Postpartum haemorrhage is a leading cause of global maternal mortality and morbidity, accounting for 25-30% of all maternal deaths, and 75-90% of these casualties result from uterine atony. Uterine compressive sutures are a well established measure for control of haemorrhage following atonic postpartum haemorrhage, when medical and non-medical interventions fail.
Here, we are reporting a case of secondary infertility in a 24-year-old lady who had undergone an elective caesarean section for central placenta previa in her first pregnancy. She had massive postpartum haemorrhage, for which B-Lynch suture and vessel ligation were done. Subsequently, she failed to conceive for 4 years. This was because of severe pelvic adhesions and uterine deformation which were found intraoperatively, as a consequence of previous use of B-Lynch suture. As no definitive treatment could be offered to her, we suggested her to go for adoption.
Postpartum haemorrhage, B-Lynch suture, Synechia, Fertility
Case Report
A 24-year-old lady, P1L0, presented with secondary infertility. She was anxious to conceive and had oligomenorrhoea for the past 4 years. She had a term intrauterine foetal demise in her first pregnancy, with central placenta previa, for which she had undergone an elective caesarean section at a tertiary care hospital four years back. Following caesarean section, she had massive postpartum haemorrhage, which was refractory to uterotonic drugs, B-Lynch suture, bilateral uterine artery ligation, but she finally responded to bilateral internal iliac artery ligation. She was in the intensive care unit for one week and her total duration of hospital stay was 14 days. Her past medical history was uneventful. There was no history which was suggestive of tuberculosis or pelvic inflammatory disease. She postponed any further conception for three years because of fear of childbirth. She presented to us after four failed attempts of ovulation induction. General and systemic examinations were within normal limits. Per-speculum examination was normal and per vaginal examination revealed a normal sized, anteverted uterus with restricted mobility. Her eagerness to conceive led us to investigate her in the line of secondary infertility.
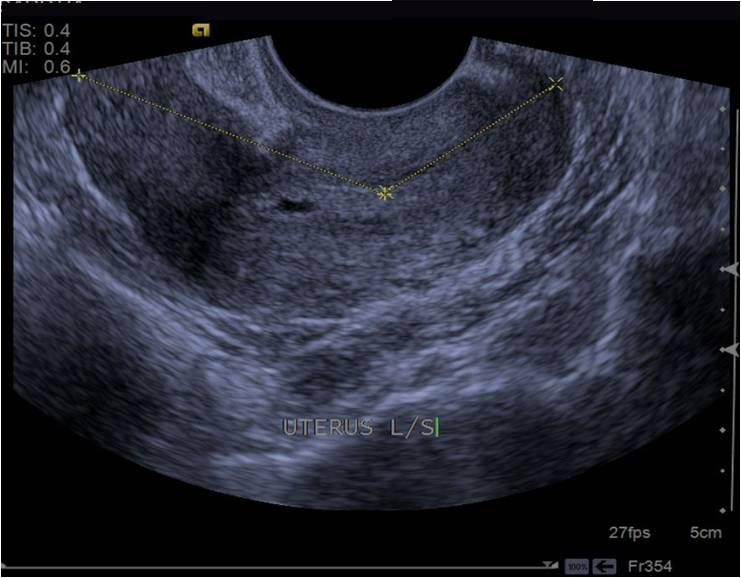
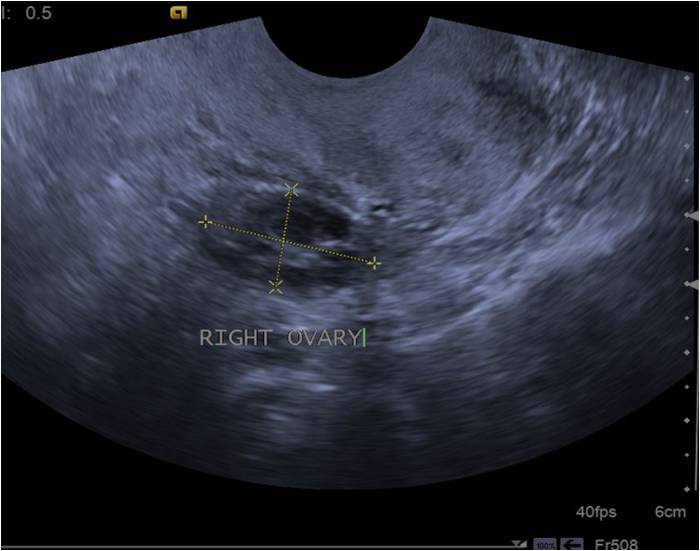
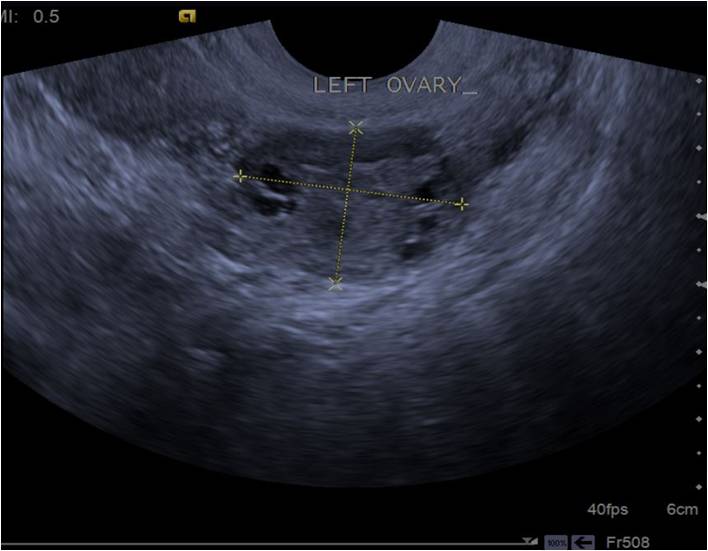
A transvaginal ultrasound which was done, showed a normal sized but severely distorted uterus with undelineated endometrium [Table/Fig-1]. Both ovaries appeared normal [Table/Fig-2,3]. To know more about the status of uterine cavity and fallopian tubes, we proceeded with hysterosalpingography. We got a report of a narrow endometrial cavity, without any opacification of fallopian tubes and absence of peritoneal spillage [Table/Fig-4]. For further confirmation, we did a diagnostic hysterolaparoscopy. We faced difficulty in advancing the hysteroscope beyond the internal Ostium (OC), due to extensive intrauterine adhesions. A concurrent laparoscopy revealed severe pelvic adhesive disease and a distorted uterus, but the bilateral tubes and ovaries appeared to be normal. We explained about the findings and causes of her secondary infertility to the patient. She was counselled to go for adoption, as her uterus was severely deformed and as she had economic constraints in going for assisted reproductive technology.
Transvaginal sonography showing saggital view of distorted uterus of size 8.2cm×4cm with undelineated, thin echogenic endometrium
Transvaginal sonography showing, right ovary of size of 3.2cm × 2.5cm with multiple ovarian follicles
Transvaginal sonography showing ,left ovary size of 3.7cm ×3 cm with multiple ovarian follicles
Hysterosalpingography showing a narrow uterine cavity, without any opacification of fallopian tubes and absence of peritoneal spillage

Discussion
Postpartum haemorrhage is a leading cause of global maternal mortality and morbidity, accounting for 25-30% of all maternal deaths, and 75-90% of these casualties result from uterine atony [1]. Traditionally, surgical management of refractory postpartum haemorrhages has always relied on postpartum hysterectomy which results in complete inability in hosting a future pregnancy, a psychological impact and risk of intra-operative surgical morbidities, particularly if the procedure is not performed under optimal circumstances. With the goal of preservation of reproductive capacity, as an alternative to this radical treatment, various conservative surgical managements have been proposed.
Uterine compressive sutures are a well established measure for control of haemorrhage following atonic postpartum haemorrhage, when medical and non-medical interventions fail [2].
Traditionally, surgical management of refractory postpartum haemorrhages has always relied on postpartum hysterectomy which results in complete inability in hosting a future pregnancy, a psychological impact and risk of intra-operative surgical morbidities, particularly if the procedure is not performed under optimal circumstances. With the goal of preservation of reproductive capacity, as an alternative to this radical treatment, various conservative surgical managements have been proposed.
Conservative surgical management which involves surgical ligation of pelvic arteries (internal hypogastric artery) was described by Sagarra M et al in the early 1960s, bilateral uterine artery ligation was described by O’Leary in 1966 and stepwise uterine devascularization procedure used in cases of postpartum haemorrhage was described by Abd Rabbo [3–5]. Then came the B-lynch uterine compression suture which was first reported in 1997 and it has gained popularity, with a number of subsequent publications attesting to its efficacy [6,7].
B-Lynch compression brace suture technique is one of the established conservative surgical procedures which are done for atonic postpartum haemorrhage. B-Lynch is a uterine compression suture, which apposes the anterior and posterior wall through a pair of vertical brace sutures which are put around the uterus. It works by direct application of pressure on the bleeding placental bed and by reducing the blood supply to uterus. The success rate of B-Lynch in avoiding hysterectomy is 86.4% and it has been widely recommended for controlling postpartum haemorrhages [6]. Reports on either successful or unsuccessful pregnancies which followed B-Lynch are meagre in literature. B-Lynch has been heralded as a life and fertility preserving technique for postpartum haemorrhages. It can at times, though, lead to unwarranted post-operative sequlae, ending up in hysterectomies. A case of total uterine necrosis was reported, following which a hysterectomy was done [8]. Ochoa et al., have also reported infectious complications like pyometra after peformance of B-Lynch [9]. Suture related complications like erosion into the lower segment of the uterus during 6th week of postpartum period, which lead to anterior wall defects, have also been reported [10].
In our case, the B-Lynch led to synechia, and pelvic adhesions, jeopardizing any further scope for pregnancy. Similar cases have also been reported in literature. Rathat G et al., followed 37 post uterine compression suture patients and found that 7 had synechia of varying degrees, with three of them having severe synechia which was akin to Asherman’s syndrome [11]. One nearly similar isolated case of Asherman’s syndrome which occurred after B-Lynch and vessel ligation done for postpartum haemorrhage, has been reported by Goojha et al., [12]. Akoury and Sherah reported a patient who required both B-Lynch and Cho compressive sutures, who developed uterine synechia in the early post-operative period and for which synechial lysis was done hysteroscopically. After this, patient had a full term pregnancy one year later and an area of full thickness myometrial necrosis was noted, which required operative resection. The author concluded that pressure which was produced by the compressive sutures may have caused progressive myometrial necrosis [13]. In our case, B-Lynch suture, followed by bilateral uterine and hypogastric artery ligation was done, to control postpartum haemorrhage. In hindsight, we feel that the extensive pelvic adhesions could have been caused by the effect of the combined surgical procedures. It has also been stated that synechia can occur because of the use of delayed absorbable sutures, causing ischaemic necrosis and extensive folding of uterine wall, which are produced by compressive force of the suture. Though vessel ligation was performed in this case, literature shows that it does not compromise with women’s subsequent fertilities and obstetrical outcomes [14].
Not all women with B-Lynch sutures have dismal outcomes. Successful pregnancies have been documented. Baskett TF et al., reported seven uneventful pregnancies which followed B-Lynch, which remains the largest review with positive outcomes [15]. However, the pregnancy outcomes are not always encouraging after B-Lynch use, as many of the women don’t reach term gestations and as they unfortunately suffer unexpected complications. A case of uterine rupture which occurred at third trimester following B-Lynch suture use has been reported [16]. Similarly, a full thickness myometrial necrosis which occurred in a subsequent pregnancy has also been reported by Akoury et al., This was noticed during caesarean section and it was thought to be caused by compression effect of sutures, which may have led to uterine wall necrosis, both anteriorly and posteriorly [13].
Conflicting reports surface regarding fertility outcomes, when B-Lynch is combined with vessel ligation. Some authors advocated that use of B-Lynch with stepwise uterine devascularization had no deleterious effect on successful pregnancies [17]. However, there are some reports where B-Lynch was used only for control of postpartum haemorrhage, without any vessel ligation and the pregnancy outcomes in these cases were also favourable [18]. The sequence of management for postpartum haemorrhage, as per WHO guidelines, states that after failure of conservative management, compression sutures should be attempted before vessel ligations [2]. But Sentilles et al., strongly advocates vessel ligation technique, out of which bilateral uterine artery ligation should be the first choice for surgical management, as it is a well assessed, simple, rapid and an effective procedure than B-lynch suture. It is the first line uterus sparing procedure which should be used for postpartum haemorrhage, as long as the impact on patient’s subsequent fertility and pregnancies which follow B-Lynch remains insufficiently assessed [19].
Conclusion
All the patients who undergo compression sutures should be advised strict follow ups to assess any procedure related complications and fertility outcomes, which was lacking in our case, as she never received any obstetric and gynaecological consultation for four years. An earlier consultation could have led to a more fruitful outcome. As the fertility data on B Lynch only technique or B Lynch and its modifications with concomitant vessel ligation are limited, this case is reportable and consensus guidelines should be formulated and followed universally.
[1]. Zheng J, Xiong X, Ma Q, Zhang X, Li M, A new compressive suture for postpartum hemorrhage with atonyBJOG 2011 118:370-4. [Google Scholar]
[2]. WHO guidelines for the management of postpartum hemorrhage and retained placenta. Geneva: World Health Organisation, c2009 [Google Scholar]
[3]. Sagarra M, Glasser ST, Stone ML, Ligation of the internal iliac vessels in the control of post-partum hemorrhage: report of a caseObstet.Gynecol 1960 15:698-701. [Google Scholar]
[4]. O’Leary JL, O’Leary JA, Uterine artery ligation in the control of intractable postpartum hemorrhageAm J Obstet Gynecol 1966 94:920-24. [Google Scholar]
[5]. AbdRabbo SA, Stepwise uterine devascularisation: a novel technique for management of uncontrolled postpartum hemorrhage with preservation of the uterusAm J Obstet Gynecol 1994 171:694-700. [Google Scholar]
[6]. B-Lynch C, Coker A, Lawal AH, Abu J, Cowen MJ, The B-Lynch surgical technique for the control of massive postpartum haemorrhage: an alternative to hysterectomy? Five cases reportedBr J Obstet Gynaecol 1997 194:372-5. [Google Scholar]
[7]. Ducas JV, Busowski MT, Busowski JD, Smithson S, Masters K, Sibai BM, Surgical treatment of uterine atony employing the B-Lynch techniqueJ Matern Fetal Med 2000 9:194-6. [Google Scholar]
[8]. Treloar EJ, Anderson RS, Andrews HS, Bailey JL, Uterine necrosis following B-Lynch suture for primary postpartum haemorrhageBJOG 2006 113:486-8. [Google Scholar]
[9]. Ochoa M, Allaire AD, Stitely ML, Pyometria after hemostatic square suture techniqueObstet Gynecol 2002 99:506-9. [Google Scholar]
[10]. Grotegut CA, Larsen FW, Jones MR, Livingston E, Erosion of a B-Lynch suture through the uterine wall: a case reportJ Reprod Med 2004 49:849-52. [Google Scholar]
[11]. Rathat G, Dotrirh P, Mercier G, Reyftmann L, Dechanet C, Boulot P, Synechia after uterine compressive sutureFertil Steril 2011 95(1):405-9. [Google Scholar]
[12]. Goojha Case A, Pierson A, Development of asherman syndrome after conservative surgical management of intractable Postpartum hemorrhageFertil Steril 2010 94(3):1098e1-5. [Google Scholar]
[13]. Akoury H, Sherman C, Uterine wall partial necrosis following combined B-Lynch and Chi-square sutures for the treatment of primary postpartum hemorrhageJ Obstet Gynaecol Can 2008 30:421-4. [Google Scholar]
[14]. Nizard J, Barrinque L, Frydman R, Fernandez H, Fertility and pregnancy outcome following hypogastric artery ligation for severe Postpartum hemorrhageHum Reprod 2003 18(4):844-8. [Google Scholar]
[15]. Basket TF, Uterine compressive sutures for postpartum hemorrhage: efficacy, morbidity and subsequent pregnancyObstet Gynecol 2007 110:68-71. [Google Scholar]
[16]. Pechtor K, Richards B, Paterson H, Antenatal catastrophic uterine rupture at 32 weeks of gestation after previous B Lynch sutureBJOG 2010 117:889-91. [Google Scholar]
[17]. Sentilhes L, Gromez A, Trichot C, Ricbourg-Schneider A, Descamps P, Marpeau L, Fertility after B-Lynch suture and stepwise uterine devascularizationFertil Steril 2009 91:934e5-9. [Google Scholar]
[18]. Gerli S, Favilli A, Giardona C, Pesicoli S, Laweati E, Renzo GCD, Fertility after “only B-Lynch suture”: a case report and literatureTaiwan J Obstet Gynecol 2013 52(4):110-2. [Google Scholar]
[19]. Sentilhes L, Gromez A, Descamps P, Marpeau L, Why stepwise uterine devascularisation should be the first line conservative surgical treatment to control severe Postpartum hemorrhage?Acta Obstet Gyn Scan 2009 88(4):490-2. [Google Scholar]