be obtained for culture and demonstration of AFB, to confirm or rule out the possibility of TOM in chronic cases. Gene amplification techniques like PCR are very useful for early detection of cases and when cultures and smear give false negative results.
The Mantoux test is done to indicate an exposure of the immune system to Mycobacterium tuberculosis or to the BCG vaccine. A negative test is thought to rule out infection. However, false negative tests may occur in 20% of persons with active tuberculosis [11]. Further studies reveal false negative tests may occur in various conditions like milliary tuberculosis, protein malnutrition, reticuloendothelial disease and corticosteroid therapy. Such negative results have also been attributed to general illnesses and they become positive, 2-3 weeks after initiating treatment.In the present case, the negative Mantoux test could have been caused by the above reasons or it was probably a variant (delayed) tuberculin reactivity. In this, it has been seen that induration of less than 10 mm occurred at 48-72 hours,which became greater than 10 mm when read again at 6 days [11].
Anti -tubercular treatment is the treatment of choice for TOM. Cases are well managed with Category I antitubercular therapy. Surgery is done for functional reconstructions or to remove bony sequestrum and for treating complications [5]. However, for most of the cases of uncomplicated TOM, chemotherapy alone is sufficient. Sangeeta et al., reported management of 5 cases of TOM with ATT alone, with complete resolution of clinical symptoms [12]. Our patient showed a good clinician response with ATT alone, with complete cessation of ear discharge.
The present case highlights the occurrence of tuberculous otitis media. Secondary bacterial infections which are reported sooner, may mask the underlying cause if it is not looked for. This also brings out the fact that BCG vaccination, though it is highly recommended and useful, could still leave some populations vulnerable.
Conclusion
TOM must be strongly suspected in all cases of chronic otorrhoea which do not respond to antibiotics. Patients with known or suspected tuberculosis and chronic ear infections should also be screened for TOM. However, all cases of CSOM must be screened for AFB by staining and culture. Gene amplification techniques should be taken advantage of, if facilities are available. Keeping a high index of suspicion and a diligent search for evidence of tuberculosis by doing repeated sampling, are expected from clinicians. An early diagnosis and a prompt management will prevent middle ear damage and CNS complications.
[1]. Manigandan G, Venkatesh C, Gunasekaran D, Soundararajan P, Tuberculous Otitis Media and Staphylococcus aureus Co-infection in a five year old boy with military tuberculosisI J Glob Infect Dis 2013 5(1):26-8. [Google Scholar]
[2]. Windle-Taylor PC, Bailey CM, Tuberculous otitis media: a series of 22 patientsLaryngoscope 1980 90:1039-44. [Google Scholar]
[3]. Adhikari P, Tuberculous Otitis Media: A Review of LiteratureThe Internet J of Otorhinolaryngology 2009 9(1):10.5580/1b78 [Google Scholar]
[4]. Weiner GM, O Connell JE, Pahor AL, The role of surgery in tuberculosis mastoiditis: Appropriate chemotherapy is not always enoughJ Laryngol Otol 1977 111:752-3. [Google Scholar]
[5]. Aremu SK, Alabi BS, Tuberculous otitis media: a case presentation and review of the literatureBMJ Case Reports 2010 10:1136 [Google Scholar]
[6]. Turner AL, Eraser JS, Tuberculsis of the middle ear cleft in childrenJ Laryngol Otol 1915 30:209 [Google Scholar]
[7]. Arya M, Dixit R, Paramez AR, Sharma S, Rathore DS, Tuberculosis of the middle ear with post auricular abscessIndian J Tuberc 2009 56:160-3. [Google Scholar]
[8]. Kaushik M, Mishra P, Dehadaray A, Bansal A, Primary Tuberculous otitis with Cholesteatoma Revisited: Literature review with case reportBiological and Biomedical Reports 2012 2(2):94-8. [Google Scholar]
[9]. Nishiike S, Irifune M, Doi K, Osaki Y, Kiuchi N, Tuberculous otitis media: Clinical aspects of 12 casesAnn Otol Rhinol Laryngol 2003 12:935-8. [Google Scholar]
[10]. Verma SK, Mahajan V, Srivastava AN, Tuberculous otitis media with postaural abscess and submandibular lymphadenopathyLung India 2009 26(1):22-3. [Google Scholar]
[11]. Fitzgerald D, Haas DW, Mycobacterium TuberculosisPrinciples and Practice of Infectious Diseases by Mandell, Douglas and Bennet 2009 Seventh EditionPhiladelphiaPublishers Elsevier, Churchill and Livingston:2852-86. [Google Scholar]
[12]. Sangeeta V, Dinesh V, Kamal P, Divya P, Sudhir J, Tuberculous otitis media-are we missing it?Ind Jour of Otol and Head and Neck Surg 2000 52:143-6. [Google Scholar]