Retinal Arterial Obstruction-still Remains an Enigma
Anupama Kakhandaki1, Charushila Gejapati2, Preetam B. Patil3, Vivekanand S.G.4
1 Professor, Department of Ophthalmology, Shri Dharmasthala Manjunatheshwara College of Medical Science and Hospital, Sattur, Dharwad, Karnataka, India.
2 Assistant Professor, Department of Ophthalmology, Shri Dharmasthala Manjunatheshwara College of Medical Science and Hospital, Sattur, Dharwad, Karnataka, India.
3 Associate Professor, Department of Radiology, Shri Dharmasthala Manjunatheshwara College of Medical Science and Hospital, Sattur, Dharwad, Karnataka, India.
4 Chief Cardiologist, Department of Cardiology, SDM-Narayana Hrudayalaya, Dharwad, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anupama Kakhandaki, Professor, Department of Ophthalmology, SDM College of Medical Sciences and Hospital, Sattur, Dharwad, Karnataka-580009, India.
Phone: +91 9972309657,
E-mail: anupamadesaiblr@gmail.com
Retinal artery obstruction is an ocular emergency which usually carries a poor visual prognosis. Restoration of fruitful vision depends on the underlying cause and the immediate start of treatment. However, none of the known treatment modalities, have so far, assured positive results consistently. Retinal artery obstructions are forewarners of possible systemic emboli/infarcts. Thus, it is imperative for ophthalmologists to identify the disease and get a thorough systemic examination done, preferably by a cardiologist, so as to prevent serious systemic morbidity. It is to be noted that in our case report, in spite of having delayed presentations, both the patients were subjected to thorough cardiovascular examinations. In clinical practice, patients are not further investigated, once the chances of visual recovery are bleak. Our case report highlights the importance of subjecting these patients to complete cardiovascular work ups, even though a poor visual recovery is expected, which can lead to detection of various cerebrovascular infarcts.
Amaurosis Fugax, Retinal artery obstruction, Carotid Angiography
Case Reports
Case I
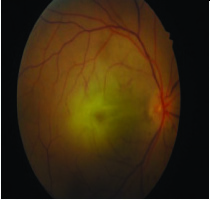
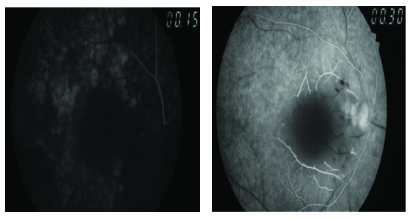
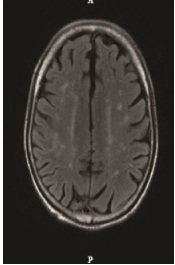
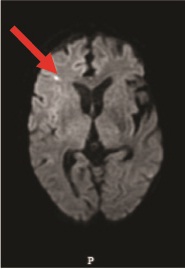
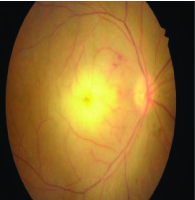
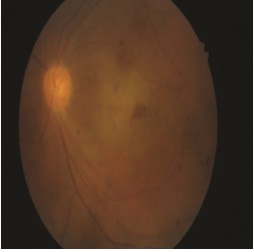
A 58-year-old male presented with complaint of sudden loss of vision in the right eye, of 15 days duration. He gave a history of transient obscuration of vision in the right eye for few seconds, two weeks prior to this episode. It was associated with weakness of the left upper limb. There was no history of associated headache, jaw claudication or any clinical symptom which was suggestive of giant cell arteritis. On ocular examination, the visual acuity was found to be absence of perception of light in the right eye and 20/120 in left eye, which had improved to 20/20 with pinhole. There was a relative afferent pupillary defect in the right eye. Anterior segment examination was unremarkable, with normal intraocular pressures being seen in both eyes. Dilated fundus examination of right eye showed mild disc oedema, absence of typical cherry red spot, macular oedema and mild arteriolar narrowing with cattle trucking of blood column [Table/Fig-1]. Left eye fundus revealed only mild arteriolar narrowing. On fundus fluorescein angiography, right eye showed a delayed filling of choroidal vessels, narrowing of the arterioles, an enlarged foveal avascular zone [Table/Fig-2,3] and cattle trucking of the blood column. No abnormality was detected in the left eye. The patient underwent a thorough systemic examination, which included a cardiovascular examination. He was detected with systemic hypertension and was started on anti-hypertensives. He was subjected to systemic investigations, which included an electrocardiogram, which was found to be normal, ESR, which was normal, complete lipid profile, which showed raised total cholesterol, LDL and triglycerides. Colour Doppler of carotids showed calcified plaques which measured two mm each, in the bulb of the carotids. However, there was no evidence of a haemodynamically significant stenosis. Patient underwent plain MRI study of the brain, which showed an acute lacunar infarct in the right frontal lobe [Table/Fig-4,5]. He was followed up after one week and the right eye’s fundus showed the presence of two new superficial haemorrhages which were adjacent to the disc [Table/Fig-6]. As the vision in his right eye had improved to hand movements, these haemorrhages could be explained as caused by dislodgement of the emboli. After two months, patient developed optic atrophy in the right eye.
Fundus photograph showing Stage III CRAO in right eye
FFA showing enlarged FAZ in right eye
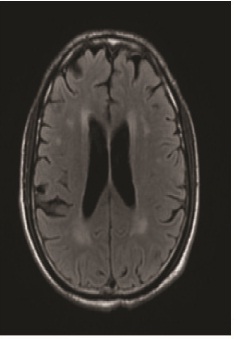
MRI Scan showing old multiple lacunar infarcts
MRI Scan showing acute infarct in right frontal lobe
After 1 week, Fundus photograph showing two new hemorrhages superotemporally, in the right eye
Case II
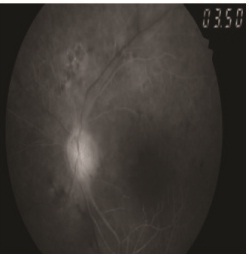
A 78-year-old male presented with sudden loss of vision in the left eye, of one week’s duration. There was no history of headache, jaw claudication or scalp tenderness, which were suggestive of giant cell arteritis. Patient gave a history of a similar episode which had occurred one month back, with sudden loss of vision in left eye, which had lasted for one hour, followed by complete visual recovery. On clinical examination, the visual acuity was found to be 20/60 in the right eye, which improved to 20/40 with pinhole.Visual acuity in the left eye was hand movements close to face, with accurate projection of rays. On slit lamp examination, left eye showed presence of nebular grade opacity in the cornea, which measured 10mm horizontally and 5 mm vertically, which covered half of the pupillary area. Both eyes had grade II nuclear sclerosis with pseudo exfoliation. Intraocular pressures were within normal limits. Dilated fundus examination of the right eye showed one isolated plaque in the superotemporal artery, 1 disc diameter away from the disc. The left eye fundus showed mild haziness of media, caused by corneal and lenticular opacifications. The disc appeared to be normal and there was oedema of the retina between disc and fovea [Table/Fig-7]. Few superficial haemorrhages were seen adjacent to the disc. Fundus fluorescein angiography showed a delayed filling of choroidal vessels and an enlarged foveal avascular zone [Table/Fig-8,9]. On doing carotid angiography, it was seen that there was a 100% block of the left vertebrobasilar artery and normal flow on right side [Table/Fig-10,11]. Carotid Doppler showed plaques in internal carotid artery, on both sides. MRI scan of the brain showed multiple old lacunar infarcts [Table/Fig-12]. A conservative line of treatment was started by the cardiologist. Patient was given Tablet Atorvastatin, 20 mg OD and Tablet Aspirin, 100 mg, OD. No visual improvement was seen at subsequent follow ups, two months later.
Fundus photograph showing macular edema with few hemorrhages in left eye
FFA showing delayed filling (view is not clear due to corneal opacity)
FFA showing a marginally enlarged FAZ
Carotid angiography showing normal blood flow in vertebrobasilar artery on right side

Carotid angiography showing complete block of vertebrobasilar artery on left side

MRI scan of Brain showing multiple lacunar infarcts
Discussion
Retinal arterial obstructive disease usually presents with sudden loss of vision and it is the most dramatic event which is seen by an ophthalmologist [1]. It was first described by Von Graefe [2]. This condition is not only important from the point of visual outcome and ocular complications, but also due to its increased association with systemic morbidity and mortality [2].
Stages of CRAO
Stage I: Incomplete CRAO – diminution of vision, but no complete loss of vision; retinal oedema and cherry red spot are present. FFA shows a delayed but not a completely interrupted blood flow.
Stage II: Subtotal central retinal artery obstruction – A highly reduced visual acuity with a small island of vision. A distinct retinal oedema with cherry red spot and cattle truck appearance is present. FFA shows a distinct delay in arterial blood flow.
Stage III: Total central retinal artery obstruction – There is no perception of light. Massive retinal oedema and cattle truck appearance are present and there is absence of cherry red spot. FFA shows no blood flow in the premacular arterioles (in some cases, there is an additional interruption of choroidal blood flow).
The management of acute retinal arterial obstructive disease has not changed over the past three decades, though local intra-arterial fibrinolysis has been advocated for the prevention of recurrences [2]. The visual acuity at the time of presentation and duration of the visual impairment appear to correlate with the visual prognosis [3]. In spite of conducting trials on treatment of CRAO by using various treatment modalities, in different parts of the world, the visual outcomes were similar. This points towards a lack of efficacy of present standard treatment which is given in acute CRAO [4]. As both the patients who came to us, did not present early (within 24 hours), none of the standard treatment modalities [5] were tried [Table/Fig-13].
Standard treatment protocol followed for CRAO within 48 hours of occlusion
| Standard treatment protocol | |
| Ophthalmic management | Non-Ophthalmic management |
| In Emergency department (By non-ophthalmologist) | 1. Management of co-existing diseases such as Hypertension, Diabetes Mellitus and Hyperlipidemia |
| 1. Lie Patient flat | |
| 2. Ocular massage | 2. Dietary advice for the above conditions |
| 3. Intravenous Acetazolamide, 500 mg stat | |
| 4. Inhalation of Carbogen (5%CO2,95%O2) | 3. Oral Aspirin |
| By Ophthalmologist | |
| 1. Anterior chamber paracentesis | |
| 2.Intraophthalmic artery fibrinolysis followed by 2 days of heparinisation | |
| 3. Days of heparinisation | |
| (Under hospitalization and expert supervision) |
Interestingly, both the patients who presented to us gave history of amaurosis fugax which was seen a few days prior to occurrences of the acute episodes of CRAO. Such a history of amaurosis fugax, not only forewarns about an impending retinal arterial occlusion, but it also forewarns about the possibility of a systemic ischaemic attack, which can be life threatening. Hence, it is mandatory for every patient who suffers from CRAO to be thoroughly evaluated for cardiovascular abnormalities [6]. A preceding history of amaurosis fugax is strongly suggestive of an embolic origin of occlusion [7]. Emboli are visible in the retinal arteries in 20-40% of the eyes with CRAO. Cholesterol emboli are often small and they seldom cause complete obstructions. Calcific emboli are less common, but they are larger and cause severe obstructions. These usually arise from cardiac valves. However, Hayreh pointed out a few misconceptions regarding CRAO, such as, (a) absence of any abnormality on carotid Doppler and echocardiography always rules out that those sites are embolisms, (b) absence of an embolus in the retinal artery means that the occlusion was not caused by an embolus [8].
Conclusion
Unlike western countries, people in rural part of the Indian sub-continent have poor awareness about most of the major ocular emergencies, which include central retinal artery obstructions. In both the cases which have been described, it can be observed that the symptoms of amaurosis fugax were totally ignored and that the duration of presentation was more than two weeks after the onset of the problem. This case report highlights the utmost need to increase awareness in the population in this regard, so as to prevent systemic morbidity and mortality. Irrespective of the duration of presentation, all patients with retinal artery obstructions should be subjected to thorough systemic investigations like complete lipid profile, Carotid Doppler and echocardiography. MRI of Brain and Carotid angiography may also be advised, if required. Both the patients who have been reported here, did not regain any fruitful vision, but the systemic investigations were able to detect various cardiovascular and cerebral lesions. Both patients were cautioned regarding risk of similar episode in the other eye or cerebrovascular accidents.
[1]. Sanborn G E, Magargal L E, Arterial obstructive disease of the eye, Chapter 14, Duane’sClinical Ophthalmology 2005 edition CD-ROM [Google Scholar]
[2]. Beatty S, Au Eong K G, Acute occlusion of the retinal arteries: current concepts and recent advances in diagnosis and managementJ Accid Emerg Med 2000 17:324-29. [Google Scholar]
[3]. Augsburger JJ, Magargal LE, Visual prognosis following treatment of Acute CRAOBr J Ophthalmol 1980 64:913-17. [Google Scholar]
[4]. Rudkin AK, Lee AW, Aldrich E, Miller NR, Chen CS, Clinical characteristics and outcome of standard management of central retinal artery obstructionClin Experiment Ophthalmol 2010 38(5):496-501. [Google Scholar]
[5]. Schmidt DP, Monting JS, Schumacher M, Prognosis of central retinal artery obstruction: Local intraarterial fibrinolysis versus conservative treatmentAJNR 2002 23:1301-07. [Google Scholar]
[6]. Muhammad SAR, Marshall T, Burton BJL, Acute central retinal artery obstruction presenting as CREST syndrome: a case reportCases Journal 2009 2:9 [Google Scholar]
[7]. Sharma S, Brown GC, Central retinal artery obstruction2nd volumeRetinaElsevier publication:1322-34.Chapter 69 [Google Scholar]
[8]. Hayreh SS, Prevalent misconceptions about acute retinal vascular occlusive disordersProg Retin Eye Res 2005 24(4):493-519. [Google Scholar]