CBCT Cyst Leasions Diagnosis Imaging Mandible Maxilla
K Prabhusankar1, A Yuvaraj2, C.A Prakash3, J Parthiban4, B Praveen5
1 Professor, Department of Oral and Maxillofacial Surgery, Rama Dental College and Hospital, Kanpur, India.
2 Reader, Department of Oral and Maxillofacial Surgery, Sri Venkateswara Dental College and Hospital, Chennai, India.
3 Reader, Department of Oral and Maxillofacial Surgery, Tagore Dental College and Hospital, Chennai, India.
4 Reader, Department of Oral and Maxillofacial Surgery, Tagore Dental College and Hospital, Chennai, India.
5 Professor, Department of Oral and Maxillofacial Surgery, Tagore Dental College and Hospital, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. K. Prabhusankar, 12/23,G-2, Sambangi Street, West Mambalam, Chennai-600033, India.
Phone: 09840100853,
E-mail: prabhu_omfs@yahoo.com
The bony anatomy and the soft tissue contours of the maxillofacial region, along with the oro dental tissues, is very complex. In earlier times, analog radiographs of the skull, the mandible and the sinuses, along with intraoral films, were the only tools which were available for dentists. The past decade has seen a revolution in dental imaging, with the introduction of Cone beam computed tomography/cone beam volumetric tomography (CBCT/CBVT). In this article, we have discussed the value of CBCT in diagnosis and treatment planning which we observed in four cases of maxillofacial cystic lesions. It proved to be a multifaceted win-win situation for the diagnostician, the patient and the operating surgeon. The 3D imaging led to a precise pre-operative surgical planning, resulting in a surgery that was minimally invasive, minimally morbid and time saving and at the same time, conservative, yet complete.
Advanced diagnostic radiology, Cystic, Conservative treatment
Case Studies
The current article brings out the benefits and indications of/for 3D imaging in reducing the morbidity of surgical treatment procedures which are done on patients. In this case study, we selected four cases of cystic lesions of the jaws, evaluated their preoperative anatomies and treated the patients in the best conservative manner which was possible, with minimal morbidity.
The potential risks and preservation of natural structures to the best extent which was possible, have been highlighted.
Case 1
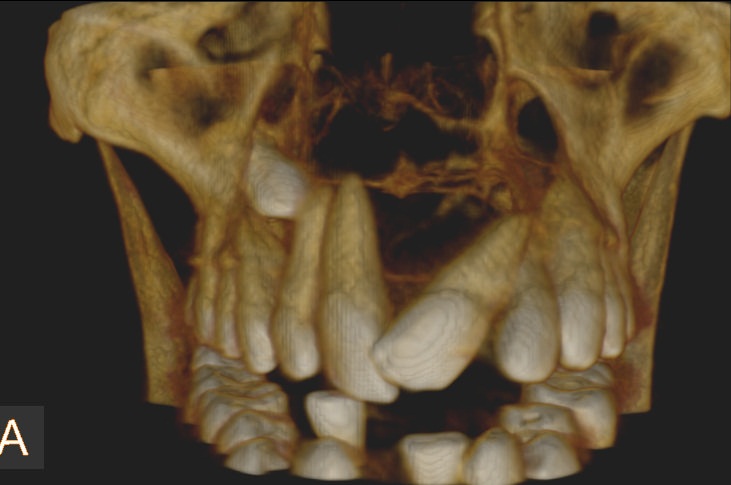
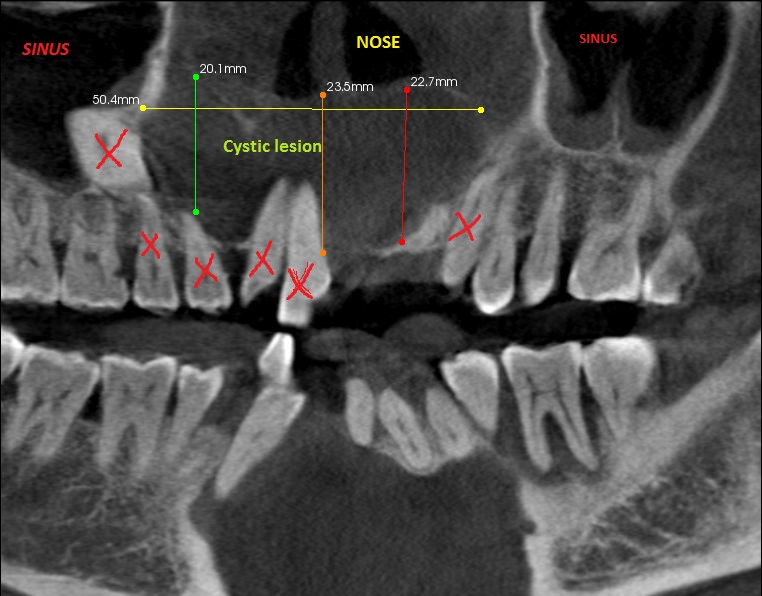
A 50-year-old male patient reported with the complaint of a swelling in the upper anterior region, which had been present since the past two months. An OPG done, revealed a large radiolucent lesion which extended from 16 to 24, with few missing teeth and an impacted tooth in right maxillary sinus area. Surgery was done under General anaesthesia (GA). Pre-operative planning done by Cone beam computed tomography (CBCT) helped in saving adjacent teeth [Table/Fig-1,2] and also in removing the cyst from the nasal floor area, along with the impacted canine tooth, with minimal morbidity.
3DCBCT showing extension of the lesion
3DCBCT guided treatment plan
Case 2
A 21-year-old female patient came with a history of pain and swelling in the lower anterior region, which was of three years duration. Forty four and 45 had been extracted a year ago. Swelling recurred and there was a draining intraoral sinus in 43 region. An Ortho pantomo graph (OPG) done, revealed a large radiolucent lesion which extended from 43 to 33 region [Table/Fig-3]. A biopsy was done and its histopathology report was suggestive of Odontogenic Keratocyst (OKC). A CBCT was done [Table/Fig-4]. All the lower anterior teeth were RC treated. The lesion was enucleated in toto and the residual cavity was treated with Carnoy’s solution. The RC treated teeth were later crowned. A 2 year follow-up of the patient revealed good bone healing, with no recurrence of the lesion.
OPG showing a bony defect in symphisis region

3DCBCT showing a bony defect in symphisis region
Case 3
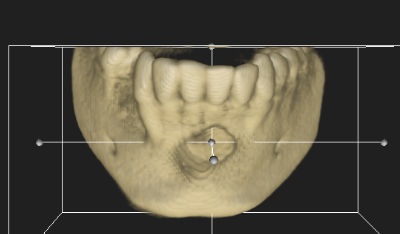
A 21-year-old male came with a history of swelling and inability in opening mouth since 15 days. An OPG was done later and it revealed a radiolucent lesion around an impacted 38 [Table/Fig-5]. A biopsy was done and it was suggestive of a dentigerous cyst. CBCT was done to identify the relationship of inferior alveolar nerve (IAN) and root apex of 37 with the tooth and the cystic lesion[Table/Fig-6]. RCT was done in 37 and lesion was enucleated, with no damage to the IAN.
OPG showing a cyst like lesion in relation to 38

CBCT showing a cyst like lesion in relation to 38
Case 4
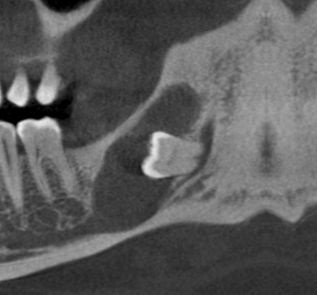
A 55-year-old female came with a chief complaint of pain in 2nd quadrant, of 15 days duration, with mild difficulty in opening of mouth. An OPG was done and it revealed a supra erupted, buccoverted 28 and impacted 38 and 48 [Table/Fig-7]. Twenty eight was extracted under Local anaesthesia (LA). Swelling and pain showed initial improvement, but after a few days, symptoms recurred. The CBCT revealed a large radiolucent lesion in the posterior maxilla, which obliterated the the entire left maxillary antrum [Table/Fig-8]. The posterior wall of the maxilla was also destroyed and the lesion extended into the pterygoid region. An incisional biopsy was done under LA and tumour was reported as an osteogenic sarcoma. The patient was referred to an oncologist for appropriate management.
OPG shows a bony defect in relation to 28

3DCBCT shows a bony defect in relation to 26,27

Discussion
Technical advances and the digital revolution in dentistry is creating new opportunities for diagnosis, treatment planning and computer aided manufacturing in almost every specialty of the profession.
CBCT scanners have recently been developed for dentomaxillofacial imaging. They were developed by eldkamp et al., [1]. Dedicated CBCT scanners for use in oral and maxillofacial (OMF) regions were pioneered in the late 1990s independently by ari et al., [2]. In Japan and Mozzo et al., in Italy [3].
In 2008, the Executive Council (EC) of the AAOMR published an executive opinion statement on the performance and interpretation of CBCT in dentistry [4].
Modern advances made in imaging help dentists in using CBCT with the appropriate field of view and spatial resolution; therefore, the internal mineralized structures of the pathologic lesions can be investigated by using a low radiation dose [5].
The main advantages of CBCT imaging are, that it offers a real-size dataset with multiplanar cross-sectional and 3D reconstructions which are based on a single scan, on using a low radiation dose [3].
Because a volume of data has been acquired and stored by CBCT, these data can be reformatted or realigned and several different types of images can be synthesized in any way which diagnostician requires [6].
CBCT examination has been found to be useful in the preoperative diagnosis of impacted lower third molars [7].
In evaluating cysts or benign tumours, a single, intraoral radiograph may not fully record the supero-inferior and mesiodistal dimensions of the lesion. Multiplanar sections (axial, coronal, and sagittal planes) are required when cysts or tumours which are located deep in the tissues are examined. CBCT is a better option for making a diagnosis [5]. Apart from pre surgical evaluation of aggressive benign cysts or tumours, CBCT is also helpful in post surgical follow-ups of lesions that may have high recurrences. Because of super imposition of large tissue volume, an extraoral plain film radiograph often cannot provide reliable information on the internal structure of a lesion. Some other benefits of CBCT are accuracy in measurement and absence of image distortions [6].
CBCT is a better imaging modality which can be used for the assessment of foreign bodies and fragments which are present in the face, such a fragments which are embedded from gunshot wounds, automobile or industrial accidents, and for localizing broken dental needles.
As the technology now stands, with respect to evaluating maxillofacial disease, CBCT is mostly used as a tool for diagnosing diseases of the osseous structures. The main challenge in CBCT imaging and diagnosis is the lack of familiarity which is experienced by most of the dental professionals, with the concept of multiplanar imaging that is offered by this new and exciting technology [6]. Comfort level amongst dental surgeons is high with conventional 2D IOPA and panoramic views. Multiplane imaging ( MPI) interpretation and understanding is still lacking and it needs to be addressed at the earliest.
In view of the increasing number of available CBCT scanners, providing an accuracy which is superior to that which is provided by conventional cephalograms [8], and the amount of described indications, the importance of the cone-beam technology will further increase in the near future.
Conclusion
It is strongly recommended that to take advantage of the CBCT images in full, the diagnostician should be able to understand and apply the concept of multiplanar reformatting to the highest degree. It is the dentist who has to reveal the information which is related to each diagnostic task which is backed by a sound knowledge of anatomy and our skills, to retrieve relevant diagnostic information.
[1]. Feldkamp LA, Davis LC, Kress JW, Practical cone-beam algorithmJ Opt Soc Am 1984 1(6):612-9. [Google Scholar]
[2]. Aria Y, Tammisalo E, Iwai K, Hashimoto K, Shinoda K, Development of a compact computed tomographic apparatus for dental useDentomaxillofac Radiol 1999 28:245-8. [Google Scholar]
[3]. Mozzo P, Procaccic Tacconi Martini PT, Andreis IA, A new volumetric CT machine for dental imaging based on the cone-beam technique : preliminary resultsEur Radiol 1998 8:1558-64. [Google Scholar]
[4]. Carter L, Farman AG, Geist J, Scarfe WC, Angelopoulos C, Nair MK, American Academy of Oral and Maxillofacial Radiology executive opinion statement on performing and interpreting diagnostic cone beam computed tomographyOral Surg OraL Med Oral Pathol Oral Radiol Endod 2008 106:561-2. [Google Scholar]
[5]. Macdonald-Jankowski DS, Focal cemento-osseous dysplasia: a systematic reviewDentomaxillofac Radiol 2008 37:350-60. [Google Scholar]
[6]. Ghaeminia H, Meijer GJ, Soehardi A, Borstlap WA, Position of the impacted third molar in relation to the mandibular canal. Diagnostic accuracy of cone beam computed tomography compared with panoramic radiographyInt. J. Oral Maxillofac Surg 2009 38:964-71. [Google Scholar]
[7]. James JC, Brain LS, The use of cone beam computed tomography as an aid in evaluating and treatment planning for mandibular cancerJ Oral Maxillofac Surg 2007 65:766-71. [Google Scholar]
[8]. Hilgers ML, Scarfe WC, Scheetz JP, Farman AG, Accuracy linear Temporomandibular joint measurements with cone beam computed tomography and digital cephalometric radiographyAm J Orthod Dentofac Orthop 2005 128:803-911. [Google Scholar]