Dengue Fever (DF) is an old disease which is known by many names- break bone fever and dandy fever [1]. At the beginning of the 21st century; it is the most important arboviral disease observed among humans, with global reports going on the rise by an average of fivefold in the past 20 years [2]. Dengue is endemic or epidemic in almost every country which is located in the tropics [3]. A majority of Dengue cases are being reported from Asia, including India and it is a leading cause of hospitalization and death, especially among children [2,4]. The World Health Organization estimates that there may be 50 million to 100 million cases of Dengue virus infections worldwide every year, which may result in 250,000 to 500,000 cases of Dengue haemorrhagic fever (DHF) and 24, 000 deaths each year [5].
Historically, Dengue was considered to be a debilitating but not a fatal illness. During the late 1960s and 1970s, outbreaks of fatal Dengue haemorrhagic fever changed this perception [6,7]. Dengue viruses are maintained in transmission cycle, especially by the mosquito, Aedes aegypti. Others such as Aealbopictus and Aepolynesiensis are also involved. The incubation period is 4–7 days (range 3–14 days) [8,9].
The clinical spectrum of disease ranges from asymptomatic infection, mild Dengue fever to DF, DHF, or Dengue shock syndrome, which is frequently fatal. Consistent haematological findings, especially thrombocytopaenia [10] and unusual manifestations such as miocardiopathy, hepatic failure, and neurological disorders have been reported [11–13]. Mucosal involvement is seen in about more than 15-20% of patients, which most commonly involve conjuctival and scleral margins, soft palate, lips and tongue [14]. Oral lesions rarely occur and if they are present, they are often mistaken for platelet abnormalities. Stanford reported that more than 50% cases show manifestations in the soft palate [15]. Hence, oral physicians must be able to differentiate between the varied presentations of such cases.
Efforts made to decrease transmission by vector control have failed, and no effective antiviral treatment is available or foreseeable on the immediate horizon [12]. Hence, the importance of laboratory diagnosis of Dengue cannot be undermined. Serology is currently the method which is most widely applied for making its routine diagnosis [16], but one limitation is that it requires blood as a specimen for testing [17]. Salivary antibodies have been reported to be useful for the diagnosis of a number of infections and they have been widely studied in Acquired Immunodeficiency syndrome, leptospirosis, measles, mumps, Hepatitis A and B and rubella, among others [18,19]. But there are only few reports on Dengue IgM, IgA, and IgG detections in saliva samples [20]. This prompted us to conduct a pilot study to evaluate the presence of Dengue antibody, its sensitivity and specificity by ELISA by using saliva as diagnostic tool.
Materials and Methods
This study was carried out at M. S. Ramaiah Medical College and Hospital, Bangalore, India [20]. Seropositive patients with Dengue infection and 20 seronegative cases who were admitted to hospital, were considered. Consent for the study was obtained from every individual who participated in the study. Approval of ethical committee was also obtained. This study was carried out from June- September 2012.
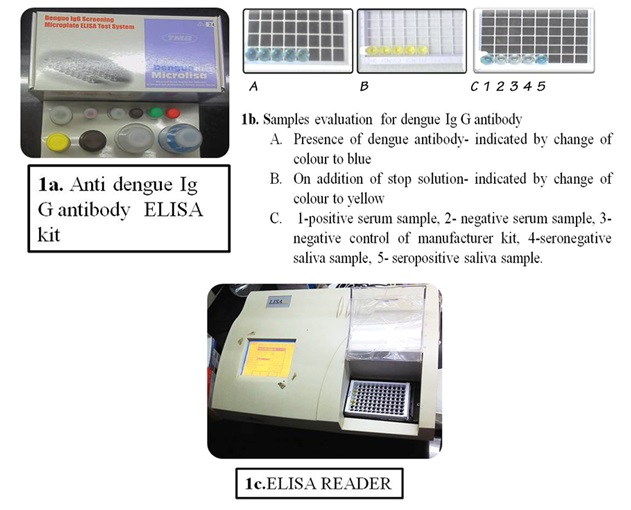
Unstimulated saliva samples were collected from both the groups on convenience in 20 ml wide mouthed bottles. The saliva collection was about 3 ml- 5 ml, which was stored immediately at -20 C until analysis. Before the procedure commenced, samples were thawed to room temperature. For Dengue virus detection, Ig G antibody detecting ELISA Kit, SD ELISA 3.0, was employed [Table/Fig-1a]. The procedure was standardized for detection of the antibody in saliva by running seropositive and seronegative cases, where the serum samples were used as controls [Table/Fig-1b]. As was instructed by the manufacturer, the ELISA procedure was carried out with a kit with which positive and negative controls were provided . On completion of the method, readings were obtained from an ELISA reader which was adjusted to the wavelength of 450 nm [Table/Fig-1c] and they were tabulated [Table/Fig-2].
Results of saliva samples for detection of Ig G dengue antibody
| Saliva Samples |
|---|
| Serum samples | Positive | Negative | Sensitivity | Specificity |
| Positive (n=20) | 20 | -- | 100% | 100% |
| Negative (n=20) | -- | 20 |
Results
By keeping a cut off value of 0.075, a sensitivity of 100 % and a specificity of 100 % were obtained. All the 20 seropositive cases of Dengue infection showed positivity on saliva samples, while all the 20 seronegative cases of Dengue infection showed negativity on saliva samples too. The inference which was noted here was that we obtained 100% sensitivity and 100% specificity when saliva was used as a diagnostic tool in our study.
Discussion
Accurate and efficient diagnosis of Dengue is not only of prime importance for case confirmation, but also for clinical and epidemiological surveillance and for vaccine evaluation [16]. Therefore, there is a great demand for a rapid detection of Dengue, in order to provide timely clinical treatment and for disease control [4,21].
Making a diagnosis of Dengue infection on the basis of clinical presentations alone is not reliable, because of its varied presentations, which can make accurate diagnosis difficult [21,22]. In recent years, many diagnostic tools have become available for Dengue [17]. The routine laboratory diagnosis of Dengue virus infection is serodiagnosis, which is primarily achieved by detection of antigens or antibodies, isolation of virus in tissue culture, or molecular detection by the demonstration of viral RNA [21,23][Table/Fig-3].
Laboratory Methods For the diagnosis of dengue [4,22,24]
| Direct Method | Method | Advantages | Disadvantages | Technique |
| Virus detection | For confirmation Specific test Serotypes can be identified | Requires expertise and appropriate facilities expensive | Culture |
| Viral RNA* detection | PCR** |
| NS1 Antigen Detection | Diagnosis during the acute stage of infection Less expensive Easy to perform | Antigen detection in the acute stage of secondary infections can be compromised by pre-existing virus– immunocomplexes | ELISA**** RIA***** |
| Indirect Method | IgM antibody detection | Initially detectable between 3 to 5 days post onset of fever Less expensive Easy to perform | IgM levels are significantly lower in secondary dengue infections | ELISA Lateral flow Particle agglutination test |
| IgG antibody detection | Used to determine whether an infection is a primary or a secondary infection Less expensive Easy to perform | IgG levels are significantly lower during the initial stages of primary dengue infections | ELISA HAI test****** |
*RNA- Ribonucleic acid, **PCR- Polymerase chain reaction, ***NS1- Non Structural protein 1, ****ELISA- Enzyme linked immunosorbent assay, *****RIA- Radioimmuno assay, ******HAI-Haemagglutination-inhibition test
Several methods have been employed for serological detection of Dengue virus-specific antibodies, such as haemagglutination inhibition (HI) test, the neutralization test, the indirect immunofluorescent- antibody test, ELISA, complement fixation, to name a few. Among these, capture IgM and/or IgG ELISA, antigen- coated indirect IgM and/or IgG ELISA, and the HI test are the serological techniques which are most commonly used for the routine diagnosis of Dengue virus infections [18, 21]. Currently, serum and more recently, saliva samples are being utilized for anti-Dengue IgG detection diagnosis [16].
Potential problems which occur with the use of serum include the requirement of consent and cooperation of the patient, the need of a trained venipuncturist, the need to separate serum before testing and the difficulty and added risk of venipuncture in children, the group which is most commonly affected by Dengue in areas where infection is endemic [18]. On the contrary, saliva, being non-invasive, cost effective, easy to collect, available in sufficient quantity and easy to store and transport; with no need of auxiliary personnel and having simplified, repeated sample collection, is particularly useful for epidemiological studies. Saliva sample collection has been shown to have a significant comfort and convenience level as compared to urine and blood [25].
Considering the endemicity, varied clinical presentations and the challenges/disadvantages of serum collection, we wanted to evaluate the presence of the IgG Dengue antibody and its sensitivity and specificity by ELISA in saliva samples. Among the 20 seropositive patients, there were seven paediatric patients of age group – four years to 12 years, including a case of Down’s syndrome case. Six patients had a history of duration of fever of more than ten days, which they had neglected, until it had turned severe. Seven patients were admitted to the intensive care unit. Based on these observations, we interpreted that the symptoms of Dengue were non-specific in initial stages, which had probably led to negligence by the patients and difficulty in making a diagnosis, which was faced by physicians. Also, all age groups can be affected by this viral infection and it can be severe. We obtained prior information from the incharge faculty and only when patients were in stable condition, did we go ahead with sample collection. Our study received good response from the patients when we requested for saliva sample collection and their participation when we explained about the study to them. We also got the same level of co- operation from all the paediatric patients and their attenders and they were more than willing to oblige. In spite of the reduced volume of saliva which was obtained from most of the paediatric and intensive care unit patients, which was less, with a range of 2-3 ml, the quantity was more than sufficient for the study.
Though the literature shows that various antibodies [Table/Fig-4] such as Ig A, Ig M, Ig E antibodies are detectable in diagnosis of Dengue on using saliva, we chose to evaluate the presence of Ig G antibody in saliva for the following reasons:
Literature Review of Various Antibodies Detected In the Saliva of Dengue Patients [18, 20, 26, 27]
| Numbers | Percentage (n=17) |
|---|
| Author | Dengue Antibody detection by ELISA | Sensitivity | Specificity | Advantages | Disadvantages |
| Andrea J. Cuzzubbo | Ig G & Ig M | Overall 92% for both primary and secondary patients | 100% | Salivary IgG levels correlated well with serum HAI titer Salivary IgG levels could be used to distinguish between primary- and secondary-dengue virus infections. | Patients with primary-dengue infections had elevated levels of IgM without detectable IgG, Majority of patients with secondary dengue (86%) showed elevated levels of IgG with or without detectable IgM. |
| Angel Balmaseda | Ig M & Ig A | Ig M- 90.3% Ig A- 94.4 % | Ig M- 92% Ig A- 74.7% | Salivary IgM may not be bound to antigen and therefore may be detected better in the assay rather in serum | The low sensitivity of Ig A marker could be due to the high concentration of nonspecific IgA present in saliva that can compete with DENspecific IgA |
| S. Vázquez et al., | Kinetics of IgM, IgA,Ig E and IgG in serum, saliva, and urine samples from adult patients with primary or secondary dengue infection | | | In saliva, 100% of primary and secondary cases showed a positive IgM at days 6 and 7, respectively A 100%positive IgA response in serum in primary and secondary cases was observed at day 7 All secondary cases were positive to IgG in saliva and urine samples at day 7 | The IgA values were lower than IgM both in serum and saliva. The IgM and IgA OD values and the geometric mean titer of IgG antibodies were lower in saliva than in serum samples. |
| Angel Balmaseda et al., | IgM, IgA, and IgG in serum, filter-paper blood spots, and saliva | Ig M- 39.3 Ig G-81.8 | Ig M- 71.0 Ig G- 80.6 | In contrast to serum and filter-paper blood spots, detection of IgM and IgA in saliva was greater in primary than in secondary dengue cases Detection of IgG alone in serum, filter-paper blood spots, or saliva functioned best for measuring DENV infection | Intermediate and poor results were obtained in saliva for IgM and IgA, respectively |
| Grace Yap et al., | IgA | Ig A Primary infection-36% Ig A Secondary infection-100% | 97 % | Saliva is known to be rich in IgA, the concentration of which is 100 times greater than that of IgM and 14 times greater than IgG | IgA was short-lived compared to IgM Anti-DENV IgA typically appeared after IgM |
1. Due to its high sensitivity, specificity, simplicity, and feasibility for automation [21].
2. As it is useful for sero-epidemiological studies, for identifying past Dengue infections [3].
3. Anti-Dengue IgG appears in a low titre at the end of the first week of disease onset, and it increases slowly. High levels of IgG are detectable, even in the acute phase and they rise dramatically over the following two weeks.
Cardosa et al., demonstrated that the IgG response was specific and no that cross-reaction was observed when sera were tested from individuals who were infected with Dengue virus or Japanese Encephalitis virus [28]. Also, an excellent specificity of anti-Dengue-specific IgG assay was obtained by Buchy et al., [29]. IgG avidity ELISAs can be used to determine as to whether an infection is primary or secondary, and they can be more useful than the haemagglutination inhibition test which is used for this purpose [29].
In our study, the sample size was small. This was major limitation of our study. Though we got good response for conducting the study from the patients, laboratory procedures, including time were similar to serum, minimal amount of saliva was required, cross infection with the laboratory personnel was avoided and most importantly, the sensitivity and specificity were good.
Other than saliva, various other diagnostic samples such as urine, filter paper blood spots have been utilized, with satisfactory results. Although detection of IgG in saliva was less sensitive than that seen in serum or filter-paper blood spots, it is an acceptable and attractive marker which can be used for community-based studies, because of its non-invasive nature. It was the method of choice for monitoring Dengue infection in children, in a large study which was done on community participation in mosquito control and Dengue prevention in Managua, Nicaragua over the past four years [27]. Hence, saliva could be used as alternative selective sample when blood samples were difficult to obtain, e.g., in newborns and patients with haemorrhagic syndromes [30].
Investigators have detected a large number of viruses in oral samples by using antigen, antibody or nucleic acid targets. The literature on salivary-based antibody tests which are used for detection of viral infections is extensive. Clinicians can use a number of oral samples to diagnose viruses, including whole saliva, gingival crevicular fluid, oral swabs of mucosal tissue, and so on. Saliva remains an attractive biological matrix for Point-Of-Care diagnosis, especially when focus is made on applications made in remote settings or home-care situations. Salivary tests, although they are rapidly increasing in use, still constitute a minority of all diagnostic tests which are performed [31].
Acknowledgements
We would like to sincerely thank Dr. Indumathi, Professor and HOD, Dr. Gayathri, Professor and Lab Technicians from Department of Microbiology, M S Ramaiah Medical College and Hospital, all the faculty members of Department of Oral Pathology, M S Ramaiah Dental College and Hospital and everyone who was involved in the study, for their suggestions and contributions.
Conclusion
Based on our results on 100% sensitivity and specificity, we could hypothesize that saliva played a pivotal role in diagnosis of Dengue.The sample size that we considered for our study was minimal. This necessitates further research for implementation of this study to a larger population, which can lead to a diagnostic revolution with greatest impact, especially in the most remote or impoverished communities. Diagnostic abilities of saliva and ELISA, together can potentially improve surveillance and early detection of cases; facilitate implementation and initiation of treatment at an earlier stage, which in turn can translate to prompt Dengue control efforts.
*RNA- Ribonucleic acid, **PCR- Polymerase chain reaction, ***NS1- Non Structural protein 1, ****ELISA- Enzyme linked immunosorbent assay, *****RIA- Radioimmuno assay, ******HAI-Haemagglutination-inhibition test