Primary postpartum haemorrhage (PPH) is defined as bleeding from the genital tract of 500 mL or more in the first 24 hours following delivery of the baby [1]. It is one of the leading causes of maternal mortality in developing countries [2]. Several risk factors have been identified over the years as causative of its occurrence. Recent estimates have indicated that at least one quarter of all maternal deaths are caused by haemorrhage i.e. at least 18,000 annually, worldwide [3]. Most of these deaths occur within four hours of delivery and are a result of problems which occur during the third stage of labour [4].
Several risk factors have been identified as causative of postpartum haemorrhage, for example; Asian race, anaemia, hypertensive disorders, prior PPH, history of retained placenta, multiple pregnancies, antepartum haemorrhage, macrosomia (>4 kg), chorioamnionitis, uterine over distension, epidural anaesthesia, prolonged first/second stage of labour, induction labour, etc [5]. Several studies have demonstrated that induction or augmentation of labour with oxytocin increases the risk of postpartum bleeding [6,7]. However, modern practice of labour induction with prostaglandin analogues have claimed no difference [8] in bleeding after deliveries as compared to that which occurs after spontaneous vaginal deliveries, but this evidence is somewhat limited.
Early identification of third stage blood loss is very vital in order to institute prompt treatment, so that morbidity and mortality which are associated with PPH is reduced. But universally, practitioners resort to visual estimation of blood loss at delivery, which is observer based and is prone to errors. Most of the times, blood loss is underestimated and this delays the intervention. In this regard, a specially designed bag estimation of blood loss is more accurate than a visual estimation and it may have particular utility in the developing world [9].
This study is based on a quantitative assessment of blood loss which occurs in induced and vaginal deliveries, which determines as to which of the population is at a greater risk for postpartum haemorrhage.
Materials and Methods
This non-interventional, prospective and clinical observation based study was conducted at the Department of Obstetrics and Gynecology, Kasturba Medical College, Manipal, a tertiary care centre in southern India. Approval was obtained from hospital’s Research Ethics Board for conducting the study. The study population consisted of 200 pregnant ladies, 150 of whom had vaginal deliveries after labour induction and 50 of whom had spontaneous vaginal deliveries, who served as controls. The patients with a history of bleeding disorders or those who were on heparin therapy were excluded from the study.
A detailed history was taken from each woman and general physical examinations were done. Risk factors such as preeclampsia, gestational hypertension, gestational diabetes mellitus and a previous history of postpartum haemorrhage were duly noted. Written informed consents were taken from the patients prior to the induction. The type of induction was determined by the obstetrician who was in charge of the patient. The study included the following induction protocols.
a) Artificial Rupture of Membranes (ARM) which was supplemented with oxytocin.
b) Preinduction priming with Mifepristone, followed by intracervical dinoprostone gel (Cerviprime).
c) Intracervical Cerviprime only.
d) Oral dinoprostone tablets (Primiprost).
The blood lost during the third stage of labour was recorded by means of a specially designed blood collection bag. Haemoglobin values were recorded for each patient at the start of labour and on first postnatal day. In addition, the maternal age, parity index, gestational age, duration of labour, mode of induction, indication for induction were recorded. All patients, whether they were induced or not, received inj Methergine 0.2 mg IM after placental expulsion and those who had hypertension were given inj. Prostodin 250 micrograms IM. The weight of the baby, complications which were associated and the APGAR values at 5 and 10 minutes were also duly recorded.
Description of blood collection bag
It consisted of a funneled and calibrated collecting pouch which was attached to a plastic sheet that was placed under the woman’s buttock immediately after delivery of placenta. Two belts attached to the upper end of the drape were tied around the woman’s abdomen to optimize blood collection and calibration levels, which indicated the volume of blood which was collected by the drape. The calibration provided an objective measurement of postpartum blood loss.
Statistical Analysis
Statistical analysis was performed by using SPSS statistical package (version 14 for windows). Cases and controls were compared by means of Chi-square (χ2) test for cross tab data, independent t-tests for comparison of blood loss between induced and spontaneous delivery groups, ANOVA for variations within induced groups, paired t-test for paired observations (haemoglobin changes before and after delivery). The difference was considered to be statistically significant at a p-value of 0.05.
Results
A total of 200 patients were studied in one year’s time period, 150 of them had vaginal deliveries following labour induction and remaining 50 had delivered spontaneously. The two groups were well-matched for age, height, weight before delivery and parity index [Table/Fig-1]. The incidence of preeclampsia was statistically more significant in induced group, may be because of the policy of routine induction of labour in them by 38 weeks of gestation. Similarly, incidence of prelabour rupture of membranes was more in induced group, as the condition required delivery if patient did not go into spontaneous labour. Gestational age at delivery was significantly lower in induced group, as many of the conditions in that group required delivery by 37 completed weeks. The duration of labour was also significantly higher in induced group (6 hrs 56 min vs. 5 hrs 28 min). There were no significant differences between haemoglobin values and birth weights in two groups. [Table/Fig-2] shows the methods and drugs used in induction of labour. We used surgical induction ie, artificial rupture of membranes (ARM) whenever cervix was favourable and 3 cm dilated followed by continuous oxytocin infusion as per standard guidelines in 31patients. When the Bishop score was poor, intracervical dinoprostone E2 gel in order to ripen the cervix in 59 cases and in some, it was repeated every eighth hour till satisfactory response was obtained. Forty subjects had preinduction cervical preparation by oral mifepristone 200 mg and followed by intracervicalcerviprime 24 hours later. Oral primiprost (PGE2 – dinoprostone) was used whenever there was frank leak, as intracervical cerviprime was likely to be expelled by liquor gushing out of vagina. [Table/Fig-3] shows analysis of third stage blood loss (means and standard deviations) in two main groups and subgroups of induced groups.The mean blood loss in induced group was approximately 30 mL more than spontaneous group. This difference however was not statistically significant (independent t-test statistics revealed p value of 0.12). Among the induced group, artificial rupture of the membranes (ARM) followed by oxytocin had more blood loss compared to other methods of induction. To determine variance within induction group, ANOVA (one way analysis of variance) was conducted. The test [Table/Fig-4] showed significant variations in blood loss between and within different induction groups (f-value: 20.8, p-value <0.001).
Demographic characteristics of study and control groups a independent t- tests, b chi sq tests
| Variables | Induced (n = 150) | Spontaneous (n = 50) | p-value |
|---|
| Maternal Age (Yrs) | 26.4 ± 3.87 | 27.2 ± 3.80 | 0.22 a |
| Height (mtr) | 1.543 ± 0.04 | 1.548 ± 0.05 | 0.54 a |
| Weight before delivery(Kg) | 62.23 ± 8.06 | 64.29 ± 10.04 | 0.61 a |
| BMI | 27.4 ± 3.24 | 26.8 ± 4.15 | 0.45 a |
| Parity |
| -Nullipara | 89 (59%) | 25(50%) | |
| -Primipara | 52 (35%) | 23 (46%) | |
| -Multipara | 9 (6%) | 2 (4%) | 0.34 b |
| Antenatal Complications |
| -Preeclampsia | 36 (24%) | 3 (6%) | 0.001 b |
| -Gestational Hypertension | 12 (8%) | 1 (2%) | 0.13 b |
| Essential hypertension | 9 (6%) | Nil | 0.07 b |
| Gestational Diabetes | 24 (16%) | 4 (8%) | 0.15 b |
| -IUGR | 18 (12%) | 2 (4%) | 0.10 b |
| -Oligoamnios | 15 (10%) | 2 (4%) | 0.18 b |
| -PROM | 27 (18%) | 3 (6%) | 0.03 b |
| -Past Dates | 9 (6%) | Nil | 0.07 b |
| Gestational age at labour (Wks) | 37.1 ± 1.75 | 38.2 ± 1.91 | <0.01 a |
| Duration of labour (hrs) | 6 hr 56 min ± 2 hr 34 min | 5 hr 28 min ± 2 hr 24 min | 0.002 a |
| Hb before delivery (gm/dL) | 12.01 ± 0.86 | 12.19 ± 1.27 | 0.39 a |
| Birth Weight (Kg) | 2.853 ± 0.386 | 2.901 ± 0.430 | 0.55 a |
| Artificial Rupture of membranes (ARM) followed by Oxytocin intravenous infusion | 31 |
| Intracervicaldinoprostone E2 gel (Cerviprime) | 59 |
| Oral Mifepristone followed by intracervicaldinoprostone gel | 40 |
| Oral dinoprostone (PGE2) tablets (Primiprost) | 20 |
| Total | 150 |
Third stage blood loss in various groups in mL
| Numbers | Mean | Std. Dev |
|---|
| According to the type of delivery |
| Induced delivery | 202 | 117 |
| Spontaneous delivery | 172 | 114 |
| According to the method of induction |
| ARM & oxytocin | 327 | 140 |
| Cerviprime | 173 | 99 |
| Mifeprostone&Cerviprime | 165 | 64 |
| Primiprost | 166 | 70 |
One Way Analysis of Variance (ANOVA) of blood loss variation
| Sum of Squares | Df | Mean Square | f | Sig. |
|---|
| Between Groups | 611930.175 | 3 | 203976.725 | 20.829 | .0001 |
| Within Groups | 1429740.659 | 146 | 9792.744 | | |
| Total | 2041670.833 | 149 | | | |
A pair wise comparison of different induction protocols was done by using Tukey’s post hoc tests. It was found that ARM and oxytocin group showed significant increases in blood loss as compared to those in other groups. Blood loss was comparable and lesser in different kinds of prostaglandins and it did not show statistically significant variations. The statistical results have been shown in [Table/Fig-5].
ANOVA Post-hoc Statistics (Tukey’s test)
| Induction protocols | n | Different (p<0.05) from |
|---|
| ARM & oxytocin | 31 | Cerviprime, Mifeprostone with Cerviprime, Primiprost |
| Cerviprime | 59 | ARM & Oxytocin |
| Mifeprostone & Cerviprime | 40 | ARM & Oxytocin |
| Primiprost | 20 | ARM & Oxytocin |
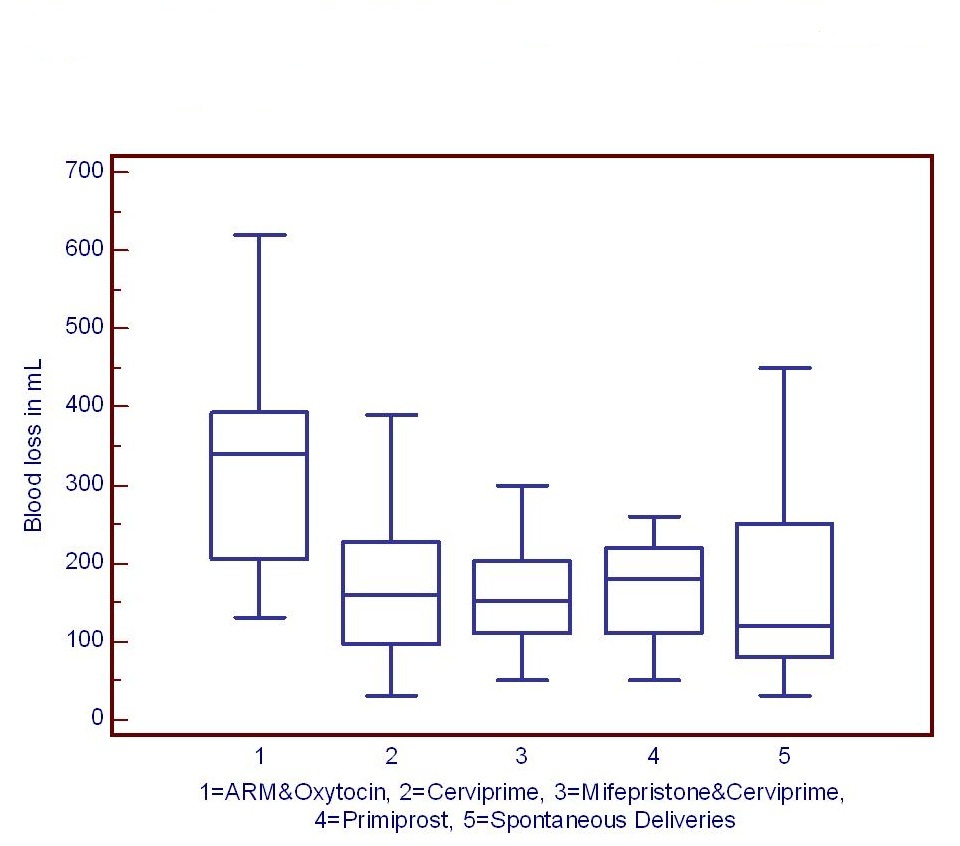
Further analysis was done to compare the blood loss in various induction protocol groups with that in spontaneous delivery group, to determine as to which method of induction was associated with higher blood loss as compared to spontaneous births. The results of independent t-tests have been shown in [Table/Fig-6]. Oxytocin group also had comparatively more blood loss than spontaneous group. Labour induction using prostaglandins did not show more blood loss as compared to that in those who delivered spontaneously. The blood losses in different groups have been pictorially represented in box and whisker plots [Table/Fig-7].
Third stage blood loss in various induction protocols compared to spontaneous deliveries
| Type of induction (n) | Control (n) | p-Value |
|---|
| ARM & oxytocin (31) | Spontaneous (50) | < 0.0001 |
| Cerviprime (59) | Spontaneous (50) | 0.94 |
| Mifeprostone&Cerviprime (40) | Spontaneous (50) | 0.74 |
| Primiprost (20) | Spontaneous (50) | 0.83 |
Box and whisker plot showing blood loss in different Group
[Table/Fig-8] shows changes in haemoglobin values before labour and immediate postpartum day. Both induced and spontaneous delivery groups had statistically significant drop in haemoglobin values, but the drop was relatively more in induced group compared to spontaneous vaginal delivery (0.96 gm/dL vs. 0.56 gm/dL) which appeared statistically significant (p=0.001). There were five cases postpartum haemorrhage (as defined as blood loss > 500 mL) in induced group. Four occurred in oxytocin group and one occurred in cerviprime induced delivery group and all the five cases responded to conservative treatment and none of them required any surgical intervention. There were no such cases in spontaneous vaginal delivery group.
Changes in the haemoglobin after delivery
| Haemoglobin before delivery | Haem- oglobin after delivery | Significance |
|---|
| Mean | St Dev | Mean | St Dev | p-Value* |
|---|
| Induced Delivery (n=150) | 12.01 | 0.86 | 11.05 | 1.19 | 0.001 |
| Spontaneous Delivery (n=50) | 12.19 | 1.27 | 11.63 | 1.21 | 0.001 |
Discussion
WHO statistics showed that haemorrhage and hypertensive disorders were one of the leading causes of maternal mortality in developing countries, with haemorrhage accounting for more than 30% of the deaths which were reported. With the increasing number of deliveries which were performed following labour inductions, a detailed study on the supposedly increased risk of postpartum haemorrhage which was associated with induced labour has become a necessity. Studies have shown that the number of inductions which were performed had nearly doubled in the period from 1989-1997. According to current studies, 9.5 to 33.7% of all pregnancies annually undergo labour induction. It is generally believed that third stage blood loss is more in patients whose labour is induced with oxytocin induction or augmentation than in patients who deliver without induction. This is because, uterus which contracts under the influence of oxytocin hormone during first stage of labour, fails sometimes to continue to do so after delivery of baby and expulsion of placenta. Another reason which is often quoted is increased incidence of precipitate labour in these women because of injudicious use of oxytocin (however it was not seen in this study, as we were very cautious with oxytocin). However, prostaglandins outscore oxytocin induction, because they are able to induce structural changes in the poorly ripe cervix, making it favourable for easy dilatation during first stage of labour and hence, they are used more commonly these days [10]. Another advantage is that there are available as many analogues and can be used by different routes [11]. In many studies, labour induction with prostaglandins was associated with decreased third stage blood loss [12].
Though there are ample numbers of studies on the incidence of primary postpartum haemorrhage in various types of labour inductions, the information in literature on exact amount of blood loss which occurs during third stage of labour is limited. A previous study done in the United States showed greater blood losses in oxytocin administered group (333 ± 298 mL) as compared to those in controlled group (345 ± 285 mL) [13]. Brinsden and Clark from St Mary’s Hospital, Portsmouth, Hampshire, reported a mean blood loss of 235 mL in induced group and of 205 mL in spontaneous vaginal deliveries [14]. In our study, the blood loss in oxytocin group was comparable (334 ± 147 mL), but control group had less blood loss (172 ± 114 mL). This may be attributed to current practice of active management of third stage labour to control the amount of blood loss.
A study which was carried out in Jamaica focused on blood loss occurred in misoprostol induction [15]. There was a significantly greater mean blood loss at delivery in all induced labour cases as compared to that in those who were not induced. For misoprostol (162.5 ± 190 mL), oxytocin (150 ± 100 mL and for oxytocin plus misoprostol (150 ± 150 mL), while controls had the lowest mean blood loss (100 ± 130 mL) occurring where no predelivery oxytocin was needed. Because of other adverse effects which are associated with misoprostol induction, we do not favour its usage in third trimester labour induction.
Many studies done on usage of dinoprostone (PGE2) for labour induction by various routes have focused mainly on incidence of postpartum haemorrhage, as was defined by a blood loss more than 500 mL, but not on the amount of third stage blood loss. Howarth GR and Botha DJ, in their Cochrane meta analysis review, stated that prostaglandin induction was not associated with an increased risk of postpartum haemorrhage as compared to that in controls [16]. Present study also revealed that prostaglandin induction (either through oral or vaginal route) was not associated with increased blood loss as compared to that in those who delivered spontaneously. Present study did not show significant drops in haemoglobin values in induced and spontaneous delivery groups following deliveries (12.01±0.86 gm/dL to 11.05±1.19 gm/dL, 12.19± 1.27 to 11.63±1.21 gm/dL). This may be due to the fact that present study did not show significant difference in quantity of blood loss in third stage in either of the groups. Bhullar A et al., studied haemoglobin changes in normal population as compared to those in buccal misoprostol group and reported that a major haemoglobin drop did not occur following delivery unless it was preceded by postpartum haemorrhage [17]. Many studies done on estimation of third stage blood loss were based on visual estimation of blood loss that occurred at the time of placental delivery and were sometimes underestimated by 25 to 50% [18]. Razvi K et al., conducted a prospective study at National University Hospital, Singapore. They compared visual Estimation of Blood Loss (EBL) at delivery with laboratory determination of Measured Blood Loss (MBL). There was a tendency to underestimate blood loss when MBL was between 301 to 500 mL [19].
Another randomized controlled study done by Patel et al., which involved 123 women who delivered at District Hospital, Belgaum, Karnataka, India, indicated that the visual estimate of blood loss was 33% less than drape estimate. It was opined that drape estimation of blood loss was more accurate than visual estimation and that it may have particular utility in developing world [9]. In our study, we used a blood collection bag with a calibrated collection pouch which was designed similar to BRASS-V drape which was used in Belgaum study [9]. We found this technique to be very useful in our study, for accurate assessment of blood loss. The potential benefit of this type of estimation of blood loss lies in the identification of acute postpartum haemorrhage that occurs in conditions like anaemia, preeclampsia and institution of timely and appropriate intervention measures [20].
Conclusion
Modern methods of labour induction which use prostaglandins have made the parturition process relatively safer, but there are occasions where oxytocin has to be used, especially when labour augmentation is required. However, postpartum haemorrhages can occur in any type of delivery, induced or vaginal, oxytocin or prostaglandin induced, and it is very vital to diagnose them early, in order to decrease maternal mortality and morbidity which are associated with it. Accurate estimation of blood loss is very important in this aspect and a visual estimation is reported to underestimate the quantum of blood loss and it is also observer dependent.The blood collection technique which has been mentioned in the present study is accurate, easy to use and relatively in expensive (<Rs. 100 per sterilized bag). It also allows earlier detection of postpartum haemorrhage, especially in cases like anaemia, preeclampsia, where even smaller quantity of blood loss is associated with catastrophic outcomes.