Functioning Oxyphil Parathyroid Adenoma: A Case Report
Rajendra B Metgudmath1, Vinita V Metgudmath2, Prakash R Malur3, Amal T Das4, Anjali R Metgudmath5
1 Associate Professor, Department of Otorhinolaryngology, Head and Neck Surgery, Jawaharlal Nehru Medical College, KLE University, Belgaum, Karnataka, India.
2 Assistant Professor, Department of Otorhinolaryngology, Head and Neck Surgery, Jawaharlal Nehru Medical College, KLE University, Belgaum, Karnataka, India.
3 Professor, Department of Pathology, Incharge Histo-Pathologist, K.L.E.S. Dr. Prabhakar Kore Hospital & M.R.C, KLE University, Belgaum, Karnataka, India.
4 Post Graduate, Department of Otorhinolaryngology, Head and Neck Surgery, Jawaharlal Nehru Medical College, KLE University, Belgaum, Karnataka, India.
5 Associate Professor, Department of General Medicine, Jawaharlal Nehru Medical College, KLE University, Belgaum, Karnataka, India.
ANME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rajendra B Metgudmath, 95/c, Anugraha, Shanti-Nagar, M.G. Road, Tilakwadi, Belgaum-590006, Karnataka, India.
Phone: +919880327769,
E-mail: drrajmet@yahoo.co.in
Oxyphil parathyroid adenomas are rare and clinical features of patients with this entity are not well defined. We are presenting a case of primary hyperparathyroidism with marked elevation of parathyroid hormone (PTH) and near normal calcium levels, that underwent parathyroidectomy. Histopathology revealed an oxyphil adenoma which showed positivity for PTH on immunohistochemical staining. Post – operatively, there was a significant decline in both PTH and alkaline phosphatase levels. Benign oxyphil adenomas may mimic parathyroid carcinomas, both in terms of clinical features and tumour size; and they should be considered in the differential diagnosis of patients with primary hyperparathyroidism.
Oxyphilic adenoma, Hyperparathyroidism, Parathyroidectomy
Case Report
A 45-year-old female with a left subtrochanteric fracture, who had symptoms of easy fatigability and bone pain, was referred to Head and Neck Oncology Services by an endocrinologist. She did not complain of breathlessness, stridor or dysphagia. Her menstrual periods were normal. There was no family history for osteoporosis, renal stones or parathyroid disease. On physical examination, her blood pressure was found to be 128/78 mm Hg. Neck examination showed that trachea was deviated to the right, with no cervical lymphadenopathy. Cardiovascular, pulmonary and abdominal examinations were within normal limits.
Blood investigations done at the time of her admission revealed an elevated serum parathyroid hormone (PTH) level of 599.6 pg/mL, an elevated alkaline phosphatase (ALP) level of 1075 U/L, a near normal calcium level 10.3 mg/dL, along with a normal magnesium level of 1.7 mg/dL and a normal phosphorous level of 2.3 mg/dL [Table/Fig-1]. Kidney, liver and thyroid function tests were within normal limits. The 24-hour urine calcium test was within normal limit.
Pre-operative and post-operative biochemical profile
| S. PTH | ALP | S. Ca | S. Mg | S. Ph |
|---|
| Normal range | 11.1 – 79.5 pg/mL | 50 – 140 U/L | 8.5 – 10.1 mg/dL | 1.7 – 2.5 mg/dL | 2.5 – 4.8 mg/dL |
| Pre – op | 599.6 | 1075 | 10.3 | 1.7 | 2.3 |
| Post – op | 12.4 | 220 | 7.4 | 1.3 | 1.5 |
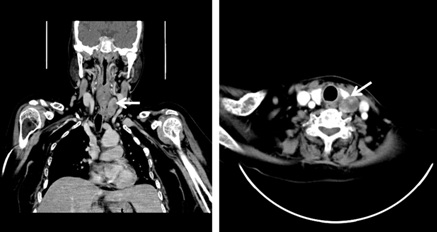
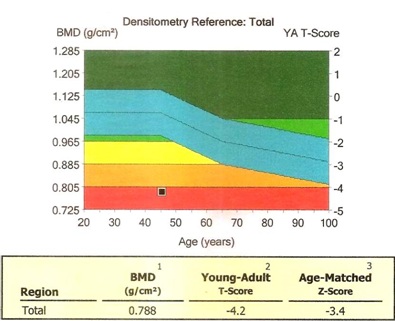
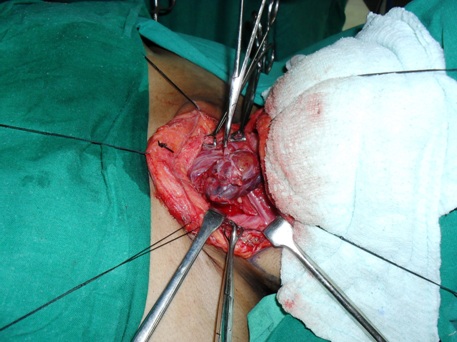
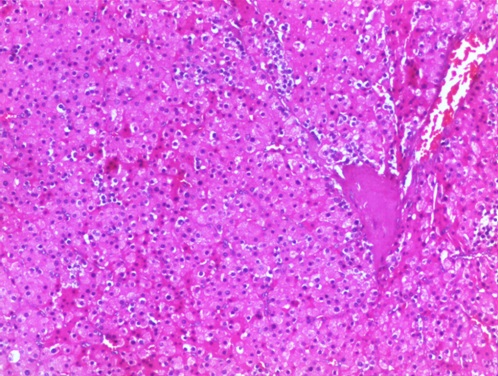
Chest X–ray showed diffuse osteopaenia of visualized bones, with evidence of multiple fractures involving 3rd to 11th ribs, on both sides of chest wall. X-ray of left knee showed a generalized decrease in bone density. X-ray of pelvis and both hips revealed generalized osteopaenia with evidence of multiple well circumscribed lytic lesions involving the pelvic bones and bilateral femur, along with a subtrochanteric fracture of the left femur [Table/Fig-2]. Ultrasonography of neck revealed two mixed echoic lesions with central necrotic areas, adjacent to the posterior aspect of the left lobe of thyroid, respectively measuring 2 x 1.3 cm and 1.5 x 1.5 cm. On doing Colour Doppler studies, the lesions showed central and peripheral vascularity. A computed tomography scan revealed a well-defined heterogeneously enhancing lesion, posterior to the left lobe of thyroid, while the other parathyroid glands were of normal sizes [Table/Fig-3]. Dual energy X- ray absorptiometry (DEXA) scan revealed a total T-score of – 4.2 within the osteoporotic range (T score less than or equal to -2.5), which was suggestive of severe demineralization [Table/Fig-4] Thus, a diagnosis of single gland hyperplasia was made and the patient was subjected to left parathyroidectomy under general anaesthesia. During surgery, a large neck mass measuring 4.0 x 2.8 x 1.7 cm and weighing 20 grams was resected [Table/Fig-5]. Histopathology revealed a capsulated tumour consisting of cords and nests of cells with large granular eosinophilic cytoplasm, with round to oval nuclei, with a thin rim of compressed parathyroid tissue being seen outside the capsule, which was suggestive of an oxyphil adenoma [Table/Fig-6]. Immunohistochemical staining showed positivity for PTH. The blood investigations done 12 hours post-operatively, revealed a fall in PTH level to 12.4 pg/mL, in ALP level to 220 U/L and in serum calcium level to 7.4 mg/dL. In the next three days, serum calcium level further reduced to 6.5 mg/dL and it was managed with intravenous calcium supplementation. Serum phosphorous and magnesium levels were also found to be low post-operatively [Table/Fig-1]. The serum calcium level was 8.6 mg/dL on 7th post-operative day. The patient was referred to an orthopaedician with a prescription of 3 grams of calcium bicarbonate and 0.75μg of calcitriol daily. The patient was lost to follow-up after discharge.
Generalised osteopaenia with evidence of multiple well circumscribed lytic lesions involving the pelvic bones and bilateral femur along with subtrochanteric fracture of the left femur (arrow)

CT scan revealed well-defined heterogeneously enhancing lesion posterior to the left lobe of thyroid (arrow) while the other parathyroid glands were of normal size
DEXA scan showing severe osteoporosis
Intraoperative photograph showing the parathyroid adenoma weighing 20 grams
Oxyphillic cells seen with large granular eosinophilic cytoplasm with round to oval nuclei.(H & E stain, 10 x)
Discussion
Parathyroid adenomas which are composed predominantly of chief cells are the most frequent cause of primary hyperparathyroidism. Parathyroid adenomas of the oxyphil cell type, an infrequent histologic subtype, are rarely seen. Warren and Morgan, in 1935, were the first to report a pure functioning oxyphil adenoma of the parathyroid [1]. Due to lack of proper biochemical studies prior to 1978, oxyphil adenomas of parathyroid were generally considered to be non-functioning [2]. The diagnostic criteria proposed by Wolpert and Vickery in 1989 for functioning oxyphil adenomas were as follows: (a) at least 90% of the adenoma should be composed of oxyphil cells, (b) a biopsy or excision of a second histologically normal parathyroid gland, excluding the diagnostic possibility of hyperplasia and (c) a post-operative alleviation of hypercalcaemia [3]. The review of literature has revealed only 142 cases of oxyphil parathyroid adenomas to date, out of which only 124 were found to be functional [3–5].
The normal parathyroid gland weighs about 25-35 mg, while an average chief-cell parathyroid adenoma weighs 0.5 gram. The oxyphil variants are known to be heavier, with an average weight of 1.2 gram [4]. In 2004, Fleisher et al described two cases of abnormally large oxyphil parathyroid adenomas which weighed 7 and 25 grams [5]. In our case, the oxyphil adenoma weighed 20 gram, which raised a clinical suspicion of a parathyroid carcinoma [4]. Microscopically, oxyphil cells are larger than chief-cells and they are filled with abundant eosinophilic cytoplasm, which may explain their large sizes [5]. Serum PTH levels in parathyroid carcinomas are often 3-10 times the upper limit of normal, whereas in typical benign lesions, values are frequently less than twice normal. In our study, the serum PTH levels were 7.5 times the upper limit of normal, which suggested that the tumour was a parathyroid carcinoma (which mimicked its features). Benign oxyphil parathyroid adenomas may mimic parathyroid carcinomas, both in terms of clinical features, biochemical parameters and tumour sizes.
Recently, Gurrado et al described an interesting case of a substernal oxyphil parathyroid adenoma with hypercalcaemia and normal PTH levels, but which produced a parathyroid-hormone-related peptide, which was managed by radioguided parathyroidectomy [6]. Although elevated PTHrP has been associated with humeral hypercalcaemia of malignancy, its exact role in causing hyperparathyroidism has not been established. They suggest measuring parathyroid-hormone-related peptide (PTHrP) in all cases of hypercalcaemia, even when a malignancy is not suspected.
Ectopic parathyroid adenomas are a reason for failures of primary surgeries and hence, a preoperative localization of the lesion by doing imaging studies, such as seastimibi scan, positron emission tomography scan and CT scan, will facilitate surgeons [7]. Even though Tc-99m-sestamibi scan uptake scan was not performed in our study, it has been found to be useful in detecting metabolically active oxyphil adenomas and especially, when pre-operative calcium level is greater than 9.5mg/dL. This helps in mitigating the risk of a bilateral neck exploration and the need of a second surgery, to hunt for ectopic parathyroid glands [7].
Conclusion
Benign oxyphil adenomas may mimic parathyroid carcinomas, both in terms of clinical features and tumour sizes. A multi-disciplinary team approach in an intensive care setting, would help in avoiding a lengthy and stormy post-operative course in such patients. Functioning oxyphil parathyroid adenomas should be considered in the differential diagnosis of patients with primary hyperparathyroidism, who present with atypical biochemical and clinical manifestations.
[1]. Warren S, Morgan Jr E, The Parathyroids: II. A Histologic study of parathyroid adenomaArch Pathol 1935 20:823-26. [Google Scholar]
[2]. McGregor Lotuaco LG, Rao MS, Chu LLH, Functioning oxyphil adenoma of parathyroid glandAm J Pathol 1978 92:691-711. [Google Scholar]
[3]. Wolpert HR, Vickery AL Jr, Wang CA, Functioning oxyphil cell adenoma of the parathyroid gland. A study of 15 casesAm J Surg Pathol 1989 13:500-04. [Google Scholar]
[4]. Bedetti CD, Dekker A, Watson CG, Functioning oxyphil cell adenoma of parathyroid gland: A clinicopathologic study of ten patients with hyperparathyroidismHum Pathol 1984 15:1121-26. [Google Scholar]
[5]. Fleischer J, Becker C, Hamele-Bene D, Breen TL, Silverberg SJ, Oxyphil parathyroid adenoma: a malignant presentation of a benign diseaseJ Clin Endocrinol Metab 2004 89:5948-51. [Google Scholar]
[6]. Gurrado A, Marzullo A, Lissidini G, Substernal oxyphil parathyroid adenoma producing PTHrP with hypercalcemia and normal PTH levelWorld J Surg Oncol 2008 6:24 [Google Scholar]
[7]. Bleier BS, LiVolsi VA, Chalian AA, Gimotty PA, Botbyl JD, Weber RS, Technetium Tc 99m sestamibi sensitivity in oxyphil cell dominant parathyroid adenomasArch Otolaryngol Head Neck Surg 2006 132:779-82. [Google Scholar]