Subcutaneous Dermatofibroma: A Rare Case Report with Review of Literature
Harjot Kaur1, Jasleen Kaur2, Karamjit Singh Gill3, Rahul Mannan4, Swati Arora5
1 Asscoiate Professor, Department of Pathology, Sri Guru Ram Das Institute of Medical Sciences and Research, Amritsar, Punjab, India.
2 Professor, Department of Dermatology, Sri Guru Ram Das Institute of Medical Sciences and Research, Amritsar, Punjab, India.
3 Professor, Department of Pathology, Sri Guru Ram Das Institute of Medical Sciences and Research, Amritsar, Punjab, India.
4 Associate Professor, Department of Pathology, Sri Guru Ram Das Institute of Medical Sciences and Research, Amritsar, Punjab, India.
5 Assistant Professor, Department of Dermatology, Sri Guru Ram Das Institute of Medical Sciences and Research, Amritsar, Punjab, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Harjot Kaur, Asscoiate Professor, Department of Pathology, Sri Guru Ram Das Institute of Medical Sciences and Research, Vallah, Amritsar-143001, Punjab, India.
Phone: 09781516166,
E-mail: harjotbhandari@gmail.com
A purely Sub-cutaneous benign fibrous histiocytoma (BFH; dermatofibroma) is rarely reported, as it is usually a dermally located mesenchymal tumour and in absence of supportive immunohistochemical (IHC) studies, it is often misdiagnosed. We are describing a case of a 19-year-old female who presented to the skin outpatient department with a painful swelling on the medial side of her thigh. Fine needle aspiration (FNA) revealed a sub-cutaneous spindle cell (mesenchymal) lesion which was corroborated on histopathology, with differentials of BFH and dermatofibrosarcoma protruberans (DFSP). BFH constitutes a diagnostic dilemma for both clinicians and pathologists, because the lesions share common clinical symptoms, radiological characteristics and histological features with many varied entities. For its subtyping and confirmation; immunohistochemical (IHC) studies were undertaken. In the present case, positivity of IHC markers, vimentin and smooth muscle actin emphatically proved that BFH arose exclusively from the subcutaneous region, with no dermal origin. Also, a negative CD34 immunostaining, along with low B-cell lymphoma 2 (Bcl-2) expression ruled out DFSP (both are strongly expressed in DFSP), MFH and other malignant mesenchymal lesions. Negative CD 68 staining ruled out giant cell lesions and their congeners. This case is worth reporting, as it not only describes a rare case presentation of BFH, but as it also highlights the importance of IHC, thus helping to comprehensively clinch the diagnosis by systematically ruling out other differentials.
Subcutaneous, Benign fibrous histiocytoma, Immunohistochemistry
Case Report
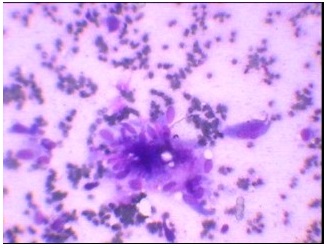
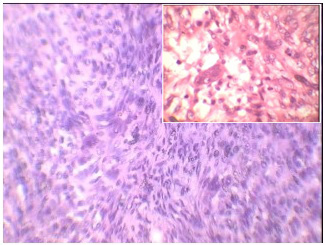
A 19-year-old female presented to the skin outpatient department with an apparently painful swelling on the medial side of her left thigh. On examination; a skin coloured, sessile, oval shaped, well circumscribed nodule, tender on touch (not associated with any elevated temperature), measuring 2.1x1.5x1.0 cm in size, was palpated. The patient was referred to the cytology department for fine needle aspiration cytology (FNAC) procedure, to ascertain its probable aetiology/nature. FNAC was done by using 22 G needles. 2-3 multiple passes were given from 2-3 different sites. The aspirates were blown on glass slides; a few of these were air dried and a few were wet fixed. May Grunwald’s Giemsa Stain (MGG) and Haemotoxylin and Eosin (H & E) staining were employed. Cytology showed a highly cellular lesion which comprised of oval to spindle cells which were arranged in clumps and sheets. Individual cells exhibited spindle shaped nuclei and abundant bluish cytoplasm [Table/Fig-1]. Nuclei of these cells were mostly benign, but they exhibited moderate pleomorphism at places. The background showed a few fibrovascular fragments and myxoid material. Based on these findings, a cytological diagnosis of a spindle cell rich (mesenchymal origin) lesion was suggested. It was decided to excise the lesion for histopathological examination. The H & E sections showed a poorly circumscribed spindle cell proliferation which was localized exclusively within the subepidermal region, which was admixed with an inflammatory cell infilterate which mainly comprised of lymphocytes and histiocytes [Table/Fig-2]. The spindle cells were arranged in bundles and they demonstrated vesicular nuclei with dispersed chromatin. Mitotic index was low (only 2 mitotic figure/10 HPF). Thus, histology also corroborated with the cytological findings of a benign mesenchymal tumour, with possibilities of a sub-cutaneous benign fibrous histiocytoma (BFH) and dermatofibroma protruberans (DFSP) being suggested. The excised surgical margins were free of tumour cells. To further subtype the tumour and for making a comprehensive diagnosis, IHC (immunohistochemistry) studies were recommended. On IHC, tumour cells exhibited strong immunoreactivity for vimentin and smooth muscle actin and they were found to be immunonegative for pancytokeratin, EMA, desmin, CD68 and CD 34. The Ki-67 Proliferative index was low (<2%). Hence, a final diagnosis of subcutaneous BFH was rendered. No recurrence was reported by the patient during her follow-up in skin outpatients department in one year.
Cytological smears show fair number of spindle cells. (MGG 400 X)
Section showing a poorly circumscribed spindle cell proliferation admixed with inflammatory cells. (H & E 200 X), inset showing (H & E 400 X)
Discussion
BFH (known by a number of names such as dermatofibroma, sclerosing haemangioma, xanthogranuloma, fibroxanthoma and nodular sub epidermal fibrosis) was not known as a clinical entity before 1970, when, as a result of the development of IHC techniques and electronic microscopy; its definite diagnosis became feasible [1,2].
Being first defined by Dahlin [3], BFHs are soft tissue tumours which are characterized by tumoural differentiations of fibroblasts and histiocytes with an unknown aetiology; which are commonly confined to the dermis or which extend into the superficial subcutaneous tissues [3]. Their location, exclusively in subcutaneous tissues is rare, whose incidence has been reported to be less than 1% of all benign fibrous histiocytomas [4,5].
BFH generally arises as a solitary and slow growing, painless, hyperkeratotic, brownish red solitary mass which is <1 cm in diameter, that protrudes from the skin in only 10% of cases. The presence of more than two lesions has also been reported in literature [6].
BFH constitutes a diagnostic dilemma for both clinicians and pathologists, because the lesions share common clinical symptoms, radiological characteristics and histological features with many benign and malignant lesions such as; non-ossifying fibromas, giant cell tumours, fibrous dysplasia, aneurysmal bone cysts, osteoblastomas, eosinophilic granulomas, chondrosarcomas, rhabdomyosarcomas, desmoid tumours, dermatofibromatous protuberans and malignant fibroma histiocytomas [7].
In the current case report, on histopathology alone; Dermatofibrosarcoma protruberans (DFSP) was the most important biological differential which was needed to be ruled out. In contrast to BFH, it arises from deeper dermis and aggressively invades the subcutaneous tissue and also carries an intermediate grade prognosis. Therefore, apart from a clinico-radiological correlation, currently; IHC is thought to be imperative, to make a conclusive diagnosis. In the present case, IHC studies emphatically proved that BFH arose exclusively from the subcutaneous region, with no dermal origin. Also, in the present case, CD34 immunostaining was negative, along with a low Bcl-2 expression (both are strongly expressed in DFSP) and its biological behaviour was confirmed by absence of any recurrence, as was revealed by the patient on follow up, as DFSPs often recur [2,3,8].
A negative CD 68 staining ruled out a giant cell tumour and negative desmin, cytokeratins and EMA staining ruled out most of the other close clinical mimickers. A low Bcl-2 expression ruled out MFH and other malignant congeners [9]. Hence, the present case was diagnosed as BFH which arose exclusively from subcutaneous region.
The present case report is worth publishing, as it not only documents a rare case of a purely sub-cutaneous BFH, but also emphasizes utilization of IHC studies for differentiating BFH from other mesenchymal lesions with similar presentations.
[1]. Hong KH, Kim YK, Park JK, Benign fibrous histiocytoma of the floor of the mouthOtolaryngol Head Neck Surg 1999 121:330-3. [Google Scholar]
[2]. Kamino H, Salcedo E, Histopathologic and immunohistochemical diagnosis of benign and malignant fibrous and fibrohistiocytic tumours of the skinDermatol Clin 1999 17:487-505. [Google Scholar]
[3]. Arikanoglu Z, Akbulut S, Basbug M, Meteroglu F, Senol A, Mizrak B, Benign fibrous histiocytoma arising from the intercostal spaceGen Thorac Cardiovasc Surg 2011 59(11):763-6. [Google Scholar]
[4]. Fletcher CD, Benign fibrous histiocytoma of subcutaneous and deep soft tissue: a clinicopathologic analysis of 21 casesAm J Surg Pathol 1990 14:801-9. [Google Scholar]
[5]. Chang SE, Choi JH, Sung KJ, Moon KC, Koh JK, Subcutaneous dermatofibroma showing a depressed surfaceInt J Dermatol 2001 40:77-8. [Google Scholar]
[6]. Han TY, Chang HS, Lee JH, Lee WM, Son SJ, A clinical and histopathological study of 122 cases of dermatofibroma (benign fibrous histiocytoma)Ann Dermatol 2011 23(2):185-92. [Google Scholar]
[7]. Kamino H, Jacobson M, Dermatofibroma extending into the subcutaneous tissue. Differential diagnosis from dermatofibrosarcoma protuberensAm J Surg Pathol 1990 14(12):1156-64. [Google Scholar]
[8]. Chung J, Namkoong S, Sim JH, Lee JS, Hong SP, Kim MH, Deep penetrating benign fibrous histiocytoma of the foot associated with throbbing painAnn Dermatol 2011 23(Suppl. 2):239-42. [Google Scholar]
[9]. Heim-Hall J, Yohe SL, Application of Immunohistochemistry to soft tissue neoplasmArch Pathol Lab Med 2008 132:476-89. [Google Scholar]