An Anatomical Variation of the Lesser Occipital Nerve in the “Carefree part” of the Posterior Triangle
Swamy Ravindra S1, Srinivasa Rao Sirasanagandla2, Satheesha B Nayak3, Mohandas Rao KG4, Jyothsna Patil5
1 Lecturer, Department of Anatomy, Melaka Manipal Medical College (Manipal Campus), Manipal University, Madhav Nagar, Manipal, Karnataka State, India.
2 Lecturer, Department of Anatomy, Melaka Manipal Medical College (Manipal Campus), Manipal University, Madhav Nagar, Manipal, Karnataka State, India.
3 Professor and Head, Department of Anatomy, Melaka Manipal Medical College (Manipal Campus), Manipal University, Madhav Nagar, Manipal, Karnataka State, India.
4 Professor, Department of Anatomy, Melaka Manipal Medical College (Manipal Campus), Manipal University, Madhav Nagar, Manipal, Karnataka State, India.
5 Lecturer, Department of Anatomy, Melaka Manipal Medical College (Manipal Campus), Manipal University, Madhav Nagar, Manipal, Karnataka State, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Mr. Srinivasa Rao Sirasanagandla, Lecturer, Department of Anatomy, Melaka Manipal Medical College (Manipal Campus), Manipal University, Madhav Nagar, Manipal, Karnataka State-576104, India.
Phone: +91 820 2922644,
E-mail: Seenaih.anat@gmail.com
The occurrence of the lesser occipital nerve (LON) at an anomalous location in the “carefree part” within the posterior triangle has been seldom reported in the literature. We are reporting a rare case of location of the LON in the “carefree part” of the posterior triangle, in a 55-year-old formalin embalmed male cadaver. LON, after emerging from the posterior margin of the sternomastoid muscle (SM), ran obliquely towards the trapezius muscle. Here, it hooked around the unusual separated muscle fasciculus of the trapezius, 7.5 cm below the superior nuchal line. Further, LON gave contributions to spinal accessory nerve (SAN); one deep into the SM and another one in the posterior triangle. The knowledge on the unusual location and course of the LON and its contribution to the SAN is significantly important while an anaesthetic blockade is being performed for the management of a cervicogenic headache and a super selective radical neck dissection.
Lesser occipital nerve, Spinal accessory nerve, Cervicogenic headache, Radical neck dissection
Case Report
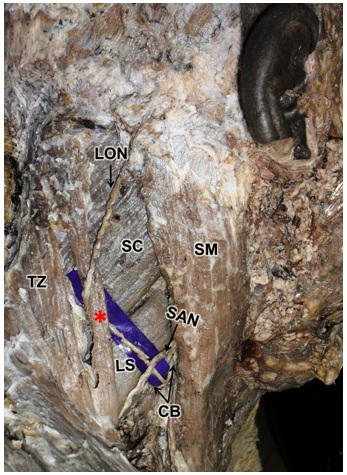
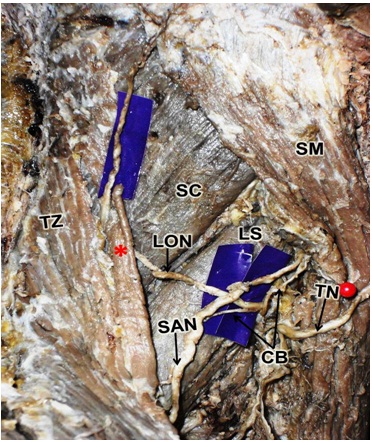
During regular dissections, we came across an anatomical variation of the LON. It was noted in a 55-year-old male cadaver of south Indian origin, which was donated to the Manipal University, for the purpose of anatomical examination, medical education and research. The observed variation was unilateral and it was noted in the right posterior triangle. After emerging from the posterior border of the SM, it wound around the SAN and coursed upwards and backwards obliquely over the levator scapulae, across the occipital area of the posterior triangle. Then, it passed deep to the sufficiently large sized unusual separated muscle fasciculus of the trapezius and hooked around this fasciculus in a fascial cleft, 7.5 cm below the superior nuchal line. After winding around this muscle fasciculus, it changed its direction and coursed forwards across the upper part of the occipital area and divided into branches to supply the scalp [Table/Fig-1]. Further, at the posterior border of SM, it gave two communicating branches to SAN. One of these branches joined the SAN in the posterior triangle. The other branch recurred to join the SAN deep in the SM [Table/Fig-2].
Dissection of right side neck showing the anomalous location of the lesser occipital nerve (LON) in the “carefree part” of the posterior triangle. Note the LON is hooking around the unusual muscle fasciculus of the trapezius muscle (Asterisk). (SAN: spinal accessory nerve, CB: communicating branches from the LON to SAN, SM: sternomastoid, TZ: trapezius, SC: splenius capitis, LS: levator scapulae).
Closer view of dissection of right side neck showing the communicating branches (CB) from the lesser occipital nerve (LON) to spinal accessory nerve (SAN). Note one of these branches joined the SAN deep to the sternomastoid muscle (SM) whereas another branch joined in the posterior triangle. (Asterisk: Unusual muscle fasciculus of the trapezius, TZ: trapezius, SC: splenius capitis, LS: levator scapulae, TN: transverse cutaneous nerve).
Discussion
The term, “carefree part” of the posterior triangle, referred to as the occipital area in the posterior triangle, is situated immediately above the SAN [1]. The LON is an ascending sensory branch of the cervical plexus. Rarely, LON is found to course through the “carefree part” [2]. Duplication and triplication are the other reported variations of the origin of LON [2,3]. Furthermore, authors have described the role of anatomical variations of the LON in cervicogenic headaches and facial rejuvenation surgeries [2–4]. According to the classical text book description, no significant structures are present in this area. We observed the unusual course of LON in the “carefree part” of the posterior triangle. Lucas et al., [2] have reported a similar case in which LON was passing through the “carefree part”. In a study, Pillay et al., [5] found presence of LON in the “carefree part” in 2% of foetal specimens. It has been demonstrated that an unusual location of LON in “carefree part” may result in neck pain, due to its stretching and compression. In addition, it has been suggested that an unusual position of the LON also plays a vital role in the development of cervicogenic headaches [2].
In the present case, LON, after emerging from the posterior margin of the SM, coursed over the levator scapule to reach the anterior border of trapezius muscle. Here, it hooked around a sufficiently large sized unusual separated trapezius muscle fasciculus. Madhavi and Holla [3] have reported a case of triplication of LON; one of its three branches pierced the trapezius, 3.5 cm below the superior nuchal line. But contrary to their report, in our case, LON pierced the trapezius, 7.5 cm below the nuchal line. The possible roles of C1, C2, or C3 root fibres, the occipital nerves, the uncovertebral joints, and the vertebral artery have been implicated in the causation of cervicogenic headaches [6]. Lucas et al., [2] demonstrated that LON is involved in the causation of cervicogenic headaches. In a study, Dash et al., [7] demonstrated that the unusual location of LON may be crucial while using anaesthetic blockades in migraine pain relief. Further, they demonstrated that the proximal site may be an effective site for the blockage of the LON.
SAN may receive contribution from the cervical plexus. Most of these contributions come from the C2, both C2 and C3, or C3 spinal nerves [8]. In a study, Lee et al., [9] found the contributions from C2 in 53.1% cases; from C2 and C3 in 38.1% cases and from C3 in 8.8% cases. In all the reported cases, SAN received these contributions deep in the SM [8,9]. For the first time, we are reporting the presence of communicating branch in the posterior triangle. In super selective radical neck dissection, the SAN and branches of the cervical plexus are usually preserved, in order to minimize the neck pain and tightness [10]. In a study done by Jong-Lyel et al., they concluded that preservation of the cervical plexuses and SAN during neck dissections not only reduced the neck morbidity but that it also improved the mental status and quality of life [11]. The neck pain may be neuropathic or myofascial in origin. Usually, the post-operative neuropathic pain is caused by the persistent excitability of the damaged nerve endings [12]. On other hand, post-operative myofascial pain is caused by SAN dysfunction [13,14]. Contributions of LON to the SAN consist of fibres from the C2 and C3. Any injury which is caused to these fibres during radical neck dissections may cause SAN dysfunction and it may consequently result in myofascial pain. The knowledge on the occurrence of unusual location of communicating branch from the LON to SAN, which has been reported in the present case, may be clinically important during radical neck dissections, for preventing injuries to the SAN and cervical plexus branches.
Conclusion
Though the anomalous location of the LON in “carefree part” of the posterior triangle has been reported earlier, its occurrence is very rare. Further, the LON which has been reported here is unique in its position and the distance at which it hooked round the unusually separated trapezius muscle fasciculus. The occurrence of communicating branch of LON to SAN in the posterior triangle is also remarkable while super selective radical neck dissections are being performed.
[1]. Basmajian JV, Slonecker CE, Posterior triangle of the neckIn: Grant’s method of anatomy. A clinical problem-solving approach 1989 11th editionBaltimoreLippincott Williams and Wilkins [Google Scholar]
[2]. Lucas GDA, Laudanna A, Choppard RP, Raffaelli Jr E, Anatomy of the lesser occipital nerve in relation to cervicogenic headacheClin Anat 1994 7:90-96. [Google Scholar]
[3]. Madhavi C, Holla SJ, Triplication of the lesser occipital nerveClin Anat 2004 17:667-71. [Google Scholar]
[4]. Berry M, Bannister LH, Standring SM LH, Berry MM, Collins P, Dyson M, Nervous system. In: Williams PL, Bannister editorsGray’s anatomy 1995 38th editionEdinburghChurchill Livingstone [Google Scholar]
[5]. Pillay P, Partab P, Lazarus L, Satyapal KS, El nervio occipital menor en fetosInt. J. Morphol 2012 30:140-144. [Google Scholar]
[6]. Fredriksen TA, Hovdal H, Sjaastad O, Cervicogenic headache: clinical manifestationCephalalgia 1987 7:147-60. [Google Scholar]
[7]. Dash KS, Janis JE, Guyuron B, The lesser and third occipital nerves and migraine headachesPlast Reconstr Surg 2005 115:1752-60. [Google Scholar]
[8]. Soo KC, Hamlyn PJ, Pegington J, Westbury G, Anatomy of the accessory nerve and its cervical contributions in the neckHead Neck Surg 1986 9:111-15. [Google Scholar]
[9]. Lee SH, Lee JK, Jin SM, Kim JH, Park IS, Chu HR, Anatomical variations of the spinal accessory nerve and its relevance to level IIb lymph nodes OtolaryngolHead Neck Surg 2009 141:639-44. [Google Scholar]
[10]. Roh JL, Yoon YH, Kim SY, Park CI, Cervical sensory preservation during the neck dissectionOral Oncol. 2007 43:491-98. [Google Scholar]
[11]. Jong-Lyel R, Yeo-Hoon Y, Sang YK, Chan IP, Cervical sensory preservation during neck dissectionOral Oncology 2007 43:491-98. [Google Scholar]
[12]. Zimmermann M, Pathobiology of neuropathic painEur J Pharmacol. 2001 429:23-37. [Google Scholar]
[13]. van Wilgen CP, Dijkstra PU, van der Laan BF, Plukker JT, Roodenburg JL, Morbidity of the neck after head and neck cancer therapyHead Neck 2004 26:785-91. [Google Scholar]
[14]. Nori S, Soo KC, Green RF, Strong EW, Miodownik S, Utilization of intraoperative electroneurography to understand the innervation of the trapezius muscleMuscle Nerve 1997 20:279-85. [Google Scholar]