Neurilemmoma (Schwannoma) is a benign tumour of neuroectodermal origin. It usually occurs as a asymptomatic, solitary, smooth-surfaced and slow growing lesion, emerging at any age, with as such, no gender prelidiction. Occurring as a common tumour in the head and neck region, its intraoral presentation is very rare. Here, we are reporting a rare case of intraoral schwannoma of the posterior palate which occurred in a 34-year-old female patient who had chief complaint of a painless, slow growing swelling on posterior palate.
Antoni type A, Antoni type B, Intraoral schwannoma, Neurilemmoma, Palate
Case Report
A 34–year-old female patient reported to the department with chief complaint of a painless, slow growing swelling on posterior palate of right side, of 1 year’s duration. The swelling was round to oval, sessile, well circumscribed, which measured about 2cm x 1.5 cm, with no erythematous surface change and which was not associated with paresthaesia or discharge [Table/Fig-1]. On palpation, the swelling was found to be firm. The lymph nodes were non palpable and the patient did not give any relevant medical history.
Orthopantomographs did not reveal any significant finding in relation to maxillary posterior teeth. Based on the above clinical findings, provisional diagnoses of a benign tumour such as a lipoma or a pleomorphic adenoma on account of their slow growths and absence of neural symptoms, and also, a mucous retention cyst, a minor salivary gland tumour or a palatal abscess on account of their sites of occurrence, were considered.
Clinical picture of patient showing intraoral swelling on right side of posterior palate

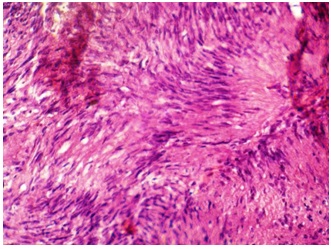
Photomicrograph showing histological section showing hypocellular Antoni type A areas (H&E, X10)
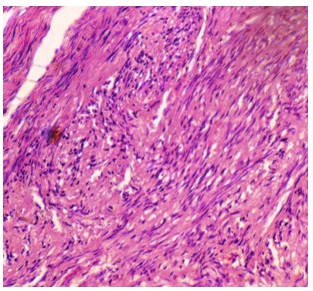
Photomicrograph showing histological section showing hypercellular Antoni type B areas (H&E, X10)
Discussion
A biopsy was performed and it was subsequently followed by a histological examination for making a confirmed diagnosis. All laboratory investigations which were carried out were found to be within normal limits before the surgical procedure. Tissue samples were submitted for a histopathological examination. Microscopic examination revealed a well-encapsulated lesion which was comprised of spindle shaped cells which were arranged in two peculiar cellular patterns. The first Antoni A pattern showed closely arranged bundles of Schwann cells with spindle-shaped nuclei which were aligned in parallel rows, which formed a typical palisading pattern around acellular, amorphous, eosinophilic masses, which represented the Verocay bodies [Table/Fig-2]. The second Antoni B pattern showed disorganized, hypocellular areas of fusiform cells which were distributed in a random fashion. In addition, few areas of hylanization and necrosis were also seen [Table/Fig-3]. Based on the histopathologic features, a definite diagnosis of an intraosseous schwannoma was made. The lesion was excised completely and post-perative period was uneventful.
Neurilemmoma (schwannoma) is a rare, benign, encapsulated perineural tumour of neuroectodermal origin that is derived from the Schwann cells of the neural sheath. Earlier (1910), Verocay referred to it as a “Neuronoma”. Later, Stout used the term, “neurilemmoma”, believing that this tumour is originated from the Schwann cells [1]. The origin of Schwann cells, according to some authors, occurs from proliferation of Schwann cells in the perineurium, causing displacement and compression of the adjacent nerve. Some think that they arise directly from the neural tube or from the neural crest [2]. Schwannomas most often involve the spinal nerve roots and the cervical, sympathetic, vagus, peroneal, and ulnar nerves [3]. They do not recur, and a malignant transformation is rare.
Being asymptomatic and slowly growing, schwanommas of the jaw commonly occur in the age range of 8-72 years, with an average age of about 34 years and with a definite female predilection[4]. Our case also presented a similar clinical picture in being asymptomatic and slow growing, also occurring in a female patient who was 34 years of age. Presentation of this lesion in oral cavity is infrequent and if it is present, it is found most commonly in tongue. Hatzoitis and Aspirides reported tongue to be the most common site intraorally, followed by palate, floor of mouth, buccal mucosa, gingiva, lips and vestibular mucosa [3]. In a review made by Leu and Chang [5], out of 52 cases of schwannomas which originated in the head and neck region, seven cases showed lesions which were located in the oral cavity, which included one in the hard palate, one in the soft palate, two in submasseteric area, one in the tongue, and one in lower lip. Intraosseous neurilemmomas, being still rare, represent less than 1% of all benign primary bone tumours [6]. But in our case, the location was palate, which was still rarer. Thus, the preoperative diagnosis was reasonably difficult and it led us to consider benign salivary gland neoplasms as differential diagnosis.
Radiographically, schwannomas present as unilocular radiolucencies with a thin sclerotic border, when they present intraosseously. They are also sometimes associated with external root resorptions and cortical expansions [4]. But in our case, we did not find any significant findings radiographically, because there was no cortical bone perforation which had an intraosseous presentation.
Microscopic examination revealed cellular Antoni A zones which often contained foci of nuclear palisading around cell processes (Verocay bodies) which were admixed with less cellular, partially myxoid Antoni B zones which closely resembled Neurofibromas. This was characteristic and suggestive of Schwannomas. The constituent Schwann cells have eosinophilic, fibrillar-appearing cytoplasm and elongated, wavy nuclei. The relative percentages of Antoni A and B zones vary greatly from case to case. Kumar et al., pointed out that a variety of secondary changes could commonly be seen, because of their long standing durations, before they were treated [7]. These could be thick walled, hyalinized blood vessels and extensive cystic changes, which resembled thrombosed blood vessels, with only a thin peripheral rim of neoplastic cells.
Immunohistochemistry acts as an adjunct in giving a definitive diagnosis. Schwannomas of all types are uniformly and intensely S-100 protein positive and they express glial fibrillary acidic protein (GFAP) in a majority of cases [8]. The pericapsular region of a schwannoma may contain EMA- and CD34- positive cells [9]. A very small minority of schwannomas may show rather extensive immunoreactivity with cytokeratin antibodies, which is thought to represent cross-reactivity with glial fibrillary acidic protein rather than true expression of cytokeratin proteins [10].
As this lesion was well-encapsulated, the treatment of choice was excision. In our case, connection with the nerve could not be seen,but if the nerve of origin is visualized, an attempt should be made to separate it carefully, to preserve its function. As the recurrence [11] and malignant transformation of neurilemmoma are exceedingly rare, the prognosis is usually very good.
Conclusion
Schwannomas rarely occur on unusual sites. Hence, they should not be spared, to be added to differential diagnosis, when any tumour is observed in the oral cavity, as we have reported in this case which has been presented. The definitive diagnosis can only be made after correlating the clincal, histopathological and immunohistochemical findings. The treatment of choice is complete surgical excision, as recurrences and malignant transformations of neurilemmomas are exceedingly rare.
[1]. LV Ackerman, FH Taylor, Neurogenous tumors within the thorax; a clinicopathological evaluation of forty-eight casesCancer 1951 4:669-91. [Google Scholar]
[2]. S Weirs, JR Goldblum, Enzinger and Weiss’s Soft Tissue Tumors. 2001 7194th Edition(725)Saint Louis MissouryMosby:1146-67. [Google Scholar]
[3]. JC Hatzoitis, H Aspirides, Neurilemmoma (schwannoma) of oral cavityOral Surg Oral Med Oral Pathol. 1967 24:510-26. [Google Scholar]
[4]. CA Chi, J Carey, S Muller, Intraosseous schwannoma of the mandible: A case report and review of literature.Oral Surg Oral Med Oral Path Oral Radiol Endod.:54-65. [Google Scholar]
[5]. SW Yang, CY Lin, Schwannoma of the upper lip: case report and literature review.Am J Otolaryngol. 2003 24:351-54. [Google Scholar]
[6]. K Patil, V Mahima, H Srikanth, D Saikrishna, Central Schwannoma of the mandible.J Oral Maxillofac Pathol 2009 13:23-6. [Google Scholar]
[7]. AK Bansal, R Bindal, DC Shetty, M Dua, Rare occurrence of intraosseous schwannoma in a young child, its review and its pathogenesisJ Oral Maxillofac Pathol 2012 16:91-96. [Google Scholar]
[8]. BW scheithauer, JM Woodruff, RA Erlandson, Tumors of the peripheral Nervous system. In Atlas of Tumor Pathology,Armed Forces Institute of Pathology 1999 3rd EditionWashington, DCfascicle 24:303-69. [Google Scholar]
[9]. AL Folpe, SD Billings, JK McKenney, Expression of claudin a recently described tight junction-associated protein, distinguishes soft tissue perineurioma from potential mimicsAm J Surg Pathol 2002 26:1620-26. [Google Scholar]
[10]. JC Fanburg-Smith, M Majidi, M Miettinen, Keratin expression in schwannoma; a study of 115 retroperitoneal and 22 peripheral schwannomas.Mod Pathol 2006 19:115-21. [Google Scholar]
[11]. SA De Lacerda, LG Brentegani, AL Rosa, MV Vespúcio, LA Salata, Intraosseous schwannoma of mandibular symphysis: Case report.Braz Dent J. 2006 17:255-8. [Google Scholar]