Behaviour of Disc Oedema During and After Amiodarone Optic Neuropathy: Case Report
Med. Alejandro Martínez-LóPez-Portillo1, Bertha O. Martínez-Gamero2, Jibran Mohamed-Noriega3, Med. Humberto Cavazos-Adame4, Med. Jesús Mohamed-Hamsho5
1 Professor, Department of Ophthalmology, Glaucoma and Optic Nerve Diseases Clinic, Hospital Universitario “Dr. José Eleuterio González”, Universidad Autónoma de Nuevo León, Monterrey, Nuevo León, México.
2 Postgraduate Student, Department of Ophthalmology, Hospital Universitario “Dr. José Eleuterio González”, Universidad Autónoma de NuevoLeón, Monterrey, Nuevo León, México.
3 Professor, Department of Ophthalmology, Glaucoma and Optic Nerve Diseases Clinic, Hospital Universitario “Dr. José Eleuterio González”, Universidad Autónoma de NuevoLeón, Monterrey, Nuevo León, México.
4 Professor, Department of Ophthalmology, Pediatric Ophthalmology and Strabismus Clinic, Hospital Universitario “Dr. José Eleuterio González”, Universidad Autónoma de NuevoLeón, Monterrey, Nuevo León, México.
5 Professor and Head, Department of Ophthalmology, Glaucoma and Optic Nerve Diseases Clinic, Hospital Universitario “Dr. José Eleuterio González”, Universidad Autónoma de NuevoLeón, Monterrey, Nuevo León, México.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Med. Alejandro Martínez López-Portillo, Professor, Department of Ophthalmology, Glaucoma and Optic Nerve Diseases Clinic, Hospital Universitario “Dr. José Eleuterio González”, Universidad Autónoma de Nuevo León, Monterrey, Nuevo León, México. Address: Av. Madero y Gonzalitos s/n Col. Mitras Centro, Monterrey, N. L. México C.P. 64460.
Phone: +52 (81) 83469259, +52 8182539010,
E-mail: amtzlp@prodigy.net.mx
A 73-year-old woman with atrial fibrillation treated with Amiodarone presented with Optic Disc oedema in right eye (OD). Using Optical Coherence Tomography (OCT) we describe the impact of this neuropathy on Retinal Nerve Fibre Layer (RNFL). At diagnosis RNFL average was of 188 μm OD and 77 μm in the left eye (OS), six months after discontinuation of the drug decreased to 40 μm in OD and 76 μm in OS. The RNFL average of OD presented a transient increase during the acute oedema that returned to normal levels during the first month after discontinuation of the drug and fell dramatically to 44 μm at the second month and 40 μm at the sixth month. We show there is axonal loss after amiodarone-associated optic neuropathy measured with OCT. The OCT may be used in these patients to document changes in RNFL in the follow-up.
Optic coherence tomography, Optic atrophy, Toxic neuropathy
Case Report
A 73-year-old woman with no previous ocular history presented with one month of decreased vision in her right eye (OD). Her past medical history included atrial fibrillation, heart failure NYHA III, and controlled hypertension. Her current medications were Losartan 100 mg q.d., Xarelto 5 mg q.d., and Amiodarone 200 mg t.i.d. for the past 6 months. The patient underwent ophthalmologic examination, including Best-Corrected Visual Acuity (BCVA), Ishihara pseudoisochromatic colour vision plate testing, and slit-lamp examination, including Intra-Ocular Pressure (IOP) with Goldman tonometry, and fundoscopy. The BCVA in the OD was counting fingers, and 20/20 in the left eye (OS). The patient could not distinguish the colour test plates with OD and showed a Relative Afferent Pupillary Defect (RAPD); OS normal. Slit-lamp examination revealed cornea verticillata, normal IOP and shallow anterior chamber in both eyes. Fundus examination revealed hyperaemic and swollen optic disc with haemorrhages in the OD and cup-disc ratio of 0.30 in the OS [Table/Fig-1].
Right Optic nerve at moment of diagnosis of right optic neuropathy associated with amiodarone. A OCT: oedema, B: Photograph of disc oedema, and C: Goldman perimetry: right central scotoma
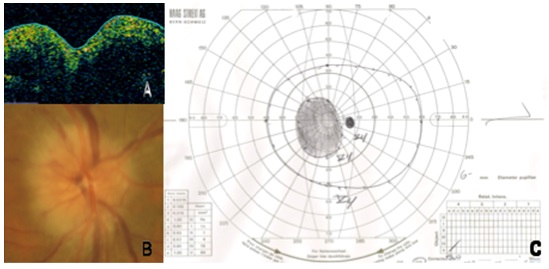
Goldmann Perimeter (940; Haag-Streit AG, Liebefeld Switzerland) showed marked central scotoma in the OD [Table/Fig-1]; OS was normal. Optic coherence tomography (OCT; Stratus-OCT™, Carl-Zeiss Medictec, Inc., Dublin, CA) of the optic nerve showed increased RNFL average in the OD with 188 μm and 77 μm in the OS [Table/Fig-2]. The erythrocyte sedimentation rate was normal. A diagnosis of unilateral amiodarone-associated optic neuropathy in OD was made, and the cardiologist discontinued the medication.
Right optic nerve 6 month post discontinuation of amiodarone. A: OCT: decreased RNFL fibre, B: photograph of optic nerve head atrophy and C:Goldman perimetry: inferior altitudinal defect
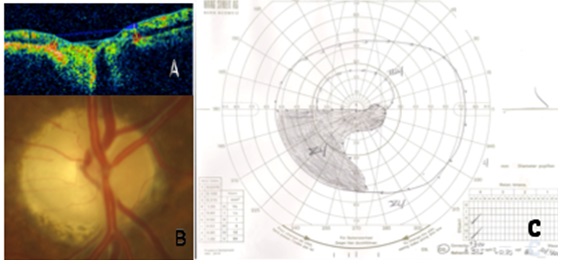
After 6 months the BCVA in OD improved to 20/400, the RAPD persisted, and the Goldmann perimetry showed an inferior altitudinal defect. Fundoscopic examination of the OD showed resolution of optic disc oedema and a pale colour of the optic nerve [Table/Fig-2], and the RNFL average was 40 μm [Table/Fig-3]; OS remained normal.
Right optic nerve 6 month post discontinuation of amiodarone. A: OCT: decreased RNFL B: Photograph of optic nerve head atrophy and C: Goldman perimetry: inferior altitudinal defect
| Right eye | Left eye | Difference OD vs OS |
|---|
| RNFL Average (absolute values, μm) |
| Baseline | 188 | 77 | +111 |
| 1 month after discontinuation of amiodarone | 72 | 76 | -4 |
| 2 month after discontinuation of amiodarone | 44 | 79 | -35 |
| 4 month after discontinuation of amiodarone | 41 | 74 | -33 |
| 6 months after discontinuation of amiodarone | 40 | 76 | -36 |
Discussion
Amiodarone toxicity can involve many organs and tissues including lungs, thyroid, skin, nervous system, liver, and eye. Ocular toxicity includes corneal micro deposits (90%), halo vision (<5%), and optic neuropathy (0.0009% to 2%), and may appear on average 6.5 weeks to 6 months after starting the drug at a daily dose of 200 mg [1–6]. Almost 30% of amiodarone-associated optic neuropathies have clinical features similar to Nonarteritic Anterior Ischemic Optic Neuropathy (NAION) [6].
In our patient it is difficult to distinguish between amiodarone toxicity and NAION because of her past medical history of atrial fibrillation, heart failure, and hypertension. Macaluso et al., proposed clinical features to distinguish amiodarone-associated optic neuropathy from NAION on the basis that insidious onset (months), visual acuity from 20/20 to 20/200, bilateral ocular involvement, and resolution of disc oedema in months are often characteristics present with the use of amiodarone [7]. On the other hand, NAION typically present with a rapid onset (days to weeks), visual acuity of 20/20 to no light perception, resolution of disc oedema in weeks, and bilateral involvement (rarely simultaneous) [7]. Years later, Purvin et al., expanded these features and divided patients in groups of unilateral or bilateral disc oedema with typical or atypical features of NAION [8]. Atypical features being insidious onset of symptoms, mild optic nerve dysfunction, and generous cup–disc ratio in the fellow eye [8]. The presence of atypical features supports the association with amiodarone. Furthermore Passman et al. reported criteria for diagnosing optic neuropathy, the association with amiodarone, and the level of diagnostic certainty [9] [Table/Fig-4]. According to the ophthalmic features presented by Macaluso et al., Purvin et al., and Passman et al., our patient has an optic neuropathy associated with amiodarone.
Passman et al., criteria for completeness of reporting for possible amiodarone-associated optic neuropathy cases
| Data Elements | Scoring (based on number of elements reported) |
|---|
| Optic neuropathy diagnosis (1 point for each element) | Optic disc oedema, visual field defect, color vision abnormalities, optic disc atrophy, optic disc haemorrhages, afferent pupillary defect, intracranial hypertension, and change in visual acuity/subjective blurring of vision | Complete (6-8) Partially complete (3-5) Incomplete (<3) |
| Association with amiodarone (1 point for each element) | Dose, duration of treatment, duration of treatment before presentation, other simultaneous drug therapy, outcome post- discontinuation, change in visual acuity after initiation of amiodarone | Complete (5-6) Partially complete (3-4) Incomplete (<3) |
| Diagnostic certainty | Completeness of information provided and the diagnosis given by the reporting physician | Probable (patient was diagnosed with optic neuropathy/neuritis) Possible (patient had one or more features suggestive of optic neuropathy/neuritis) Incomplete (no information is present on the final diagnosis or the presence or absence of features suggestive of optic neuropathy /neuritis) |
The prognosis of this type of neuropathy is very diverse. Passman et al., reported improvement in visual acuity in 58% [9] while Kervinen et al., reported permanent visual loss [2]. Six months after discontinuing amiodarone our patient’s right Goldman perimetry improved from central scotoma to inferior altitudinal defect, and her BCVA in the OD improved from counting fingers at 1 meter to 20/400.
In an effort to explain the pathophysiology of the disease Purvin et al., and Mansour et al., reported multiple lamellar inclusion bodies within large axons of the optic nerve without axonal loss [8,10]. In contrast to the absence of axonal loss in amiodarone toxicity Sühs et al., studying demyelinating optic neuritis, showed that RNFL thinned to levels greater than 10 μm below the healthy eye after a transient oedema that resolved within the first two months after disease onset [11]. Similar to Sühs et al., our patient’s RNFL showed an important elevation at baseline that returned to normal values after one month. Subsequently 2 months after discontinuation of the drug the RNFL reached 44 μm and remained almost at the same thickness until the last examination at 6 months. During the 6 months follow-up the RNFL decreased 148 μm [Table/Fig-2,3].
Van Elmbt et al., reported axonal loss and optic nerve atrophy after resolution of amiodarone-associated optic neuropathy with OCT [12]. However, the behaviour of RNFL through out the entire episode of oedema was not described. With this case, we show the variations of RNFL during and after amiodarone-associated optic neuropathy. We show there is transient elevation in RNFL during the first month with subsequent axonal loss. We recommend follow-up visits every year with an ophthalmologist for screening patients using amiodarone. During these examinations, OCT of the optic nerve may be performed to document oedema or thinning in RNFL.
[1]. Mindel JSMP, Amiodarone and optic neuropathyAmerican Heart Journal 2008 156(3):411-3. [Google Scholar]
[2]. Kervinen MMP, Bilateral optic neuropathy and permanent loss of vision following treatment with amiodaroneJournal of Cardiovascular Pharmacology 2013 :1 [Google Scholar]
[3]. Garret SNM, Kearney John J, Schiffman Jade S, Amiodarone Optic NeuropathyJournal of Clinical Neuro-ophthalmology 1988 8(2):105-10. [Google Scholar]
[4]. Nagra PK, Foroozan R, Savino PJ, Castillo I, Sergott RC, Amiodarone induced optic neuropathyBritish Journal of Ophthalmology 2003 87:420-2. [Google Scholar]
[5]. Mäntyjärvï MM, Tuppurainen Kaija Ikäheimo Kirsi Ocular Side Effects of AmiodaroneSurvey of ophthalmology 1998 42(4):360-5. [Google Scholar]
[6]. Johnson LNM, Krohel GBM, Thomas ERM, The Clinical Spectrum of Amiodarone- Associated Optic NeuropathyJournal of the National Medical Association 2004 96(11):1477-91. [Google Scholar]
[7]. Macaluso DCM, Shults William T, Fraunfelder Frederick T, Features Amiodarone Optic NeuropathyAmerican Journal of Ophthalmology 1999 127(5):610-2. [Google Scholar]
[8]. Purvin VM, Kawasaki Aki, Bourruat Francois-Xavier Optic Neuropathy in Patients Using AmiodaroneArchives of Ophthalmology 2006 124:696-701. [Google Scholar]
[9]. Passman RS, Amiodarone-associated Optic Neuropathy: A Critical ReviewThe American Journal of Medicine 2012 125:. 447-53. [Google Scholar]
[10]. Mansour AM, Puklin James E, O’Grady Richard, Optic Nerve Ultrastructure Following AmiodaroneJournal of Clinical Neuro-ophthalmology 1988 8(4):231-7. [Google Scholar]
[11]. Sühs KW, Retinal Nerve Fibre Layer Thinning in Patients with Clinically Isolated Optic Neuritis and Early Treatment with Interferon-BetaPlos One 2012 7(12):e51645 [Google Scholar]
[12]. Van Elmbt G, Andris C, Collignon N, Neuropathies Optiques Liées á L’amiodarone- A propos de deux casBull. Soc. belge Ophtalmol 2007 (303):73-8. [Google Scholar]