A Case of Perianal and Gluteal Scrofuloderma
Rajesh Kumar Reddy1, Shankar Ram H.S.2, Ashwin Pai3
1 Resident, Department of Surgery, KMC Mangalore, Kasturba Medical College, Manipal University, Mangalore, Karnataka, India.
2 Resident, Department of Surgery, KMC Mangalore, Kasturba Medical College, Manipal University, Mangalore, Karnataka, India.
3 Resident, Department of Surgery, KMC Mangalore, Kasturba Medical College, Manipal University, Mangalore, Karnataka, India.
4 Resident, Department of Surgery, KMC Mangalore, Kasturba Medical College, Manipal University, Mangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rajesh Kumar Reddy, Kasturba Medical College, Mangalore-575001, Karnataka, India.
Phone: 919686544500,
E-mail: rajesh.adapala@gmail.com
A 47-year-old male presented with multiple perianal and gluteal pus discharging sinuses. On examination, undermined sinus edges, thick and hyperpigmented surrounding skin, sacral tenderness and a lax anal sphincter were noted. Based on clinical, radiological and histopathological evaluations, patient was diagnosed to have sacral tuberculosis with perianal and gluteal scrofuloderma and he was started on anti-tuberculosis treatment.
Scrofuloderma, Gluteal, Perianal
Case
A 47-year-old male presented with multiple pus discharging sinuses in perianal and gluteal regions, which had begun as a small nodule 3 months ago. A history of low grade fever, loss of appetite and significant loss of weight was present. He also gave a history of low back ache and faecal incontinence. There was no history of any voiding difficulty. There was no past history of pulmonary or extra-pulmonary tuberculosis.
On examination, patient was found to be moderately built and poorly nourished. Local examination showed multiple discharging sinuses over gluteal and perianal regions and upper thighs, as has been shown in [Table/Fig-1,2and3]. Discharge was thick, purulent and without any bony spicules or granules. Sinuses could be probed upto not more than 1 cm. The edges of sinus tracts were undermined and surrounding skin was folded, with thickening and hyperpigmentation. Anal sphincter tone was reduced. Diffuse spinal tenderness was noted over lower lumbar and sacral regions.
Scrofuloderma of the Gluteal region with extensive involvement of perianal region

Multiple discharging sinuses over the groin

Scrofuloderma of the Thigh

On evaluation, patient was found to be HBsAg positive, with Hb-7.3gm/dl, TLC -16 810/cu.mm, ESR-40 mm/hour. HIV and Mantoux tests were negative. Liver and renal functions were within normal limits.
On radiological evaluation, chest X-ray did not show any features of pulmonary tuberculosis. CECT of lumbo-sacral spine which was done, showed destruction of spinous tubercles at S3, S4 and S5 levels, with adjacent minimally enhancing soft tissue.
Discharge obtained from the sinuses was sent for a microbiological evaluation. Staining for AFB (Acid fast bacilli) was negative. AFB culture showed no growth. No fungal elements and no sulphur granules were detected on KOH mount. Sputum AFB was also negative.
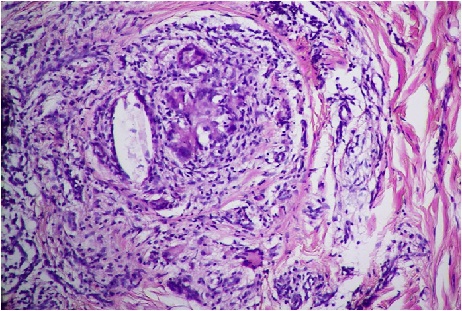
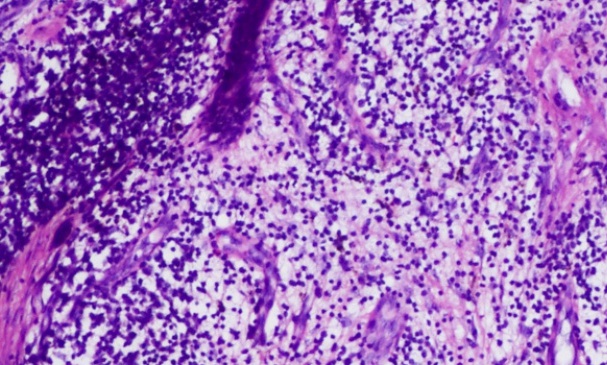
Histopathological examination of sinus tract biopsy showed granulomas in deep dermis, with Langhans giant cells, epitheliod cells and histiocytes, which were suggestive of scrofuloderma, as has been shown in [Table/Fig-4,5].
Sacral destruction evident on X-ray Lumbosacral spine. A Barium enema study of the same patient was normal

Microscopic view showing the typical granuloma formation
Chronic inflammatory infiltrate in the Dermis
Patient was started on anti-tuberculosis therapy (ATT) (including Streptomycin, for initial 2 months), along with nutritional supplementation. On follow-up examination which was done after 2 months, patient’s general condition was found to be improved, discharge from sinuses had drastically reduced and most of the sinuses were obliterated, as has been shown in [Table/Fig-1]. However, faecal incontinence and pigmentation persisted. Patient was advised to continue with ATT for 1 year.
Discussion
Scrofuloderma or “Tuberculosis cutis colliquativa” is a tuberculous or non-tuberculous mycobacterial involvement of the skin which occurs by direct extension from underlying structures like lymph node, bone or lung. It occurs most commonly in parotid, submandibular and supraclavicular regions. It first presents as a firm subcutaneous nodule and then it enlarges to form an abscess, followed by formation of multiple sinuses [1]. M.tuberculosis is the most common aetiological agent of Scrofuloderma with recovery of AFB which varies from 9.5 to 50 percent . M.scrofulaceum and M.avium complexes from skin lesions are isolated in immunocompromised patients [2].
The lumbo-sacral area is affected in less than 5% cases of spinal tuberculosis. Isolated sacral TB is extremely rare, but it should be suspected in patients who present with chronic low backache or in children with muscle spasms and discharging sinuses/abscesses which show sacral destruction on CT or MR imaging [3]. Our patient was a rare and interesting case of sacral tuberculosis with gluteal and perianal scrofuloderma.
[1]. Ermertcan AT, Öztürk F, Gençolan G, Nanir I, Özkütük N, Temiz P, Pott’s disease with scrofuloderma and psoas abscess misdiagnosed and treated as hidradenitis suppurativaJ Dermatolog Treat. 2011 22(1):52-4. [Google Scholar]
[2]. Gopinathan R, Pandit D, Joshi J, Jerajani H, Mathur M, Clinical and morphological variants of cutaneous tuberculosis and its relation to mycobacterium speciesIndian J Med Microbiol 2001 19:193-6. [Google Scholar]
[3]. Kumar A, Varshney MK, Trikha V, Unusual presentation of Isolated Sacral TuberculosisJoint Bone Spine 2006 73:751-2. [Google Scholar]