Report of an Unusual Case: Testicular Involvement of Chronic Myeloid Leukemia 10 Years after the Complete Response
Cem Nedim Yuceturk1, Berat Cem Ozgur2, Hasmet Sarici3, Pelin Borcek4, Onur Telli5
1Ankara Training and Research Hospital, Urology Clinic, Ankara, Turkey.
2Ankara Training and Research Hospital, Urology Clinic, Ankara, Turkey.
3Ankara Training and Research Hospital, Urology Clinic, Ankara, Turkey.
4Ankara Training and Research Hospital, Pathology Clinic, Ankara, Turkey.
5Ankara Training and Research Hospital, Urology Clinic, Ankara, Turkey.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Onur Telli, Ankara Training and Research Hospital Ulucanlar Cd. No:89 Altındag / Ankara, Turkey.
Phone: +905065987517,
E-mail: onurtelli@yahoo.com
Testicular extra-medullary myeloid cell tumours are rare tumours presenting in most cases with painless testicular swelling. We present here a case of 21-year-old man with painless scrotal swelling. From his medical history, he was treated by allogenic bone-marrow transplantation and chemotherapy 10 years ago because of chronic myeloid leukemia. The pathology of orchiectomy specimen revealed malign cells with blastic cell infiltration means a late relapse of chronic myeloid leukemia. The patient has been in hematological remission and no evidence of any myeloid disorders by 10 years’ follow up. Although testicular involvement is a rare and an unusual event in blast crisis of chronic myeloid leukemia, extramedullary myeloid cell tumour should be considered in the diagnosis of intratesticular tumours.
Testicular leukemia, Extramedullary myeloid cell tumor, Testis
Case Report
An Extra-medullary Myeloid Cell Tumour (EMCT) has been defined as a localized malign tumour of myeloid origin that occurs at an extramedullary location [1]. The presence varies in the literature as granulocytic sarcoma, chloroma, etc. [2]. Although many anatomic locations can be seen most commonly in soft tissues, lymph nodes, bone, skin, gastrointestinal tract and orbit, testicular involvement is rare [3–5]. The incidence of testicular EMCT is pointed out 4-5% in the literature. Clinically, like the other malignant testicular tumours, scrotal mass is usual in testicular EMCT. We are reporting here a case of testicular involvement of chronic myeloid leukemia where the only symptom is a painless scrotal swelling.
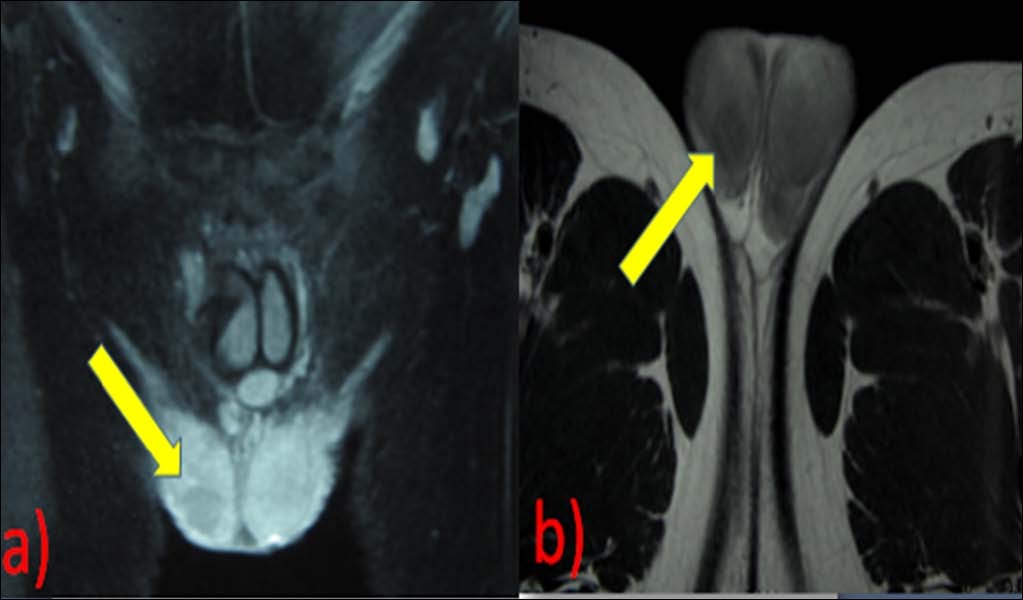
A 21-year-old man presented to our outpatient clinic with right side scrotal swelling of two months’ duration. The patient had no complaints such as urethral discharge, fever, nausea, vomiting or scrotal pain. There was no history of trauma or surgery. A physical examination revealed a painless nodule nearly 2 cm in diameter in the right testis. Urinalysis did not show any abnormality. The complete blood count was in normal levels. Serum levels of α-fetoprotein and β-human chorionic gonadotrophin were within the normal ranges. Scrotal ultrasonography showed a well-defined 1.2 x 1.0 cm hypoechoic solitary mass in the right testis. Magnetic resonance imaging has demonstrated heterogeneous low signal intensity mass on T1 and T2 images, nearly 2.0 cm diameter [Table/Fig-1] in the lower pole of the testis.
Magnetic resonance image of right testis with the lesion (a) T2-enhanced (b) T1-enhanced (The arrow shows lesion of testis)
High inguinal partial orchiectomy was planned for the patient. Peroperative findings were; two nearby lesions in the lower pole of the testis 1.5 x 0.5 cm and 0.5 x 0.5 cm in diameter. Tumour excision and biopsies of the resection bed were performed. When his frozen examination revealed ‘suspicious for hematological malignancy’, it was planned to perform orchiectomy. There were no complications throughout the surgery. We also performed biopsy to the left testis and the pathological examination was normal whereas the right orchiectomy material revealed malign cells with blastic cell infiltration. Detailed history demonstrated that he had forgotten to tell us his treatment because of chronic myeloid leukemia 10 years ago with a complete response by means of allogenic bone-marrow transplantation and chemotherapy. According to these findings, the patient is diagnosed as a late relapse of chronic myeloid leukemia involving the testis. The patient was then referred to medical oncology department for further investigation and treatment. Oncologists detected leukemic retinopathy and orbital infiltration.
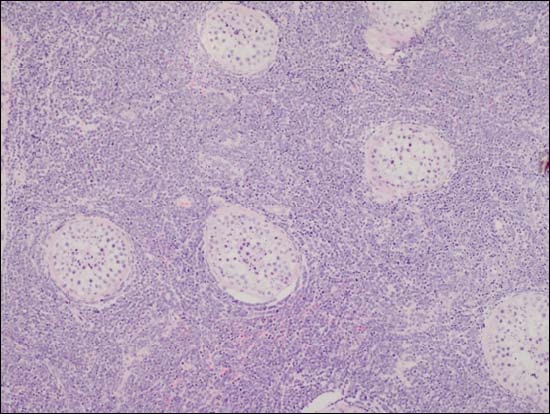
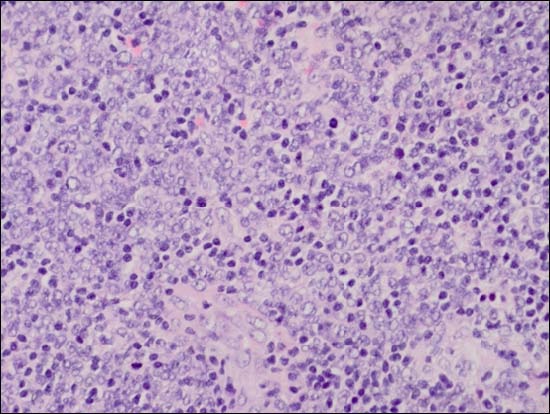
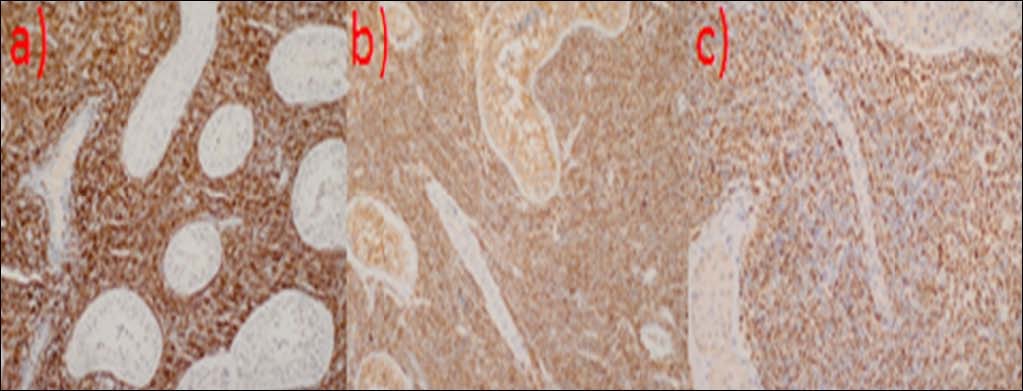
A testicular tissue of 3.5 cm diameter was submitted for intra-operative frozen section with a suspect diagnosis of testicular malignant mass. Serial sections of the material demonstrated a regular, orange coloured testicular tissue with a whitish area of indiscriminate borders. Frozen sections were taken from this focus, which displayed a diffuse, monotonous intertubuler infiltration of tumour cells with large nuclei, open chromatin pattern and brisk mitotic activity. Since the patient’s previous history was not supplied during intraoperative consultation, the frozen diagnosis was ‘suspicious for hematological malignancy. Permanent sections revealed the same histomorphological pattern with a diffuse tumoural infiltration between normal seminiferous tubules [Table/Fig-2]. The nuclei possessed open chromatin with irregular nuclear membranes, small basophilic nucleoli adjacent to nuclear membranes and inconspicious cytoplasm [Table/Fig-3]. Mitotic figures were readily identified. Immunohistochemical studies showed diffuse membraneous positivity with CD 20, CD 10, CD 99 and CD 79a and strong and diffuse nuclear positivity with TdT [Table/Fig-4]. Proliferative activity with MIB-1 was approximately 60%. CD34, MPO, CD30, bcl-6, CD 117, pancytokeratin, desmin and myoglobin were negative. Few mature lymphocytes among tumoural cells were positive for CD3. The final report was ‘Diffuse B lymphoblast infiltration of testicular tissue’. Because the patient had a previous history of bone marrow transplantation for CML, the histopathological appearance was interpreted as an extramedullary blastic crisis with B lymphoblastic origin.
Diffuse tumoral infiltration between seminiferous tubules (hematoxylin-eosin, original magnification X 100)
Tumour is composed of cells with enlarged nuclei, open chromatin, irregular nuclear membranes and small nucleoli. Mitotic figures are readily identified. (hematoxylin-eosin, original magnification X 400)
(a) Diffuse CD 20 positivity (CD 20, original magnification X200) (b) Diffuse CD 99 positivity (CD 99,original magnification X 200) (c) Diffuse TdT positivity (TdT, original magnification X 400)
Discussion
Except the known indications like a tumour in solitary testis and bilateral tumours, partial orchiectomy can also be performed in patients in testicular mass with negative tumour markers that may be possibly benign tumours. In our patient, the lesion was in benign nature according to the radiologic images so that at first we were planning to perform partial orchiectomy. After learning from his medical history that he was treated with allogenic bone-marrow transplantation and chemotherapy because of chronic myeloid leukemia, and when frozen pathology defined a suspect of haematologic malignancy as well as the possibility of testicular involvement in blast crisis of chronic myeloid leukemia, radical inguinal orchiectomy was chosen. Testicular leukemia may be the primary manifestation of leukemia or an established leukemia elsewhere in the body. In our case, the diagnosis was as; blast crisis of extramedullary involvement of chronic myeloid leukemia with multiple testicular masses as main manifestation. The differential diagnosis for infiltrative process involving the testis includes; orchitis, sarcoidosis, lymphoma, benign cysts, tuberculosis and germ/ non-germ cell neoplasia of the testis.
There are some small series of extramedullary blast crisis of chronic myeloid leukemia. In one of the largest series; Cervantes et al., showed, out of more than a hundred cases of blastic crisis of Ph’-positive chronic myeloid leukemia, 13 had extramedullary involvement, lymph nodes were the commonest extramedullary site of blast crisis (8 cases), followed by osteoperiosteal and central nervous system. The median survival of the patients after the onset of extramedullary involvement was shorter than a year [6]. Bane et al. demonstrated renal involvement with uncontrollable unilateral hematuria in chronic myelomonocytic leukemia and was treated with nephrectomy and observed conservatively but seven months later, the patient died because of marrow replacement and occurring sepsis [7]. Literature reviews revealed four reports of testicular involvement in blast crisis of chronic myeloid leukemia [8–10]. Among these four patients there were children and showed the involvement of both testes and central nervous system [11]. Rawal et al. have reported a primer case of testicular extramedullary myeloid cell tumour with an acute testicular hemorrhage which was interpreted as a hematoma into the tumour. After orchiectomy, he has been treated with induction chemotherapy and was followed by radiation therapy to the contralateral testis [12]. Corcoran et al. performed inguinal orchiectomy for an unilateral testicular mass wıth chronic myelomonocytic leukemia [13]. Despite several therapy modalities, overall survival and the prognosis of blastic crisis in chronic myeloid leukemia is poor.
Conclusion
Although it is an extremely rare event, EMCT must be considered in the differential diagnosis of unilateral testicular masses in patients with myelodysplastic disease and also late relapses of the other haematological diseases must be in mind. Blood testis barrier may be a factor of early and late relapses since this barrier decreases the allowing of many chemotherapy regimens [14]. Routine controls must include genital examination and radiologic evaluation if a suspicion occurs.
[1]. Neiman RS, Barcos M, Berard C, Bonner H, Mann R, Rydell RE, Granulocytic sarcoma: a clinico-pathologic study of 61 biopsied casesCancer 1981 48:1426-37. [Google Scholar]
[2]. Kawashima H, Sakamoto W, Nishijima T, Hanada M, Mori K, Maekawa M, Granulocytic sarcoma of the testis preceding acute myeloid leukemiaUrol Int 1988 43:310-2. [Google Scholar]
[3]. Traweek ST, Arber DA, Rappaport H, Brynes RK, Extramedullary myeloid cell tumours: an immunohistochemical and morphologic study of 28 casesAm J Surg Pathol 1993 17:1011-9. [Google Scholar]
[4]. Meis JM, Butler JJ, Osborne BM, Manning JT, Granulocytic sarcoma in non-leukemic patientsCancer 1986 58:2697-709. [Google Scholar]
[5]. Suh YK, Shin HJC, Fine needle aspiration biopsy of granulocytic sarcoma: a clinicopathologic study of 27 casesCancer 2000 90:364-72. [Google Scholar]
[6]. Cervantes F, Rozman M, Nicolás JM, López Guillermo A, Rozman C, Extramedullary blast crisis in chronic myeloid leukemiaSangre (Barc) 1989 Apr 34(2):96-8. [Google Scholar]
[7]. Bane AL, Enright H, Sweeney EC, Chronic myelomonocytic leukemia revealed by uncontrollable haematuriaArch Pathol Lab Med 2001 125:657-9. [Google Scholar]
[8]. Beedassy A, Topolsky D, Styler M, Crilley P, Extramedullary blast crisis in a patient with chronic myeloid leukemia in complete cyto-genetic and molecular remission on interferonalfa therapyLeukemia 2000 24:733-5. [Google Scholar]
[9]. Kusumakumari P, Kumar SR, Pillai GR, Unusual course of chronic myeloid leukemia. A reportAm J Clin Oncol 1994 17:19-21. [Google Scholar]
[10]. Ohyashiki JH, Ohyashiki K, Shimizu H, Miki M, Kimura N, Mori S, Testicular tumour as the first manifestation of B-lymphoid blastic crisis in a case of Ph-positive chronic myelogenous leukemiaAm J Hematol 1988 29:164-7. [Google Scholar]
[11]. Carlson NL, Erichson G, Lissel L, Simultaneous meningeal and testicular lymphoblastic transformation of Philadelphia positive CML in a three year oldAnticancer Res 1990 10:1739-41. [Google Scholar]
[12]. Rawal A, Keeler TC, Milano MA, Testicular extramedullary myeloid cell tumour: report of a case with unique clinicopathologic features and a brief review of the literatureArch Pathol Lab Med 2004 128:332-4. [Google Scholar]
[13]. Corcoran NM, Tsui A, Costello AJ, Bouchier-Hayes D, Unilateral testicular mass in man with chronic myelomonocytic leukemia: unusual presentation of chronic myelomonocytic leukemia sequelaUrology 2005 65(5):1001.e 14-1001.e 16. [Google Scholar]
[14]. Bart J, Groen HJ, van der Graaf WT, Hollema H, Hendrikse NH, Vaalburg W, An oncological view on the blood-testis barrierLancet Oncol 2002 3(6):357-63. [Google Scholar]