Diastematomyelia – A Report of Two Cases
Sushil G. Kachewar1, Smita B. Sankaye2
1 Professor, Department of Radio Diagnosis, Rural Medical College (RMC), PIMS, Loni, Uttar Pradesh, India.
2 Assistant Professor, Department of Pathology, Rural Medical College (RMC), PIMS, Loni, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sushil Kachewar, Professor, Department of Radio-Diagnosis, Rural Medical College, PIMS, At Post-Loni, Ta-Rahata, Dt-Ahmednagar, Maharashtra-413736, India.
Phone: 9921160357,
E-mail: sushilkachewar@hotmail.com
Diastematomyelia means sagittal division of the spinal cord into two hemi cords. It is a congenital malformation which results from an abnormal adhesion between ectoderm and endoderm. It is more common in females (3:1).
This abnormal adhesion which splits the cord may be in the form of fibrous tissue or purely a calcific bar or purely an ossific bar or even a combination of the earlier mentioned entities.
The health impacts of this entity are enormous, as the patients may be asymptomatic to begin with, until gradually; progressive spinal cord dysfunction sets in. Imaging plays a vital role in establishing the diagnosis and it may aid in easing the quality of life by making an early diagnosis.
The affected individual and the afflicted families need psycho-social guidance and counselling. We are presenting here, imaging findings in two cases of diastematomyelia.
Diastematomyelia, Imaging, Radiology, MRI, X-Ray, Ultrasound
Introduction
Case Studies
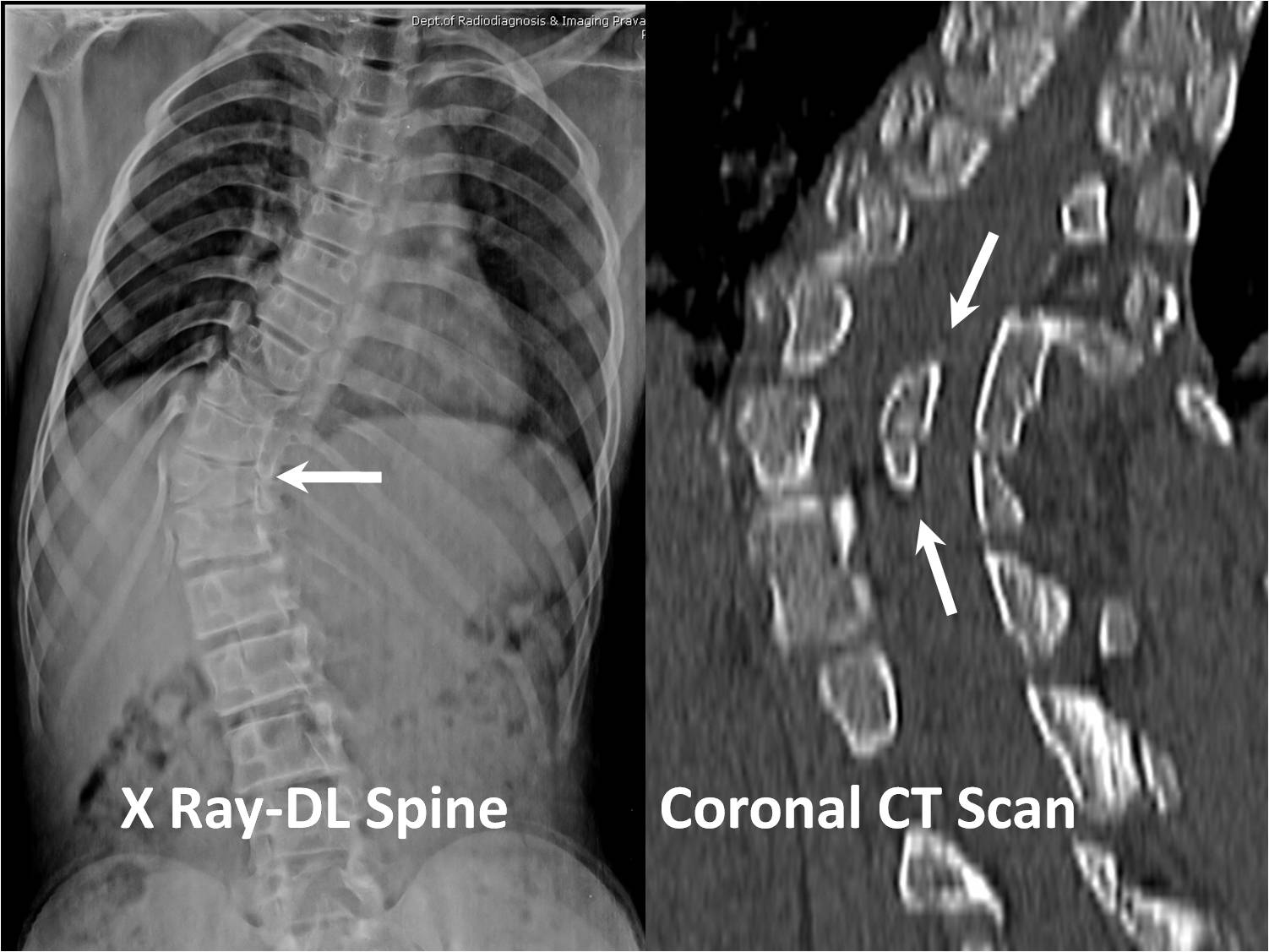
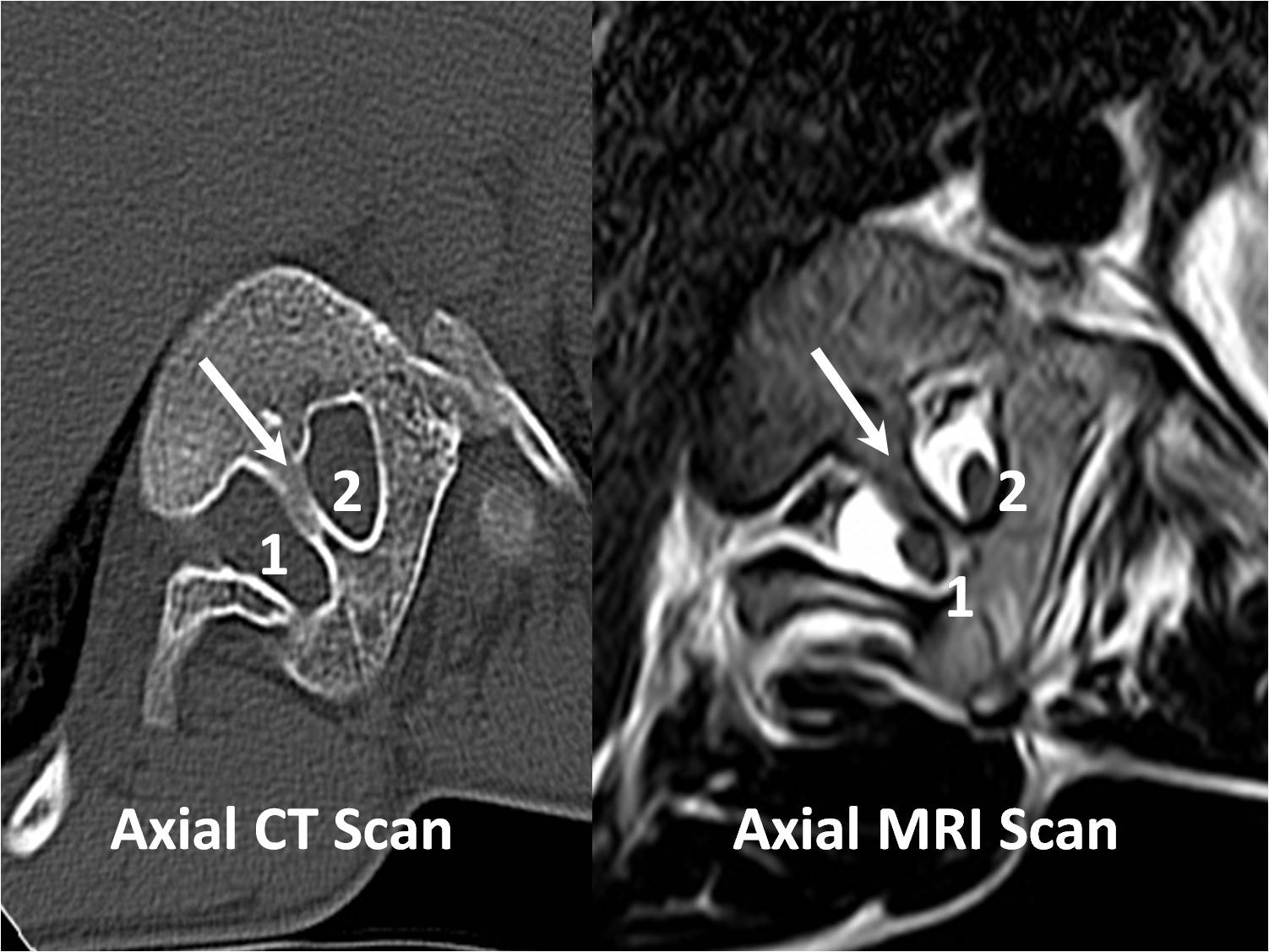
A 17-year-old male presented with history of decreased sensation in the lower half of body and loss of bladder and bowel control. Clinically, he had paraparesis involving both the lower limbs. He was referred for a complete imaging evaluation. As has been shown in [Table/Fig-1]; Antero-posterior X-ray of his dorso-lumbar spine and Coronal CT scan image showed a calcified bar splitting the spinal cord into two. As has been demonstrated in [Table/Fig-2]; Axial CT and Axial MRI images showed calcified bar splitting the spinal cord into two. Thus, a diagnosis of Diastematomyelia was made.
X-ray Spine and Coronal CT image showing calcified bar splitting the spinal cord
Axial CT and Axial MRI showing calcified bar splitting the spinal cord into two
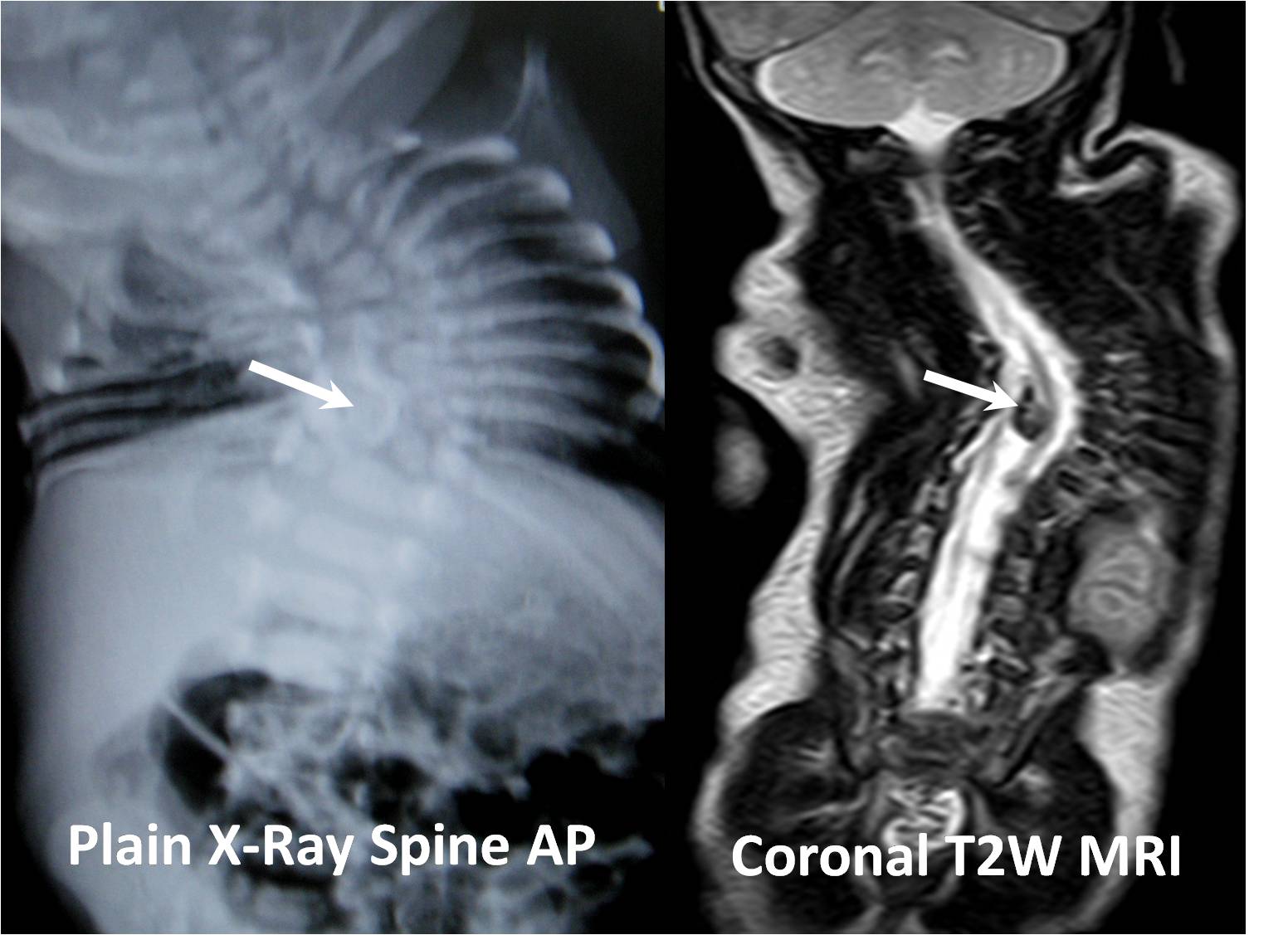
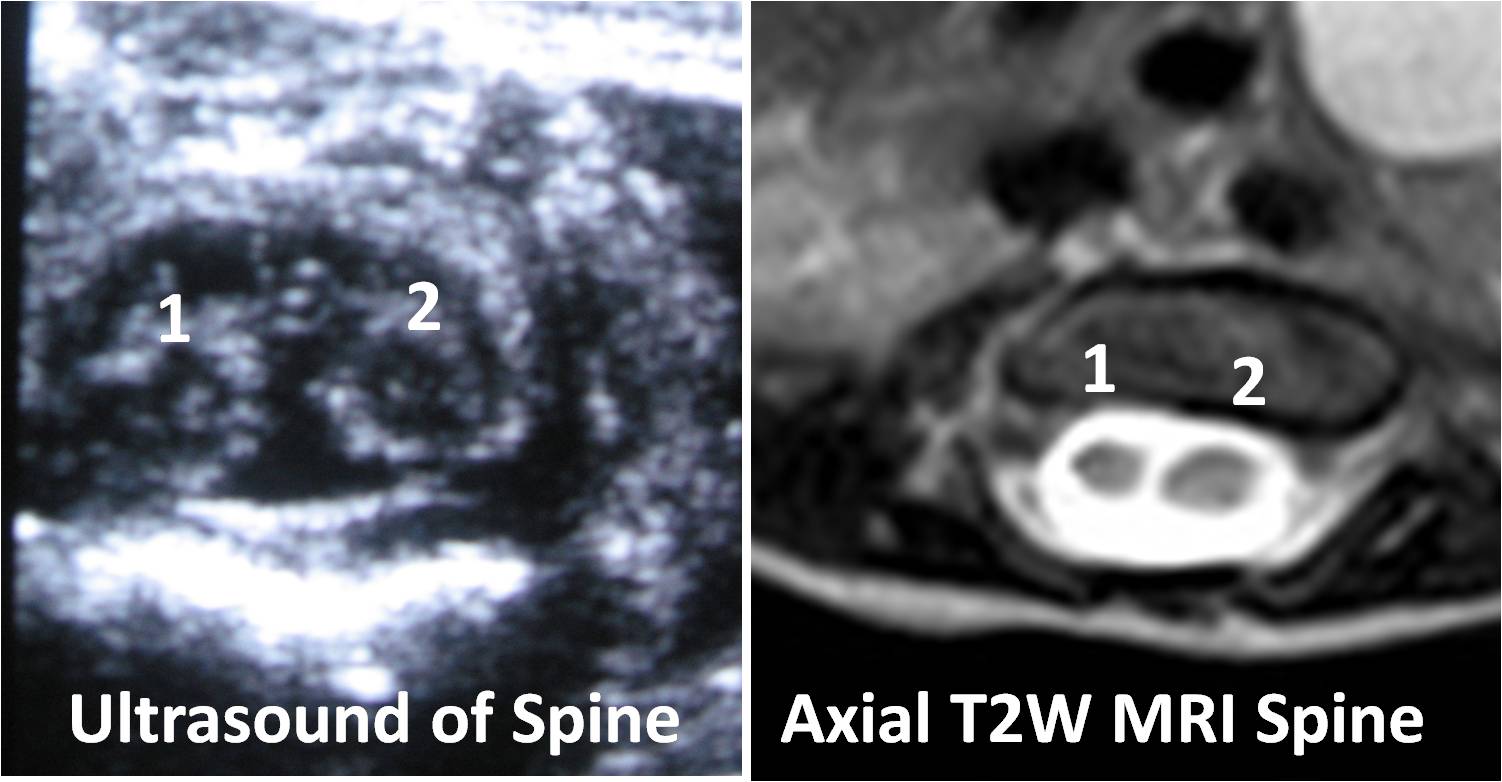
In another case, a one year child was brought with a suspected spinal deformity, as the child always remained turned on one side. No bladder or bowel abnormalities were noticed. Plain radiograph of spine and Coronal T2W MRI image [Table/Fig-3] showed a bony bar splitting the cord into two. Same findings were confirmed on high resolution ultrasound as well as T2W axial MRI image [Table/Fig-4].
X –ray Spine and Coronal MRI showing bony bar splitting the spinal cord into two
Ultrasound and Axial MRI showing bony bar splitting the spinal cord into two
Discussion
Diastematomyelia is a rare congenital spinal cord abnormality characterized by longitudinal “splitting up” of the spinal cord into two. Females are affected much more commonly than males. Usually, an osseous (bone), cartilaginous or fibrous septum in the central portion of the spinal canal produces a complete or incomplete sagittal division of the spinal cord into two hemi cords. Diplomyelia, or true duplication of the spinal cord is said to occur, when the split does not reunite distally to the spur. In this spinal dysraphism, the sagittal cleft may extend in the spinal cord, conus medullaris or even filum terminale and cause splaying of the posterior vertebral elements [1]. This entity may be isolated or associated with other segmental anomalies of the vertebral bodies [2]. It is now believed that an accessory neurenteric canal initiates this dysraphic state of unknown embryogenesis, as is evidenced by the narrowing of a disc space at the same level and interlaminar fusion. In most of the cases, the dividing bar is cartilaginous or fibrous or even bony [3]. Other anomalies of the vertebral column, such as spina bifida, kypho-scoliosis, butterfly vertebra and hemivertebra are also known to be associated with this condition [4].
Diastematomyelia usually occurs between D9 and S1 levels [5,6]. Cervical diastematomyelia is a very rare entity [7,8]. In about 50% of patients, the hemi-cords are contained in a single dural sac, while in the remaining, they lie within separate dural sacs. In the latter, bony or fibrous spurs are usually found between the two sacs [9]. Intramedullary tumours associated with diastematomyelia have been rarely described [10] and associated conditions like a tethered cord, inclusion dermoid, lipoma, syringohydromyelia and Chiari malformation have also been described in literature [11,12].
Prenatal ultrasound diagnosis of this anomaly is usually possible in the early mid third-trimester. An extra posterior echogenic focus between the foetal spinal laminae is seen with splaying of the posterior elements, thus allowing an early surgical intervention and a favourable prognosis [2,13].
Other conditions, which are sometimes associated with diastematomyelia (myelodysplasia, dysraphia of the spinal cord etc), may be the primary cause of progressive neurological lesions [13].
Bony malformations and dysplasias are generally recognized on plain radiographs [Table/Fig-1,3] and if they are clinically indicated, they can be further elucidated by CT [Table/Fig-2] along with demonstration of spinal abnormalities. However, MRI [Table/Fig-2,4] will generally allow adequate analysis of the spinal deformities and it is the technique of choice for dysraphism which requires full elucidation [3].
Prior to the universal availability of MRI scan, metrizamide myelography, and computed tomographic metrizamide myelography were used to add a new dimension to the diagnosis of dysraphic lesions of the spine [14–16].
The Health Impacts
The impact of diastematomyelia upon the quality of life (QoL) is almost similar, if not more, as of other chronic neurological diseases like quadriplegia and epilepsy. Usually, the patients become dependent and they need help for activities of daily living. The presence of a depression has a significant impact on the QoL of patients. Adequate training has to be provided to the parents and caretakers of such patients, to ensure that human beings suffering from this benign entity lead a healthy life style.
[1]. Singh H, Maurya V, Saini M, DiastematomyeliaIndian J Radiol Imaging 2000 10:255-57. [Google Scholar]
[2]. Allen LM, Silverman RK, Prenatal ultrasound evaluation of fetal diastematomyelia: two cases of Type I split cord malformationUltrasound Obstet Gynecol 2000 15:78-82. [Google Scholar]
[3]. Brian EK, Neuroradiology of the spine. In: David SText book of radiology and imaging 1998 6th edNew YorkChurchill Livingstone:1497-99. [Google Scholar]
[4]. Sepulveda W, Kyle PM, Hassan J, Weiner E, Prenatal diagnosis of diastematomyelia: case reports and review of the literaturePrenat Diagn 1997 17:161-65. [Google Scholar]
[5]. Byrd SR, Darling CP, McLone DG, Developmental disorders of paediatric spineRCNA 1991 29:4-5. [Google Scholar]
[6]. Bruberg JA, Latchaw RC, Emanuel K, Magnetic resonance imaging in occult spinal dysraphismRSNA 1988 26:181-205. [Google Scholar]
[7]. Anand AK, Kuchner E, James R, Cervical diastematomyelia: uncommon presentation of a rare congenital disorderComput Radiol 1985 9:45-49. [Google Scholar]
[8]. Herman TE, Siegel MJ, Cervical and basicranial diastematomyeliaAJR Am J Roentgenol 1990 154:806-08. [Google Scholar]
[9]. Castillo M, Mukherji SK, Imaging of paediatric head neck and spine 1996 PhiladelphiaLippincott Raven:630-35. [Google Scholar]
[10]. McMaster MJ, Occult intraspinal anomalies and congenital scoliosisJ Bone Joint Surgery (Am) 1984 66:588-601. [Google Scholar]
[11]. Han JS, Benson JE, Kaufman B, Demonstration of diastematomyelia and associated abnormalities with MR imagingAJNR Am J Neuroradiol 1985 6:215-19. [Google Scholar]
[12]. Anderson NG, Jordan S, MacFarlane MR, Lovell-Smith M, Diastematomyelia: diagnosis by prenatal sonographyAJR Am J Roentgenol 1994 163:911-14. [Google Scholar]
[13]. Banniza von Bazan U, Krastel A, Lohkamp FW, Diastematomyelia - a harmless finding or cause of late neurological disturbance? [Article in German]Z Orthop Ihre Grenzgeb 1978 116:72-80. [Google Scholar]
[14]. Aesjo M, Harwood-Nash DC, Fitz CA, Chuang SH, Computed tomographic metrizamide myelography in spinal dysraphism in infants and childrenJ Comput Assist Tomogr 1978 2:549-58. [Google Scholar]
[15]. Wolpert SM, Scott AM, Carter BL, Computed tomography in spinal dysraphismSurg Neurol 1977 8:199-206. [Google Scholar]
[16]. James HE, Olift M, Computed tomography in spinal dysraphismJ Comput Assist Tomogr 1977 1:391-97. [Google Scholar]