Unicystic Ameloblastoma of the Mandible– Report of Two Cases with Review of Literature
Saravanakumar B1, Parthiban J2, Aarthi Nisha V3, Sarumathi T4, Prakash CA5
1 Associate Professor, Department of Oral and Maxillofacial Surgery, Sree Balaji Dental College and Hospital, Bharath University, Chennai, India.
2 Reader, Department of Oral and Maxillofacial Surgery, Tagore Dental College and Hospital, Chennai, India.
3 Senior Lecturer, Department of Oral Medicine and Radiology, Sree Balaji Dental College and Hospital, Bharath University, Chennai, India.
4 Associate Professor, Department of Oral Medicine and Radiology, Sree Balaji Dental College and Hospital, Bharath University, Chennai, India.
5 Reader, Department of Oral and Maxillofacial Surgery, Tagore Dental College and Hospital, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. B. Saravana Kumar, Assosiate Professor, Department of Oral and Maxillofacial Surgery, Sree Balaji Dental College and Hospital, Bharath University, Chennai-600100, India.
Phone: +91 9444385846; +91 9884423453, Email id: drsaranomfs@gmail.com.
Ameloblastoma is classified into solid/multicystic, extraosseous/peripheral, desmoplastic and unicystic types based on the clinical appearance by WHO (2003). Unicystic ameloblastoma is the 2nd and far less frequent growth pattern seen in intra-osseous ameloblastoma. It tends to occur in younger population and constitutes approximately 6% of ameloblastomas with no sexual or racial predilection. Here in, reporting 2 cases of cystic ameloblastoma in the mandible, in varying age groups.
Odontogenic neoplasm, Intra-cystic ameloblastoma, Benign tumor, Cystogenic ameloblastoma, Enucleation Ud
Case 1
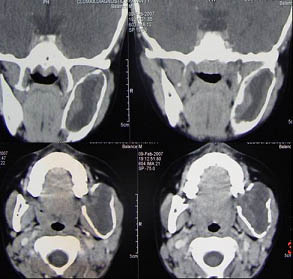
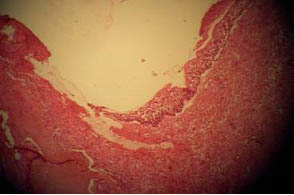
A 16-year-old female patient had a complained of slow growing swelling on the left side of the face since 6 months. There was no history of discharge or pain associated with the swelling. A diffuse extra-oral swelling measuring 2cm x 3cm in diameter was present on the lower left one-third of the face [Table/Fig-1]. On palpation, extraorally, the swelling was afebrile, firm in consistency and non-tender with no effect on surrounding structures. There were no associated intraoral changes on inspection but on percussion and mobility tests, the tooth was mobile with increased pocket depth [Table/Fig-2]. Lymph node examination revealed no changes. A provisional diagnosis of dentigerous cyst was considered. Aspirate revealed a straw colored fluid with few inflammatory and stellate reticulum like cells. Panoramic radiograph revealed a well-defined unilocular radiolucency with sclerotic margins in the body of the mandible approaching the lower border extending from the mesial aspect of 35 to 37 and resorption of mesial and distal roots of 36 [Table/Fig-3]. Coronal and Axial CT revealed an expansile lytic lesion involving the left ramus and coronoid process of the mandible with few incomplete septae within the lesion [Table/Fig-4]. Radiographic differential diagnosis was ameloblastoma, keratocystic odontogenic tumour. Biopsy was performed and histopathological examination revealed ameloblastomatous epithelium lining the cystic cavity and islands of ameloblastic cells extending into the connective tissue wall suggestive of Mural variant of Unicystic ameloblastoma [Table/Fig-5].
Diffuse swelling on the lower left one-third of the face,


Panoramic radiograph revealed a well-defined unilocular radiolucency with sclerotic margins in the body of the mandible approaching the lower border extending from the mesial aspect of 35 to 37 and resorption of mesial and distal roots of 36,

Coronal and Axial CT revealed an expansile lytic lesion involving the left ramus and coronoid process of the mandible with few incomplete septae within the lesion
Histopathological finding -Ameloblastomatous epithelium lining the cystic cavity and islands of ameloblastic cells extending into the connective tissue wall suggestive of Mural variant
Case 2
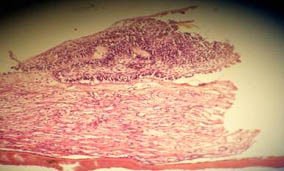
A 55-year-old male patient complained of swelling on the right side of the face since 2 years. There was no history of discharge or pain associated with the swelling. The patient visited the dentist 1 year back for the same complaint when the swelling was initially smaller in size and now he reported to us as the swelling has increased to present size. A diffuse extra-oral swelling measuring 4cm x 5cm in diameter was present on the lower right half of the face [Table/Fig-6] and intraorally there was minimal swelling with obliteration of the buccal vestibule. On palpation the swelling was afebrile, firm in consistency and non-tender. Obliteration of right buccal vestibule was seen extending from 45 to 48 [Table/Fig-7]. Grade 3 mobility irt 45, 46, 47 and 48 was seen. A provisional diagnosis of keratocystic odontogenic tumour was given and differential diagnosis was dentigerous cyst and ameloblastoma was given. Aspirate revealed a straw colored fluid with few inflammatory and stellate reticulum like cells. Panoramic radiograph revealed a well-defined unilocular radiolucency with sclerotic margins in the body of the mandible approaching the lower border extending from distal aspect of 42 to 48 and resorption of roots irt 44 and 45 [Table/Fig-8]. Biopsy was performed and histopathological examination revealed ameloblastomatous epithelium lining the cystic cavity with islands of ameloblastic cells extending into the cystic cavity suggestive of Intra-luminal variant of Unicystic ameloblastoma [Table/Fig-9].
Diffuse swelling on the lower right half of the face.

Obliteration of right buccal vestibule extending from 45 to 48.

Panoramic radiograph revealed a well-defined unilocular radiolucency with sclerotic margins in the body of the mandible approaching lower border from 46 to 48

Histopathological finding - Ameloblastomatous epithelium lining the cystic cavity with islands of ameloblastic cells extending into the cystic cavity suggestive of Intra-luminal variant of Unicysticameloblastoma
The treatment carried out for Case 1 and 2 was Enucleation, decompression and grafting reconstruction with iliac crest bone, under antibiotic coverage with Ofloxacin and Ornidazole, Metronidazole and Tramadol for 1 week and then discontinued after infection control. On follow-up at the intervals of 6 months to 1 year, there was significant regression in the size of the lesion. Both the patients were under observation for 2 years with no significant changes.
Discussion
Ameloblastoma is a benign, locally aggressive and infiltrative odontogenic neoplasm with a rare capacity to metastasize [1]. They comprise only 1.3% of all jaw cysts and tumours [1] and 2nd most common odontogenic neoplasm [2,3] constituting 10 % of neoplasm of odontogenic origin [4].
Cusack in 1827 was the first to provide the accurate description of an ameloblastoma. Falkson gave a detailed description in 1879. Weld was credited for the first histo-pathological description in 1952. Weld called the tumor ‘cystsarcoma’ but suggested that it could have arised from a tooth bud or the dental lamina [5].
In 1998, a critical review of 193 cases of UA verified that most of UA can be associated with impacted tooth i.e. Dentigerous variant (n=90) and not associated with impacted tooth i.e. non-dentigerous variant (n=101) [6].
Leider et al., among the cases found 3 pathological mechanisms for UA – a) reduced enamel epithelium associated with developing tooth, b) cell rests of odontogenic epithelium in the cyst wall, and c) a solid ameloblastoma undergoing cystic changes [7].
Vindhya et al., reported a case of plexiform ameloblastoma and discussed differential diagnosis of unicystic ameloblastoma with odontogenic cysts [8]. In 1998, three histological subtypes of UA were recognized, based on the character and extent of tumor cell proliferation within the cyst wall [7]:
Luminal - cyst wall lined by ameloblastic epithelium (Group I).
Intraluminal - cystic lesion showing proliferation of ameloblastic epithelial lining into cystic lumen (Group II).
Mural - cystic lesion with ameloblastic epithelial invasion into the supporting connective tissue or islands of ameloblastic epithelium in either follicular or plexiform pattern Invasive ameloblastoma arising from lining of the cyst
The predominance of unilocular configuration is exceptionally marked for dentigerous variant ie 4.3:1 compared to non-dentigerous variant 1.1:1. The multilocular lesions demonstrate characteristic ‘honey-comb’ or ‘soap bubble’ appearance. Resorption of roots of adjacent teeth is seen in 40% - 70% of cases [9].
Mahesh G et al., treated a case of plexiform ameloblastoma by resection and free fibula grafting at the defect which yielded good prognosis [10]. In our cases we reconstructed the mandibular defect with iliac crest bone graft which also yielded favourable results.
Sandeep G et al., reported a case report of unicystic ameloblastoma which presented in a multilocular pattern which needed aggressive management [11]. In our case reports both the cases were unilocular variant.
Vinod T performed hemimandibulectomy with disarticulation with radiological margin clearance and Titanium plate reconstruction of condyle via extended submandibular approach [12]. Rakesh S et al., performed segmental mandibulectomy via lip split incision to achieve primary closure [13].
UA has a good prognosis and the probable reason is that the UA is generally cystic, well-localized and surrounded by a fibrous capsule. However, once the tumor has breached the periphery of the capsule, it can infiltrate the surrounding cancellous bone and therefore behave more aggressively [7]. The recurrence rate following enucleation and curettage is 10-33% and is more likely in the mural variant. Recurrence of UA may be long delayed, and a long-term postoperative follow-up is essential in the proper management of these patients [7].
Di Cosola et al., suggested that a conservative approach is advisable in the case of a noninvasive and non proliferating cyst wall. The location of the lesion seems to be an important risk factor for the recurrence of the ameloblastoma. The authors concluded that, for the diagnostic phase the instrumental examinations (X-RAY, CT or MRT) are essential; while intralesional biopsies are inefficient because they don’t offer a whole vision of the tumor and could lead to diagnostic error. Therefore we think that it is advisable, considering: the site and extension, of the lesion, age and general conditions of the patient, to remove the lesion in a conservative manner in a first surgical step and according to the histological aspect evaluate a possible radical resection [13].
Conclusion
Unicystic ameloblastoma tends to affect young adolescent patients. UA can only be diagnosed based on histopathological features and cannot be predicted on clinical and radiological grounds alone. The examination of the entire lesion through sectioning at varying levels is mandatory for securing the final diagnosis. UA is believed to be less aggressive and should be treated conservatively.
[1]. Arotiba GT, Ameloblastoma in Nigerian children and adolescents: A review of 79 casesJ of Oral and Maxillofacial Surg 2005 63:747-51. [Google Scholar]
[2]. Kessler HP, Intraosseous ameloblastomaOral and Maxillofacial Surg Clin N Am 2004 16:309-22. [Google Scholar]
[3]. Neville BW, Damm DD, Allen CM, Bonquot JE, Odontogenic Cysts and TumoursOral and Maxillofacial Pathology 2004 2nd edSaunders:611-9. [Google Scholar]
[4]. Rapids AD, Ameloblastomas of Jaw: Clinico-pathological review of 11 patientsEJSO 2004 30:998-1002. [Google Scholar]
[5]. Ameloblastoma Luca’s Pathology of Tumors of the Oral Tissues 1999 5th edChurchill Livingstone:25-44. [Google Scholar]
[6]. Philpsen HP, Reichart PA, Unicystic ameloblastoma - A review of 193 cases from the literatureOral Oncol 1998 34:317-25. [Google Scholar]
[7]. Leider AS, Eversole LA, Barker MF, Cystic AmeloblastomaOral Surg Oral Med Oral Pathol 1985 60:624-30. [Google Scholar]
[8]. Vindhya S, Mahija J, Rakesh S, Unicystic ameloblastoma as a differential diagnosis for odontogenic cystsOral and Maxillofacial Pathology Journal 2014 5(1):466-9. [Google Scholar]
[9]. Robinson L, Martinez H G, Unicystic ameloblastoma- A prognostically distinct entityCancer 1977 40:2278-85. [Google Scholar]
[10]. Mahesh G, Meena K, Aarti M, Unicystic Ameloblastoma of Mandible: A Case ReportIndian J Stomatol 2011 2(4):273-6. [Google Scholar]
[11]. Sandeep SG, Shubanga M, Gupta MK, Raju R, Kavitha PK, Unicystic Ameloblastoma presenting as a multilocular lesion: A Case reportPeoples’s J of Scientific Research 2011 4(2):55-7. [Google Scholar]
[12]. Vinod T, Unicystic Ameloblastoma of Mandible- A Case reportJIADS 2011 2(2):71-3. [Google Scholar]
[13]. Di Cosola M, Turco M, Bizzoca G, Tavoulari K, Capodiferro S, Escudero-Castaño N, Ameloblastoma of the jaw and maxillary bone: clinical study and report of our experienceAVANCES EN ODONTOESTOMATOLOGÎA 2007 23(6):367-73. [Google Scholar]