The corneal endothelium is the innermost layer of the cornea which is essential for maintenance of normal corneal hydration, thickness and transparency. The human corneal endothelium has little or no ability to divide after birth [1–3]. There have been several advances in the recent years in the field of cataract surgery including phacoemulsification technique for cataract management. Today’s cataract surgery focuses on rapid visual rehabilitation and minimum surgically induced astigmatism. Despite all the advances, corneal endothelial loss remains to be a matter of concern particularly in patients with lower endothelial reserve or dysfunctional endothelium. Varying amount of corneal endothelial loss in even uneventful cataract surgery has been reported [4–6]. Increased nuclear opalescence and dense cataract has stated to be a risk factor for more corneal endothelial loss in phacoemulsification [6–8]. Phacoemulsification is not viable economically in developing countries like India, as it is machine dependent and needs trained surgeon and support staff. MSICS is an alternative technique to phacoemulsification which gives comparable results and is cost-effective [9,10]. It is particularly useful in these dense cataracts which are seen more frequently in countries like India [11].
Diabetes affects both the corneal thickness and the morphology of the endothelial cells. Hyperglycaemia in these patients causes metabolic stress which can lead to lower endothelial cell density and greater pleomorphism and polymegathism. Various studies have shown abnormal corneal morphology along with higher rate of corneal endothelial cell loss, and decreased corneal endothelial cell density in diabetics. These endothelial changes, because of the disease, may lead to a high-risk cornea, particularly in hard cataract [12–16]. We therefore evaluated the effect of manual small incision cataract surgery on cornea of diabetes mellitus patients with Nucleus Sclerosis grade 5 or grade 6 according to Lens Opacities Classification System III (LOCIII) [17].
Materials and Methods
This prospective non-randomized study was conducted over a period of 12 months in the department of Ophthalmology at Himalayan Institute of Medical Sciences, Dehradun, India from April 2008 to March 2009. Sixty diabetic patients and 60 healthy age matched control of senile cataract between the age of 50-70 years with nucleus sclerosis of Grade 5 and Grade 6 according to LOCIII undergoing MSICS were included for the study [17].
Exclusion criterion included patients under the age of 50 and over 70 years; any other types of cataract other than age-related; pre-operative endothelial count less than 1500 cells/mm [2]; pupillary dilation less than 7 mm; previous intra-ocular and refractive surgery; patients of glaucoma; any condition that impeded corneal evaluation by specular microscopy and pachymetry; intraoperative complications.
The study was approved by the local research and ethics Committee and written informed consent was obtained from each patient after explanation of the nature of the study.
Pre-operative Examinations
All patients underwent a complete ocular examination. Endothelial cell count was done pre-operatively and post-operatively at one week, six week and 12 weeks. The cataract was graded according to the LOCS III. Intra Ocular Pressure (IOP) was recorded using applanation Goldman tonometer. Evaluation of posterior segment was done using indirect ophthalmoscopy and with B scan (Nidek’s Ultrasound US-4000) in mature cataract.
Central corneal pachymetry and central corneal endothelial cell density was determined by SP-2000P non-contact specular microscope (Topcon America Corporation, Paramus, NJ). Corneal endothelial cell density (cells/mm2) was calculated by analysing minimum of 20 cells in the central cornea pre-operatively and post-operatively on subsequent follow up as per protocol.
Surgical Technique
Sixty eyes of 60 diabetic patient and 60 eyes of 60 non-diabetic patients underwent MSICS. All the eyes were dilated pre-operatively with tropicamide and phenylnephrine eye drops. Surgeries were performed under peribulbar anaesthesia using 5 mL of lignocaine and bupivacaine in ratio of 1:1 with 150 units of hyaluronidase. Surgery was done through 6.5 mm frown scleral incision. The viscoelastic used was methyl cellulose 2 percent in all patients. Nucleus was prolapsed in anterior chamber after performing capsulorhexis and delivered with irrigating wire vectis. Single piece polymethylmethacrylate intra-ocular lens was implanted in the bag in all patients after cortical aspiration. All the surgeries were done by two surgeons, RN and RD.
The percentage of post-operative endothelial cell loss (ECL per cent) was calculated as follows:

where Post-operative corneal endothelial cell count readings noted at 12 weeks post-operatively.
The data collected was subjected to the standard statistical analysis by SPSS version 19 software (SPSS Inc. Chicago, USA). The normality of data was tested. The data was homogenous and normally distributed hence one-way ANOVA was used among groups and paired t-test was used within groups for analysis. Pearson test was used for correlations among parameters. P-values <0.05 were considered statistically significant.
Results
In the current study, the male: female ratio in diabetic group was 1.06:1 and in non-diabetic group, it was 1:1. [Table/Fig-1] shows baseline information. In the diabetic group, nucleus sclerosis Grade 5 was present in 56.66% cases while Grade 6 was present in 43.33% cases. In control group nucleus sclerosis grade 5 was present in 53.33% cases while Grade 6 was present in 46.66 per cent cases. There was no case of irreversible corneal damage and decompensation at 12 weeks in both groups.
Mean age, Operative time and Visual acuity
| Study Group | Non Diabetic Group n=60 | Diabetic Group n=60 |
|---|
| Mean Age (years) | 60.88±6.035 | 60.28±5.785 |
| Pre-operative Visual Acuity LogMAR | < 1 | <1 |
| Best Corrected Visual Acuity LogMAR | 0.16±0.12 | 0.22±0.16 |
| Mean Operative time(minutes) | 12.6±4.1 | 14.4±3.4 |
Pre- and Post-operative Corneal Endothelial Counts
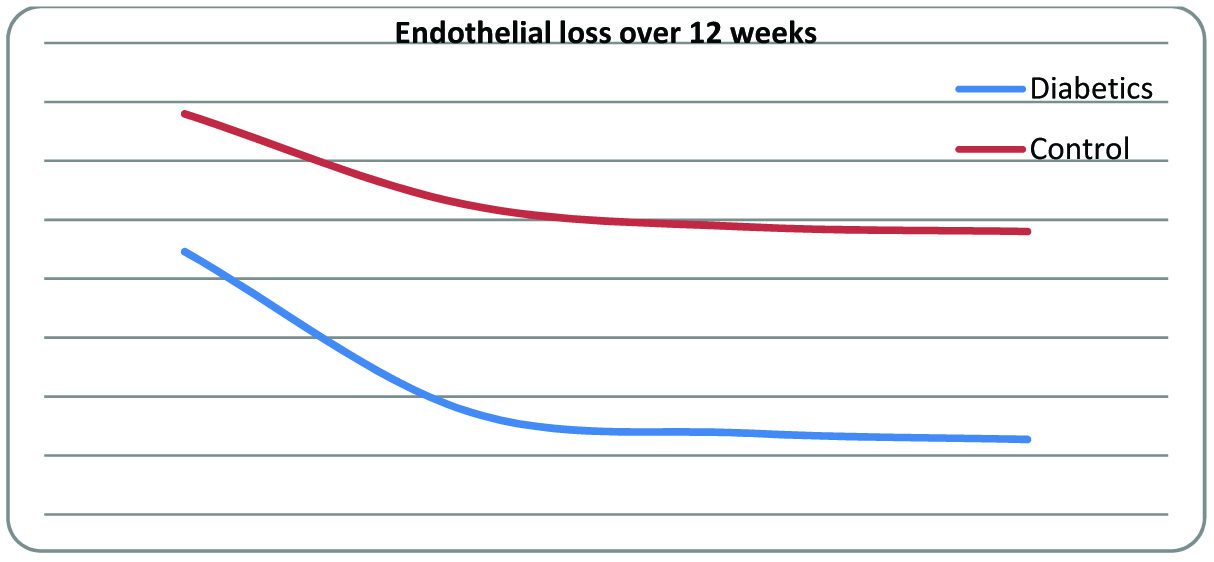
The mean pre-operative endothelial count in the control group was significantly higher than the diabetic group (p<0.001) [Table/Fig-2]. The post-operative endothelial loss in the both the groups were statistically significant (one-way ANOVA p<0.001). On comparing post-operative endothelial loss in control group to diabetic group, the diabetic group had significantly higher endothelial loss (p<0.001). [Table/Fig-3] shows the trend of endothelial loss in both groups over 12 weeks.
Mean Pre-operative and Post-operative corneal endothelial cell count
| Groups | Pre-operative cell count | Post-operative cell count | Endothelial cell loss % |
|---|
| 1 week | 12 week |
|---|
| Diabetics | 2245.87±528 | 1976.7±489.2 | 1927.25±488.7 | 318.6(14.19%) |
| Control | 2479.83±399.5 | 2326±395.3 | 2280±393 | 199.8 (8.05%) |
Post-operative Endothelial Loss over 12 weeks
Pre- and Post-operative Corneal Endothelial Indices
The pre-operative coefficient of variance for control group was significantly lower to that of diabetic group (p<0.001) [Table/Fig-4]. The pre-operative percentage of hexagonal cells were higher in control group than diabetic group (p<0.001). The post-operative change in coefficient of variance and percentage of hexagonal cells within both the groups changed significantly (p<0.001). The change in percentage of hexagonal cells in diabetic group was significantly higher than in control group (p=0.005). Inter group change in co-efficient of variance was however not statistically significant (p=0.144).
Pre-operative and Post-operative corneal endothelial indices Abbreviations: CV Coefficient of variance
| Cell Morphology indices | Diabetics group | Control group |
|---|
| Pre-operative | Post-operative | Pre-operative | Post-operative |
|---|
| CV | 24.36±5.39 | 21.84±5.28 | 19.93±4.9 | 17.6±4.6 |
| % Hexagonal cells | 66.98±6.642 | 64.08±6.74 | 77.73±6.47 | 75.35±6.74 |
Pre- and Post-operative Central Corneal Endothelial Thickness
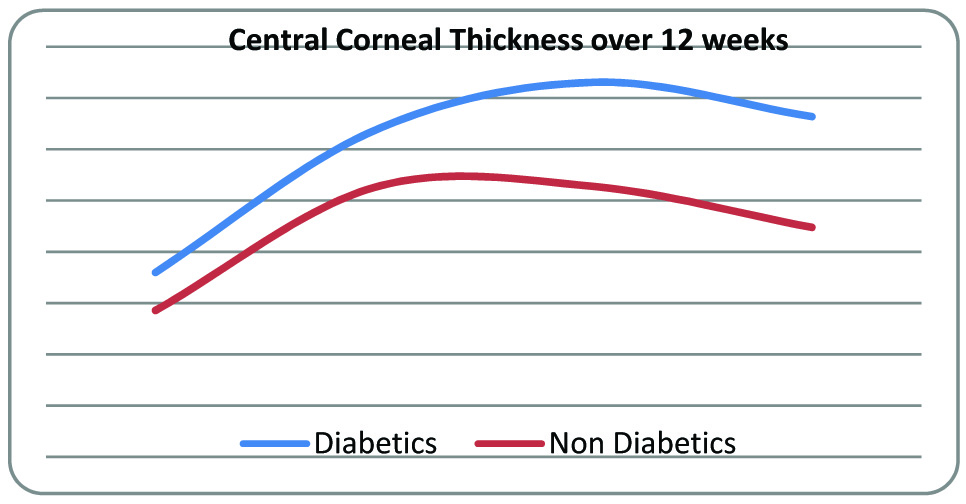
The central cornea was thicker in diabetic group compared to control group (p=0.05) [Table/Fig-5]. The thickness of cornea increased in both groups significantly (p=0.013 in control group and p<0.001 in diabetic group). On comparing inter group change, there was also a significant increase in central corneal thickness in diabetics as compared to control (p=0.004). [Table/Fig-6] shows the general trend of change in central corneal thickness in both groups.
Pre-operative and Post-operative central corneal thickness
| Central corneal thickness in micron | Diabetic group | Control group |
|---|
| Pre-operative | Post-operative | Pre-operative | Post Op |
|---|
| 1 week | 6 week | 12 week | 1 week | 6 week | 12 week |
|---|
| 509±25.5 | 533.7±26.3 | 543.1±26.6 | 536.4±28.4 | 498.6±30.3 | 522.6±31.4 | 522.8±30.1 | 514.8±26.2 |
Change in central corneal thickness in both groups
Corneal Changes According to Age and Duration of Diabetes
Pre-operative central corneal thickness of both the groups was correlated to age of patient. In diabetic group, the central corneal thickness correlated positive with the age of patient (Pearson correlation factor r=0.541 p=0.019.The endothelial loss did not show any correlation to duration of diabetes [Table/Fig-7].
Cell loss according to duration of Diabetes
| Duration of diabetes years | Pre-operative cell count | Post-operative cell count 12 weeks | Endothelial cell loss % |
|---|
| 0-10 (n=26) | 2269.65±484 | 1956±469.7 | 13.8% |
| 11-20(n=34) | 2228±609.7 | 1905.6±550.6 | 14.47% |
Discussion
MSICS has become popular as a cost effective, sutureless surgery providing early visual rehabilitation [18]. Researchers have long speculated about safety of phacoemulsification in dense cataracts. A study conducted by Bourne et al., compared endothelial loss by phacoemulsification to conventional extracapsular cataract extraction. Although no significant difference was reported in overall corneal endothelial cell loss between these two procedures these authors emphasised on an increased risk of severe corneal endothelial cell loss with phacoemulsification in patients with dense cataracts of up to 52.6% in comparison to 23.1% with extra-capsular extraction [19].
The current study evaluated effect of MSICS on cornea in diabetic patient with advanced and dense cataract. The pre-operative corneal endothelial cell was measured in both the diabetic group and the healthy age matched control group. Diabetic patients had a significantly lower endothelial count. Studies conducted by Lee et al., [15] and Ranganath et al., [20] reported lesser number of endothelial cell in diabetics as compared to non-diabetics. A recent study conducted in southern India with a large study sample showed that the mean endothelial cell density was significantly lower across all age groups in patients with Type 2 diabetes mellitus compared with controls [21]. Some studies elsewhere have shown no difference in endothelial counts of diabetic patients [14, 22]. The pre-operative coefficient of variation in diabetic group was significantly higher than in control group and the percentage hexagonal cells were lower in diabetic than age matched control group. The central corneal thickness in diabetics was significantly thicker in the study group. Similar results have been seen in studies elsewhere [12, 22]. These results suggest that though patients with diabetes have altered endothelial cell morphology and function duration of diabetes has no bearing to it.
In the current study, both the groups showed significant corneal endothelial loss in the post-operative period. The endothelial count showed progressive decrease in post-operative period, up to three months in both groups. However this endothelial loss was more pronounced in the diabetic group as compared to the control group. Despite the decrease in endothelial count in the diabetic group, none of the patients developed corneal decompensation.
Duration of diabetes was further correlated with the mean post-operative endothelial loss. There was no statistical significance of the percentage endothelial cell loss to the duration of diabetes. There was steady decrease in percentage of hexagonal cells and increase in coefficient of variance in both the groups. Both these parameters reflect the endothelial cellular repair of cornea. The change in percentage of hexagonal cells was statistically significant in diabetic group. Morikubo et al., in their study of phacoemulsification in diabetic patients reported significant endothelial loss in diabetic group in comparison to non-diabetic group. They however found no statistical difference between change in percentage of hexagonal cells and coefficient of variations [23]. A study conducted by Mathew et al., on MSICS in diabetic patients showed decreased endothelial count in diabetics at 3 months. Post-operatively the endothelial loss in control group versus diabetics was 16.58 + 12.9 per cent and 19.24 + 11.57 per cent. The diabetics group however had a higher mean pre-operative endothelial count compared to control group in this study. They noted no statistically significant change in coefficient of variance. Percentage of change in hexagonal cells was not reported in their study [24].
In the present study, in post-operative follow up central corneal thickness was increased in both the groups. The change in corneal thickness was statistically significant in both groups. The cornea in diabetic group was much thicker compared to control group and the difference in post-operative corneal thickness in both groups was also statistically significant. The recovery of cornea in diabetics takes longer compared to normal controls. Increased post-operative corneal thickness in diabetics has been reported by Morikubo et al., in their study of phacoemulsification in diabetic patients [23]. It is thought that in diabetic’s aldose reductase causes intracellular accumulation of polyol, which acts as an osmotic agent leads to swelling of the endothelial cells. Diabetes also reduces the activity of Na + K + ATPase of the corneal endothelium and this causes the morphological and functional changes of diabetic corneas [24, 25].
To summarise, the results of above study show that in patients with advanced nuclear sclerosis and brunescent cataract, there is higher endothelial loss in normal and diabetic patients. Diabetics have a lower functional reserve as compared to normal subjects and the diabetic cornea is more vulnerable to insults. Despite this, MSICS is safe surgery even in brunescent cataracts.
Limitations
The limitations of the present study were that it was a non-randomized study. The sample size was small and the follow up period was of short duration.
Conclusion
The morphological changes in cornea of diabetics are associated with low functional reserve. This may cause mild risk of corneal decompensation in these patients. Pre-operative evaluation of corneal endothelium in diabetic patients is therefore recommended before intraocular surgeries. Due precautions should be taken to minimize insult to corneal endothelium during surgery. Knowing the expected corneal endothelial loss in uneventful surgery in diabetics may help in better patient selection especially in brunescent cataracts. In diabetic patients, MSICS is a safe technique even in dense cataracts with acceptable post-operative endothelial loss.