Cognitive Behavioural Therapy versus Basic Health Education for Tobacco Cessation among Tobacco Users: A Randomized Clinical Trail
Mitali Raja1, Sabyasachi Saha2, Shafaat Mohd3, Ridhi Narang4, L Vamsi Krishna Reddy5, Minti Kumari6
1 Resident, Department of Public Health Dentistry, Sardar Patel Postgraduate Institute of Dental and Medical Sciences, Lucknow, India.
2 Professor and Head, Department of Public Health Dentistry, Sardar Patel Postgraduate Institute of Dental and Medical Sciences, Lucknow, India.
3 Senior Lecturer, Department of Public Health Dentistry, Sardar Patel Postgraduate Institute of Dental and Medical Sciences, Lucknow, India.
4 Senior Lecturer, Department of Public Health Dentistry, Surendera Dental College and Research Institute, Sri Ganganagar, Rajasthan, India.
5 Reader, Department of Public Health Dentistry, Sardar Patel Postgraduate Institute of Dental and Medical Sciences, Lucknow, India.
6 Senior Lecturer, Department of Public Health Dentistry, Sardar Patel Postgraduate Institute of Dental and Medical Sciences, Lucknow, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mitali Raja, Resident, Department of Public Health Dentistry, Sardar Patel Postgraduate Institute of Dental and Medical Sciences, Lucknow, India.
Phone: 91-9936619343,
E-mail: drmitaliraja@gmail.com
Introduction: Tobacco is the greatest disease-producing product which is known to man and it is a primary cause of many oral diseases and adverse oral conditions. This study was conducted to bring the behavioural changes and to educate individuals about the harmful effects of tobacco.
Method: Subjects reporting to the tobacco cessation centre of the Department of Public Health Dentistry and giving a history of tobacco consumption (smoking/smokeless) within past 30 day period were randomized into 2 groups: cognitive behavioural therapy (CBT) group (study group) and Basic health education (BHE) group (control group). Baseline evaluation (of demographic parameters, smoking/ smokeless behaviour) was done and Fagerstrom’s test for Nicotine Dependence (FTND) was used to assess subjects’ nicotine addiction levels. Follow up was done at intervals of 2 weeks and 4 weeks to assess the reduction in the mean FTND score. Appropriate statistical analysis was performed (Paired and Unpaired t-test).
Results: Of all the subjects who reported to the department, 40 subjects were recruited in the study. A majority of the subjects were males who belonged to rural areas, who had completed high school and most of them had consumed more than 10 sachets of pan masala daily, for an average of 10 years. In both CBT and BHE groups, significant reductions in mean Fagerstrom scores at 1st and 2nd follow ups from baseline and between 1st and 2nd follow ups were seen. But when both groups were compared, reductions in mean Fagerstrom scores were found to be more in CBT group than in BHE group at all time intervals, though it was not statistically significant.
Conclusion: Any intervention given to tobacco users from either CBT or BHE groups, helped the patients in quitting habit of tobacco.
Tobacco cessation, Cognitive behavioural therapy, Basic health education, Fagerstrom test for nicotine dependence (FTND)
Introduction
Tobacco was variously hailed as a gift from the gods, a miraculous cure-all for life’s physical ills, a solace to the lonely soldier or sailor, which has been presently identified as a filthy habit, a corrupting addiction and the greatest disease-producing product which is known to man [1].
Presently, India has more than 200 million tobacco consumers; only 13% of whom consume it in the form of cigarettes, whereas 54% consume it in the form of beedis and the rest consume it in raw/gutka forms. Worldwide, 85% of the tobacco which is cultivated is used in the production of cigarettes. Hence, the tobacco consumption pattern in India markedly differs from that in the rest of the world in terms of product configuration [2].
Tobacco is a risk factor for oral cancer, oral cancer recurrence, adult periodontal diseases, and congenital defects such as cleft lip and palate in children whose mothers smoke during their pregnancies [3].
Tobacco smoking has been in vogue for hundreds of years [4]. According to the National Sample Survey 52nd Round and National Family Health Survey- 2, prevalence of male tobacco use was 51.3% in 1995-1996 and it was 46.5% in 1998-1999. The prevalence of tobacco use among females was 10.3% and 13.8% in the respective years [5]. The prevalence of tobacco use is higher in rural population as compared to that in urban areas [4]. Tobacco use is one of the leading causes of preventable mortality in industrialized countries [6].
Globally, tobacco is responsible for the death of 1 in 10 adults (about 5 million deaths each year), with 2.41 (1.80-3.15) million deaths occurring in the developing countries and 2.43 (2.13-2.78) million occurring in the developed countries. A recent nationwide study done on smoking and mortality in India estimated that cigarette and beedi smoking caused about 5% of all deaths in women and 20% of all deaths in men who were aged 30-69 years, which totalled to 1 million deaths per year in India [2].
The average cost for treating patients with tobacco-related cancers was estimated to be Rs 3,50,000/- per head (at 1999 level). Reddy and Gupta updated these costs for 2002-2003, estimating the total cost for the 3 major tobacco-related diseases to be Rs. 308.33 ($6.6) billion [2].
Hence, the present study was conducted with the aim of testing the effectiveness of cognitive behavioural therapy in comparison with basic health education for tobacco cessation.
Materials and Methods
Study design
Randomized controlled trial.
Participants
This study was conducted between July 2012 and October 2012 in the Department of Public Health Dentistry of Sardar Patel Postgraduate Institute of Dental and Medical Sciences, Lucknow.
Colourful posters which advertised free tobacco quitting assistance provided by the tobacco cessation centre of the department were displayed in college OPD, pharmacies, parking area, and canteen. When smokers approached the centre for quitting tobacco, they were assessed for their eligibilities. To be eligible for the study, subjects must have reported to the recruiter that they had consumed tobacco (smoking/smokeless) within past 30 day period. In addition, participants needed to be able to attend the counseling sessions which were held at the centre as a part of the intervention and they needed to be reachable by phone, to allow follow up assessments.
They were excluded if they were enrolled in another cessation program, were using pharmacotherapy for cessation, pregnant/breastfeeding, or were diagnosed with an acute cardiac or respiratory problem or were already undergoing nicotine replacement therapy.
Over the course of 4 months, 70 subjects were screened for their eligibilities. Based on inclusion and exclusion criteria, 40 subjects were enrolled in the study.
Procedure
Enrolled subjects (n=40) provided written informed consents and completed a baseline evaluation (on demographics, smoking/smokeless behaviour). Each patient was assigned a number which was between 1 to 40 and by using a lottery method, the patients were randomly assigned to either cognitive behavioural therapy (CBT) or basic health education (BHE) groups at a ratio 1:1 (n = 20 for each group). Follow up was done at intervals of two weeks and four weeks.
Demographic information which was assessed, included age, gender, type of tobacco, number of consumption of tobacco per day. Fagerstrom’s test for Nicotine Dependence (FTND) was used to assess subjects’ nicotine addiction levels [7,8].
Cognitive behavioural therapy (CBT): Subjects who were randomized to this group were taught cognitive behavioural cessation and relapse prevention strategies and these included discussions on barriers to cessation, quitting self efficacy, previous quit attempts, risk perceptions and pros and cons of quitting. This therapy provided encouragement and support, training on educational and coping skills and it was repeated at every follow up.
Basic health education (BHE): The intervention served as a control arm, but it provided information on the harmful effects of tobacco use. Subjects were advised to think positively, keep themselves busy, remove tobacco products from his/her surroundings, listen to music and to exercise. All these motivational messages were repeated at every follow up.
Ethical clearance
Ethical clearance was obtained from institutional ethical committee of Sardar Patel Postgraduate Institute of Dental and Medical Sciences Lucknow.
Statistical Analysis
The data obtained were coded and tabulated. SPSS, version 20 was used to analyze the data. Paired and unpaired ‘t’ tests were used for intra-group and inter-group comparisons respectively and p values of < 0.05 were considered to be statistically significant.
Results
Of all the subjects who reported to the Department of Public Health Dentistry, 40 subjects were recruited in the study and they were randomly assigned to CBT and BHE groups. A majority of the subjects were males belonged to rural areas, who had completed high school and most of them had consumed more than 10 sachets of pan masala daily for an average of 10 years [Table/Fig-1].
Demographic variables of Study Participants
| S. No | VARIABLES | CBT ( n=20) n (%) | BHE (n=20) n (%) |
|---|
| AGE |
|---|
| 1. | 15-20 | 5 (25) | 2 (10) |
| 2. | 21-26 | 2 (10) | 4 (20) |
| 3. | 27-32 | 4 (20) | 7 (35) |
| 4. | 33-38 | 4 (20) | 2 (10) |
| 5. | 39-44 | 4 (20) | 2 (10) |
| 6. | 45-50 | 1 (5) | 3 (15) |
| GENDER |
| 1. | Male | 19 | 20 (100) |
| 2. | Female | 1 | 0 (0) |
| TYPE OF TOBACCO |
| 1. | Smoking | 1 (5) | 0 (0) |
| 2. | Smokeless | 15 (75) | 14 (70) |
| 3. | Both | 4 (20) | 6 (30) |
| NO. OF CONSUMPTION OF TOBACCO PER DAY |
| 1. | <10 cigarettes | 2 (10) | 2 (10) |
| 2. | > 10 cigarettes | 2 (10) | 0 (0) |
| 3. | < 10 bidis | 0 (0) | 1 (5) |
| 4. | > 10 bidis | 1 (5) | 1 (5) |
| 5. | < 10 sachets of panmasala | 3 (15) | 10 (50) |
| 6. | > 10 sachets of panmasala | 15 (75) | 9 (45) |
| 7. | < 5 paan | 1 (5) | 0 (0) |
| 8. | > 5 paan | 2 (10) | 0 (0) |
| 9. | < 1 chaini khain | 0 (0) | 2 (10) |
| 10. | > 1 chaini khaini | 0 (0) | 0 (0) |
After 1st and 2nd follow ups, following changes were observed:
There were significant reductions in mean FTND scores at 1st and 2nd follow ups from baseline and between 1st and 2nd follow ups in basic health education group. [Table/Fig-2].
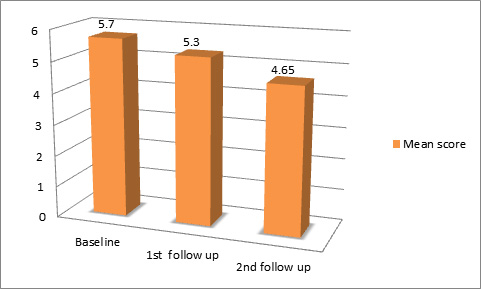
There were also significant reductions in mean scores at 1st and 2nd follow ups from baseline and between 1st and 2nd follow ups in cognitive behavioral therapy group. [Table/Fig-3].
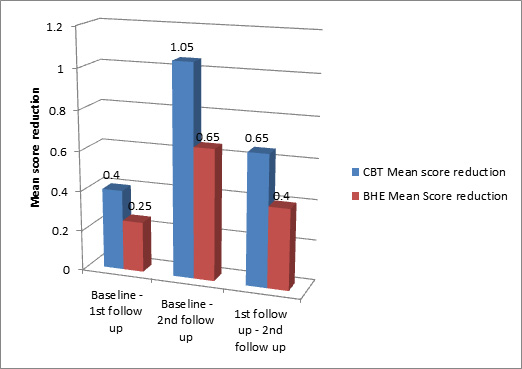
[Table/Fig-4] shows that mean score reduction was more in CBT group than in BHE group at all time intervals, but it was not statistically significant.
Comparison of mean FTND score reduction at different time interval (CBT)
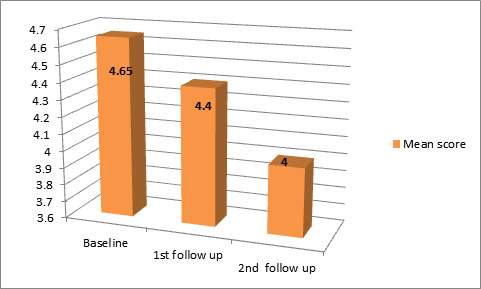
Comparison of mean FTND score reduction at different time interval (BHE)
Comparison of mean FTND score reduction in CBT and BHE at different follow-up
Discussion
Interventions that make use of CBT strategies are among the most effective treatments available for tobacco cessation; yet, they have not been tested among Indians by doing well-controlled trials. This study was done to assess and compare the effectiveness of cognitive behavioural therapy vs basic health education. Both CBT and BHE performed well, but when both the groups were compared, mean score reduction was found to be more in CBT group than in BHE group, but it was not statistically significant. It was interesting to note that mean score reduction was more in CBT group than in BHE group, despite the interventions having equivalent levels of contact. This suggested that the differences in the interventions were caused by strategies which were adopted.
A study was conducted by Robert A. Schnoll, Randi L. Rothman, and Dustin B. Wielt in 2005, where no significant difference in 30-day point-prevalence abstinence between the CBT and General Health Education conditions was detected at either 1 month (44.9% vs. 47.3%, respectively) or at 3 month (43.2% vs. 39.2%, respectively) follow up evaluations. A higher degree of quit motivation and lower cons of quitting were related to smoking cessation [9].
A study which was conducted by Catherine M. Skyes, David F. Marks in 2001 showed that at 6 months of follow up, 21 (17.2%) of 122 participants who had received therapy were abstinent and that 14 (11.5%) had reduced cigarette consumption by at least 25% of that which was seen at pre- treatment level. 6 (5.6%) of 107 participants in the control group were abstinent and none had a reduced consumption. Thus, self help CBT intervention was found to have the potential to reduce the prevalence of smoking among lower socio economic status smokers in London [10]. Another study which was conducted by Monica S. Webb, Isildinha M. Reis, Michael P. Carey, Denise Rodriguez de Ybarra and Elizabeth A. Baker in 2010 also showed that the 7- day point prevalence abstinence (ppa) was significantly greater in the CBT than in the GHE condition at the end of counselling (51% vs. 27%), at 3 months (34% vs. 20%), and at 6 months (31% vs. 14%). Thus, intensive group CBT smoking cessation interventions were found to be efficacious among African American smokers [11].
Though CBT performed better than BHE, when both the groups were compared, mean score reduction was found to be more in CBT than in BHE, but it was found that any intervention which was given to tobacco users from either CBT or BHE groups, was helpful to the patients in quitting the habit of tobacco. The only thing that was important was motivating the patient. If the patient got motivated, he/she could easily quit the habit of tobacco.
[1]. Garg Dipika, Narula Sidharth, Jindal Varun, A cigarette a day, keeps the doctor in payIndian Journal of Dental Sciences 2012 4(2):128-30. [Google Scholar]
[2]. Rao V, Chaturvedi P, Tobacco and health in IndiaIndian Journal of Cancer 2010 47(1):53-8. [Google Scholar]
[3]. Petersen PK, Tobacco and Oral Health – the role of the World Health OrganizationOral Health Prev Dent 2003 1:309-15. [Google Scholar]
[4]. Reddy KS, Gupta PK, Tobacco Control in India 2004 :1-378. [Google Scholar]
[5]. Rani M, Bonu S, Jha P, Nguyen SN, Jamjoum L, Tobacco use in India: Prevalence and predictors of smoking and chewing in a national cross-sectional household surveyTobacco Control 2003 129(4):1-8. [Google Scholar]
[6]. Gonseth S, Abarca M, Madrid C, Cornuz J, A pilot study combining individual based smoking cessation counselling, pharmacotheraphy, and dental hygiene interventionBMC Public Health 2010 10:1-5. [Google Scholar]
[7]. Ebbert JO, Patten CA, Schroeder DR, The Fagerstrom Test for Nicotine Dependence-Smokeless Tobacco (FTND-ST)Addictive Behaviors 2006 31(9):1716-21. [Google Scholar]
[8]. Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KL, The Fagerstrom Test for Nicotine Dependence: a revision of the Fagerstrom Tolerance QuestionnaireBritish Journal of Addictions 1991 86:1119-27. [Google Scholar]
[9]. Schnoll RA, Rothman RL, Wielt DB, A randomized pilot study of cognitive-behavioral therapy versus basic health education for smoking cessation among cancer patientsAnn Behav Med 2005 30(1):1-11. [Google Scholar]
[10]. Skyes CM, Marks DF, Effectiveness of cognitive behaviour therapy self help programme for smokers in London, UKHealth Promotion International 2001 16(3):255-60. [Google Scholar]
[11]. Webb MS, Reis IM, Carey MP, Ybarra DR, Baker EA, Cognitive–behavioral therapy to promote smoking cessation among African American smokers: A randomized clinical trialJournal of Consulting and Clinical Psychology 2010 78(1):24-33. [Google Scholar]