Transinguinal Preperitoneal Technique of Inguinal Hernioplasty – A Better Alternative to Lichtenstein Procedure
Rubik Ray1, Manoranjan Kar2, Mrityunjay Mukhopadhyay3
1 Senior Resident, Department of Surgical Gastroenterology, School of Digestive and Liver Diseases, IPGMER, Kolkata, India.
2 Professor, Department of General Surgery, Malda Medical College, Kolkata, India.
3 HOD, Department of General Surgery, College of Medicine and Sagar Dutta Hospital, Kolkata, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rubik Ray, 147 N.S. Road, Vivekananda Park, Narendrapur, Kolkata-700103, India.
Phone: 9804659199,
E-mail: rubikray@gmail.com
Introduction: The Lichtenstein technique is currently one of the popular methods in practice as it provides very good results consistently. However many patients suffer from wound indurations’ and chronic wound pain which are often underreported. The transinguinal preperitoneal technique (TPT) avoids these complications by placing the mesh in preperitoneal plane by open approach.
Materials and Methods: In this study, 71 patients were randomized into two groups one, of which one underwent the Lichtenstein repair and the other preperitoneal repair by TPT. All the patients were followed up for two years.
Results: Patients in TPT group had less pain in immediate post-operative period (p - .005), less wound induration and chronic pain on follow-up. Patients were also able to return to work early (p =0.036) . Average duration of operation was slightly longer compared to Lichtenstein technique (p < .0061) .There was no recurrence in either group on 2 year follow-up.
Conclusion: This study shows that TPT provides a better alternative to Lichtenstein technique with decreased incidence of wound complications and chronic groin pain, while having a similar recurrence rate. Preperitoneal mesh placement by open approach in TPT is also easier and eliminates the need for laparoscopy.
Hernia repair, Preperitoneal mesh, Lichtenstein complications
Introduction
Inguinal hernia repair is the second most common performed operation for a general surgeon [1]. In today’s scenario, the Lichtenstein technique has achieved marquee status as the procedure of choice for open repairs. It is a tensionless repair, easy to learn and perform, with very low recurrence rates [2]. However patients undergoing hernioplasty by Lichtenstein procedure can have wound complaints and chronic groin pain which is often underreported [3]. These problems can be avoided by placing the mesh in the preperitoneal plane by the transinguinal preperitoneal technique [TPT]. Preperitoneal repairs are usually performed by the laparoscopic approach but are generally restricted to bilateral and recurrent hernias. In addition, the laparoscopic approach is hampered by a long learning curve [4], increased cost and higher recurrence and complication rates. TPT avoids all these problems while retaining the benefits of preperitoneal mesh placement.
The aim of the present randomized controlled study was to compare the TPT to Lichtenstein procedure, in patients with unilateral inguinal hernia with respect to operative time , duration of hospital stay and return to work , as well as incidence of wound complications , chronic groin pain and hernia recurrence post-operatively.
Materials and Methods
The study was designed as a prospective comparative randomized controlled study including 71 patients undergoing open repair for unilateral inguinal hernia for a period of 30 months. Exclusion criteria: patients aged below 18 years, bilateral or recurrent hernias, undergoing emergency hernia repairs, and medically unfit for the operation. The study protocol was cleared with local institutional ethics committee. Informed consent was obtained from all patients. The patients were randomized into two groups, one the Lichtenstein group (Licht) (35 patients) and other the TPT (36 patients). The median follow-up was 2 year (range 6 month – 3 years). None of the patients was lost during follow-up during the study period.
The mean age of our patients was 48.3 years (range:22 years – 68 years). The types of hernias were indirect in 73% cases, direct – 24% and combined variety - 3 % [Table/Fig-1].
| TPT | Lichtenstein |
|---|
| Number of patients | 36 | 35 |
| Sex | All Male | All Male |
| Age |
| 18-40 years | 6 | 5 |
| 41-60 years | 23 | 24 |
| > 60 years | 7 | 6 |
| Types of Hernia |
| Indirect | 25 | 27 |
| Direct | 10 | 7 |
| Pantaloon | 1 | 1 |
| Comorbidities |
| Hypertension | 9 | 6 |
| Diabetes | 3 | 3 |
| COPD | 3 | 2 |
| Prostatism | 1 | 1 |
| Smoking | 5 | 6 |
| Constipation | 2 | 2 |
Technique
Both the groups were operated under spinal anaesthesia. Lichtenstein repair was done according to established techniques as per standard protocols and precautions. In case of TPT, patients were catheterised pre-operatively, to prevent any injury to the bladder and aid in preperitoneal dissection. The catheter was removed after 48 hours post-operatively.
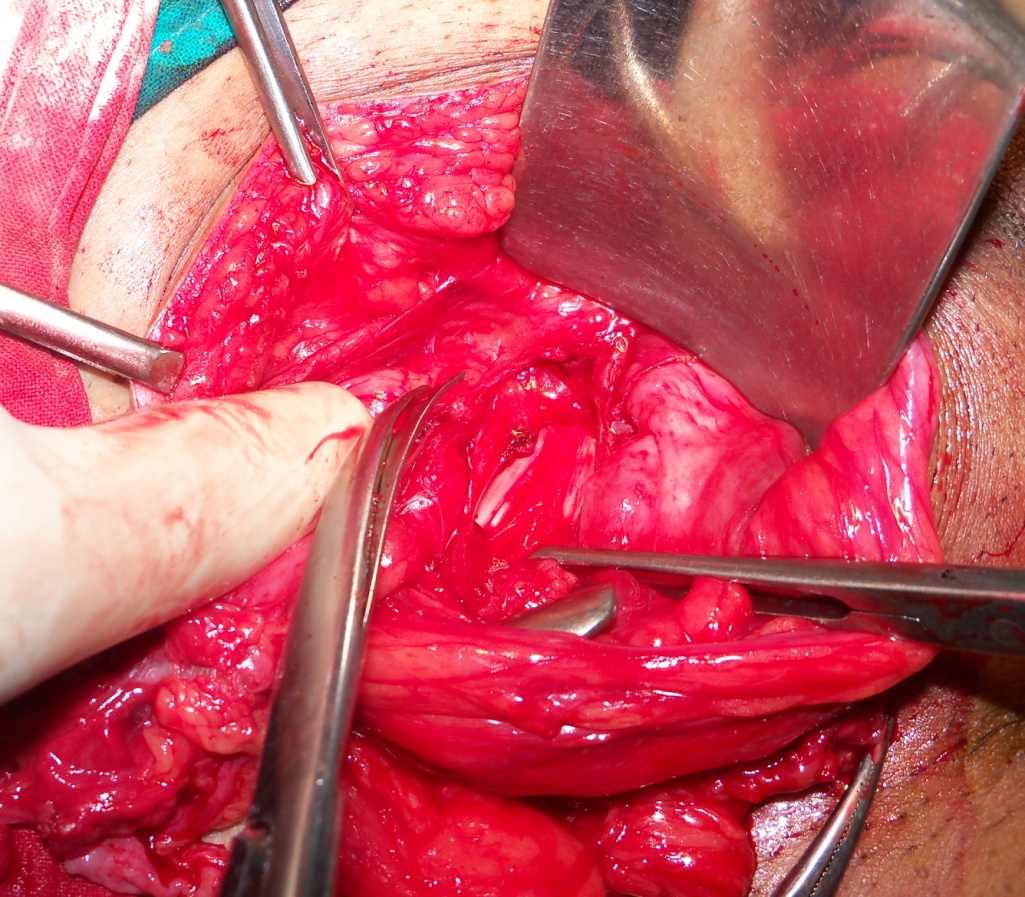
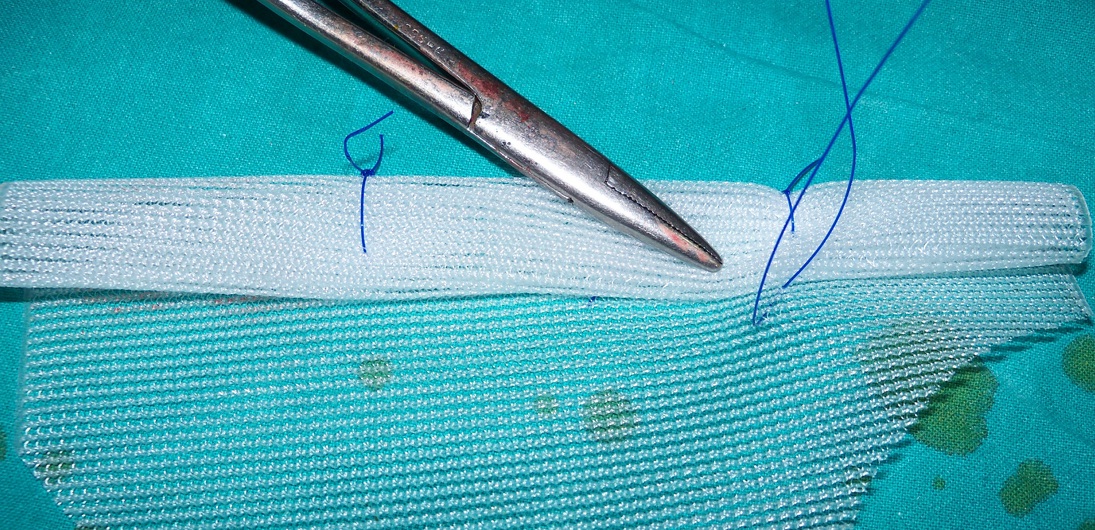
Incision of TPT is same as that of Lichtenstein technique [5]. After dissection of the sac, the transversalis is fascia is incised [Table/Fig-2] to enter the preperitoneal space. The preperitoneal space is developed by dissection with index finger [Table/Fig-3]. The space extends from rectus muscle medially, arcuate line cranially, a little beyond the anterior superior iliac spine over the psoas muscle laterally [Table/Fig-4] and the lilipubic tract caudally. A 15 cm x 15 cm polypropylene mesh, cut into dimension 15 cm x 12 cm, the inferior medial angle of the mesh is trimmed in a semicircular fashion [Table/Fig-5] to prevent trauma to the bladder neck. The mesh is placed in the preperitoneal space and anchored to the Cooper’s ligament with a single 2-0 interrupted prolene suture [Table/Fig-6,7and8].
Incision of Fascia Tranversalis to Enter into Preperitoneal Space
Index finger in preperitoneal plane dissection
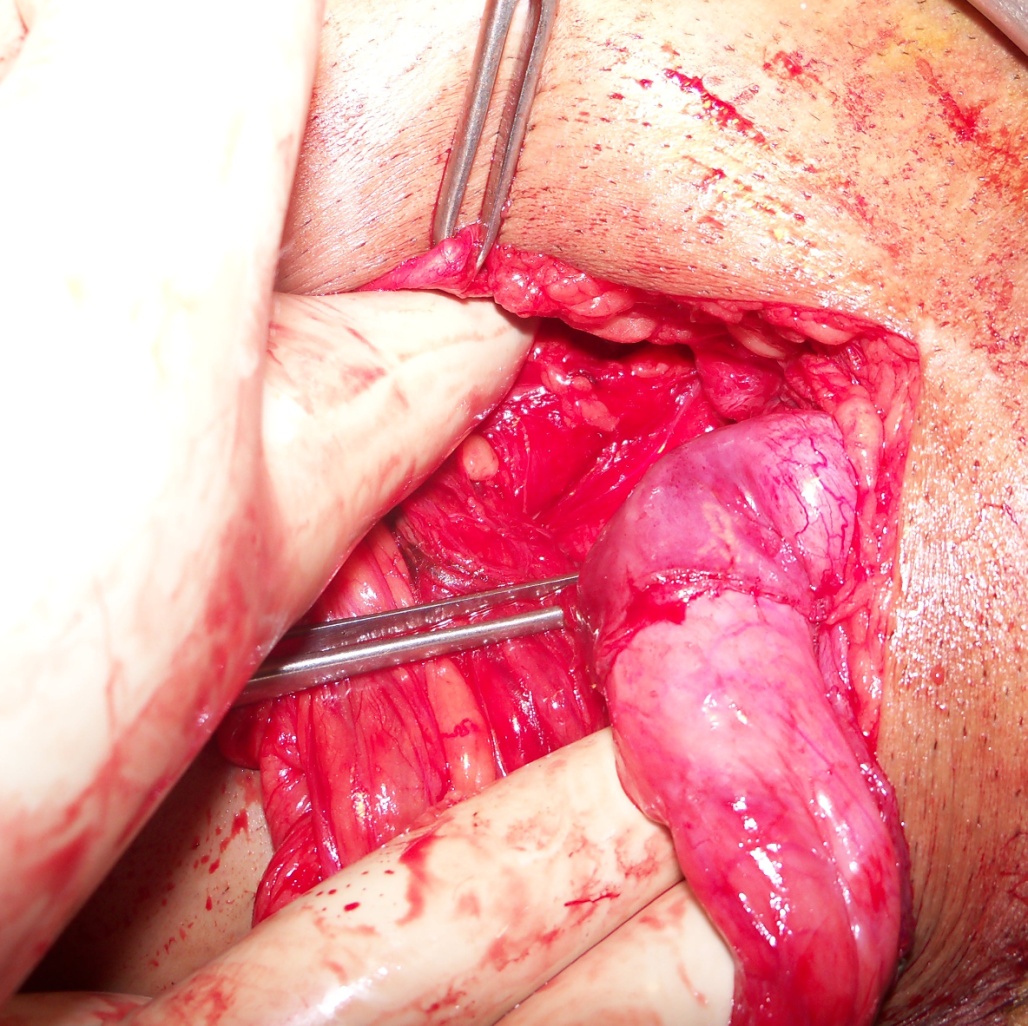
Lateral limit of dissection –the anterior superior iliac spine

Mesh rolled up and fixed with prolene suture
Mesh being inserted into the preperitoneal space
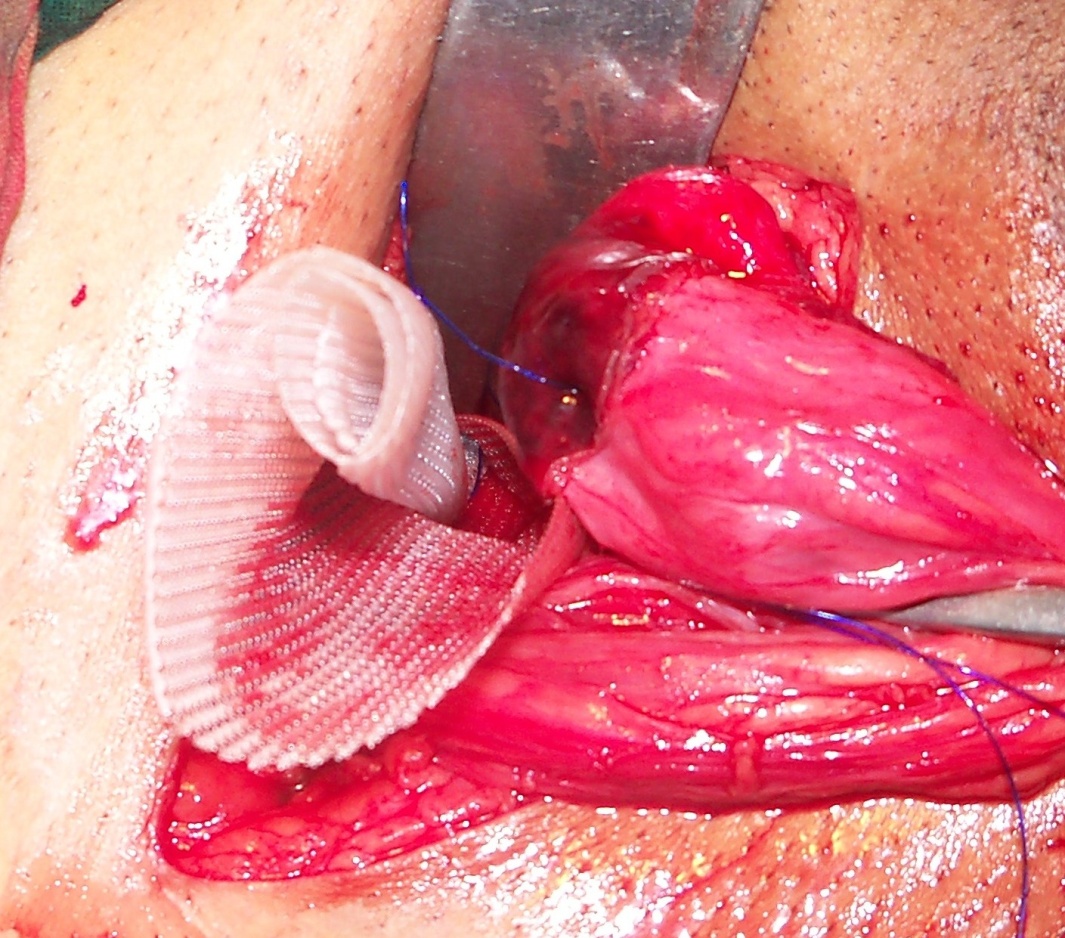
Mesh spreading with hemostatic forceps

Appearance after 1 month of surgery

Results
A total of 71 patients were studied, TPT group- 50.7% and Licht group - 49.3% patients respectively. The duration of operation was more in the TPT group and this was statistically significant. (p < .0061) On assessment of post-operative pain, significant difference of pain observed at 12 hours (p = 0.005) which was more in Lichtenstein repair while no significant difference was found after 24, 48 and 72 hrs and at discharge. The duration of hospital stay was found to be similar in both the groups. Return to sedentary work was earlier in the TPT group and it was found to be statistically significant (p =0.036) [Table/Fig-9]. Complications encountered are tabulated below [Table/Fig-10].
| TPT | Lichtenstein |
|---|
| Duration of Operation | 49.5 ±11.5 minutes | 37.9 ± 13.7 minutes |
| Hospital stay | 4.6 ±1.23 days | 4.65 ± 1.39 days |
| Return to Sedentary Work | 12.3 ± 2.01 days | 13.6 ± 1.6 days |
| Complications | TPT | Lichtenstein |
|---|
| Per-operative |
| Injury to peritoneum | 3(8.5%) | Nil |
| Injury to Vessels | 1(2.7%) | Nil |
| Immediate post-operative |
| Wound seroma | Nil | 2(5.7%) |
| Scrotal collection | 1(2.7%) | 1(2.7%) |
| At 1 month |
| Wound Induration | Nil | 6(17.14%) |
| Scrotal collection | 1 | 1 |
| Chronic Pain | Nil | 3 |
| Recurrence | Nil | Nil |
| At 6 months |
| Chronic pain | Nil | 1 |
| Scrotal collection | Nil | Nil |
| Wound induration | 1 | 3 |
| Recurrence | Nil | Nil |
| At 1 year |
| Chronic pain | Nil | Nil |
| Wound induration | Nil | Nil |
| Recurrence | Nil | Nil |
Peritoneal breach and injury to inferior epigastric vessels or the corona mortis was more in TPT group. Wound seroma (5.7%), wound induration (17.14%) were more in the Licht group. 8.6% of patients in Lichtenstein group had chronic pain in early follow-up which caused sufficient alarm to the patients and which persisted in 2.8% of patients on long term causing significant alteration in the patient’s normal lifestyle. There was no recurrence in either of the groups during the course of the study. Maximum follow-up for some patients were up to 3 years but there were no recurrences in either of the groups till date.
Discussion
The Lichtenstein technique is one of the popular methods of inguinal hernioplasty as it is easy to learn and perform, and gives consistent good results with less than 1% recurrence rates [6]. However placement of the mesh in the inguinal canal has some demerits. Patients in our Lichtenstein group had increased incidence of wound and scrotal collection in the immediate post-operative period, as well as wound induration and chronic pain in long term follow-up. Polypropylene mesh can cause light microscopic and ultra structural changes in the peripheral nerve due to myelin degeneration, endoneurial and perineurial edema, fibrosis, axonal loss [7], and can cause chronic groin pain by entrapment of the nerve in scar tissue. Wound seroma and induration can be caused by foreign body reaction to mesh [8,9]. Chronic pain and wound complaints delays recovery and can significantly affect a patient’s daily lifestyle [3]. All these complications are avoided by placing the mesh in the preperitoneal plane by TPT. In addition , by placing a mesh in the preperitoneal space, the myopectineal orifice is covered completely which not only is the optimal treatment for indirect, direct, femoral and obturator hernias but also protects against any of these hernias from recurrence. Patients in the Licht group also had delayed return to work. This was mostly due to the chronic wound related problems. These problems were virtually absent in the TPT group.
These advantages of preperitoneal repair are well demonstrated by the totally extraperitoneal (TEP) or by the transabdominal preperitoneal (TAPP) methods of inguinal hernia repair [6,10]. However, laparoscopic methods have their unique set of complications as well as having a difficult and prolonged learning curve [1,11], and the need of general anaesthesia during the procedure [3]. The transinguinal preperitoneal technique can be considered more analogous to the totally extra peritoneal repair. But compared to the totally extra peritoneal repair this technique is not expensive, easier to perform and can be performed under regional anaesthesia. It can be applied to all types of primary inguinal hernia.
In TPT the average operating time is slightly longer than the Lichtenstein procedure which can be attributed to preperitoneal dissection as well as proper placement of the mesh. Complications like peritoneal breach are easily avoided by meticulous technique. Large tears should be repaired with a few stitches of absorbable suture as it helps in proper mesh placement. Placing the mesh could pose some difficulty since the total dissected area cannot be visualised directly and can only be felt with the fingertips. The mesh also needs to be folded similar to laparoscopic techniques to introduce it into the preperitoneal space through the defect in the fascia transversalis. While fixing the mesh to the Coopers ligament care should be taken so as not to injure the corona mortis, or troublesome bleeding may result.
Limitations of this study include a smaller sample size as well as incomplete follow-up on long term. All patients were followed up for a median time period of 2 year (range: 6 months – 3years). There were no cases of recurrence in either group of patients. However long terms follow-up is needed in these patients to document the true incidence of recurrence in these groups.
Conclusion
In conclusion, this study shows that the TPT provides significant advantages over the Lichtenstein technique in case of repair of unilateral inguinal hernias. Patients in TPT group had less incidence of wound induration and chronic groin pain. They were also able to return to their jobs earlier. Though the average operating time was slightly increased, the duration of hospital stay was same compared to the Lichtenstein group. On 2 years follow-up TPT did not have any recurrence. Therefore the transinguinal preperitoneal technique offers a better alternative to Lichtenstein technique for open repair of unilateral inguinal hernias and should be recommended wherever indications or scope of laparoscopy does not exist.
[1]. Alexandre JH, Bouillot JL, Dupin P, Aouad K, Bethoux JP, Cure of inguinal hernias with large preperitoneal prosthesis: Experience of 2,312 casesJ Minim Access Surg 2006 2(3):134-8. [Google Scholar]
[2]. Nordin P, Bartelmess P, Jansson C, Svesson C, Edlund G, Randomized trial of Lichtenstein versus Shouldice hernia repair in general surgical practiceBr. J. Surg 2002 89:45-9. [Google Scholar]
[3]. Koning GG, Koole D, de Jongh MA C, de Schipper JP, Verhofstad MHJ, Oostvogel H J M, The transinguinal preperitoneal hernia correction Vs Lichtenstein technique; is TIPP top?Hernia 2011 15(1):19-22. [Google Scholar]
[4]. Karatepe O, Acet E, Altiok M, Adas G, Cakir A, Karahan S, Preperitoneal Repair (open posterior approach) for recurrent inguinal hernias previously treated with Lichtenstein tension-free hernioplastyHippokratia 2010 14(2):119-21. [Google Scholar]
[5]. Zollinger Robert Jr, Ellison E, Repair of Inguinal Hernia with Mesh (Lichtenstein)In:Zollinger’s Atlas of Surgical Operations 2010 9th EditionThe McGraw Hill Companies Inc:458 [Google Scholar]
[6]. Vironen J, Nieminen J, Eklund A, Randomized clinical trial of Lichtenstein patch or Prolene Hernia System for inguinal hernia repairBr J Surg 2006 93:33-9. [Google Scholar]
[7]. Demirer Seher, Kepenekci Ilknur, Evirgen O, Birsen O, Tuzuner A, Karahuseyinoglu S, The Effect of Polypropylene Mesh on Ilioinguinal Nerve in Open Mesh Repair of Groin HerniaJ. Surg Research 2006 13(2):175-81. [Google Scholar]
[8]. Robert Bendavid Abdominal wall hernias: principles and management. Springer. 2001 pg 722 [Google Scholar]
[9]. Gilbert AI, Felton LL, Infection in inguinal hernia repair considering biomaterials and antibioticsSurg Gynecol Obstet 1993 177:126 [Google Scholar]
[10]. Collaboration EH, Laparoscopic compared with open methods of groin hernia repair: systematic review of randomized controlled trialsBr J Surg 2000 87:860 [Google Scholar]
[11]. Palanivelu C, Laparoscopic Transabdominal Preperitoneal HernioplastyIN. Palanivelu C,ed.Text book of Surgical Laparoscopy 2002 CoimbatoreGem Digestive Diseases Foundation:227-36. [Google Scholar]