Paediatric patients encompass a very interesting study group, as several long term physiological changes take place in the maxillofacial area. During the mixed dentition period, children can report with complaint of swelling in the maxillofacial area, which may or may not be associated with pain. A history of trauma also needs to be elicited, because they are prone to falling down during playing, which can affect the jaws. Any intraosseous pathology which is detected should be treated, while keeping in mind the various developmental changes which take place in the transitional dentition. Numerous studies on the prevalence of maxillofacial pathologies in the paediatric patients have been published [1–4]. These mostly include both hard and soft tissue pathologies. When involving bone, only odontogenic cysts or odontogenic tumours as a category have been considered. Intra-osseous paediatric jaw lesions can present in diverse clinical patterns and their diagnoses can vary from odontogenic to non-odontogenic pathogeneses, which can rarely include connective tissue pathology. Clinicians need to keep abreast of the various intra-osseous lesions with their presenting signs and symptoms, so that the patient can be treated without any delay and avoiding unnecessary administration of antibiotics.
Hence, this study was undertaken to comprehensively analyze the distribution of intraosseous paediatric jaw lesions (in the age group of 0-16 years), which had reported to the institution.
Materials and Methods
The data stored in the Department of Oral Pathology, Maulana Azad Institute of Dental Sciences was retrieved for retrospective study from the time detailed biopsy records were available i.e. September 2006 to November 2012. A detailed analysis of paediatric cases was undertaken to segregate intraosseous pathology from soft tissue pathology.
Following inclusion criteria were considered
All intra-osseous cases with evidence of radiographic changes in bone were included.
In included cases of fibrous dysplasa and round cell tumours, records which were available were only incisional in nature.
In certain cysts, direct excisional tissues were received.
Exclusion criteria
Any soft tissue pathology showing superficial erosion of bone was excluded from the study.
A total of 171 lesions were identified as intraosseous paediatric pathology (from age 0-16 years) during the study period. All the cases were analyzed with respect to gender, anatomic location, radiographic features, histopathological diagnosis, treatment and recurrence rate. Since the study encompassed a detailed analysis of paediatric intraosseous jaw lesions, an attempt was made to decipher the various radiographic presentations with respect to histopathological diagnoses.
Results
The retrospective analysis of data revealed 3,756 biopsied cases being reported from September 2006 to Novmeber 2012, out of which, the paediatric intraosseous lesions were 171 in number. The present study revealed 54/171 odontogenic cysts, 45/171 odontogenic tumours, 33/171 bone pathologies, 2 malignant tumours, 1 connective tissue pathology and 36/171 miscellaneous cases.
Cases
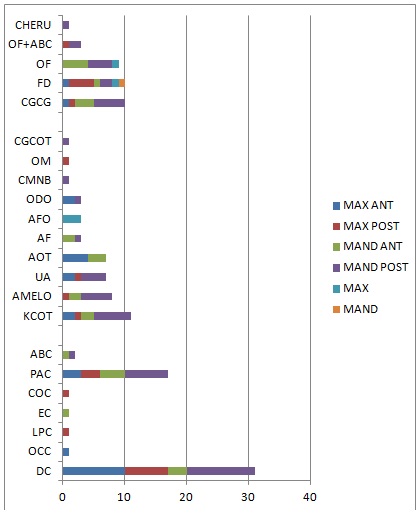
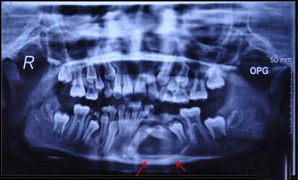
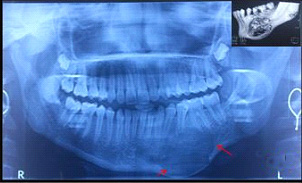
[Table/Fig-1] shows the distribution of odontogenic cysts with dentigerous cyst (DC) (n=31) being the predominant type followed by radicular cyst (RC) (n=17). DC showed a high male predilection, with posterior mandible being the preferred site [Table/Fig-2]. Twenty-six out of 31 cases showed unilocular radiolucencies [Table/Fig-3] which were associated with an impacted tooth [Table/Fig-4]. RC exhibited a female predilection with a preponderance for posterior mandibular site [Table/Fig-2]. Fifteen cases showed unilocular radiolucencies which were associated with non vital teeth. One case showed a multilocular radiolucency and one case showed a mixed radiolucent-radiopaque appearance [Table/Fig-4].
Shows the distribution of odontogenic cysts
| Odontogenic Cyst | No. | Gender | Site | Radiograph | Treatment |
|---|
| Dentigerous Cyst* | 31 | Male=25 Female=6 | 1†=10, 2‡=7, 3§=3, 4||=11 | ULRL**=31, IMP††=26 | Enucleation=26/31 Marsupialization=5/31 |
| Orthokeratinised Odontogenic Cyst | 1 | Male=0 Female=1 | 1†=1, 2‡=0, 3§=0, 4||=0 | ULRL**=1 IMP††=1 | Enucleation=1/1 |
| Lateral Periodontal cyst | 1 | Male=0 Female=1 | 1†=0, 2‡=1, 3§=0, 4||=0 | ULRL**=1 | Enucleation=1/1 |
| Eruption Cyst | 1 | Male=1 Female=0 | 1†=0, 2‡=0, 3§=1, 4||=0 | ULRL**=1, UE†††=3 teeth | Enucleation=1/1 |
| Calcifying Odontogenic Cyst | 1 | Male=1 Female=0 | 1†=0,2‡=0, 3§=0, 4||=1 | ULRL**=1 | Enucleation=1/1 |
| Inflammatory Cyst |
| Periapical cyst | 17 | Male=6 Female=11 | 1†=3, 2‡=3, 3§=4, 4||=7 | ULRL**=15, MXRL‡‡=1,MLRL***=1 | Enucleation=14/17, Enucleation + apicoecotomy=3/17 |
| Pseudocyst |
| Aneurysmal Bone Cyst | 2 | Male=1 Female=1 | 1†=0,2‡=0,3§=1,4||=1 | ULRL**=1, MXRL‡‡=1 | Surgical removal + Curettage=2/2 |
* Including inflammatory Dentigerous Cyst, † =Anterior maxilla, ‡=Posterior Maxilla, §=Anterior Mandible, ||= Posterior Mandible, **=Unilocular radiolucency, ††=Impacted tooth, ‡‡= Mixed radiolucency, ***=Multilocular radiolucency, †††= Unerupted
Show the site variation in odontogenic cysts, odontogenic tumours and bone pathologies
DC= Dentigerous cyst, OCC= Orthokeratinized Odontogenic cyst, LPC=Lateral periodontal cyst, EC= Eruption cyst, COC= Calcifying Odontogenic cyst, PAC= Periapical cyst, ABC= Aneurysmal bone cyst, KCOT=Keratinizing Cystic odontogenic Tumour, AMELO= Ameloblastoma, UA= Unicystic ameloblastoma, AOT= Adenomatoid Odontogenic tumour, AF= Ameloblastic fibroma, AFO= Ameloblastic fibro odontoma, ODO= Odontoma, CMNB= Cementoblastoma, OM= OdontohenicMyxoma, CGCG= Central giant cell Granuloma, FD= Fybrous dysplasia, OF= Ossifying fibroma, CHERU= Cherubism, MAX ANT=Maxillary anterior, MAX POST= Maxillary Posterior, MAND ANT= Mandibular anterior, MAND POST= Mandibular posterior, MAX= Maxilla, MAND= Mandible
Shows well-defined unilocular radiolucency extending from 32-36 with impacted 33 & 34 (Dentigerous cyst)
Show the radiographic findings in odontogenic cysts, odontogenic tumours and bone pathologies
DC= Dentigerous cyst, OCC= Orthokeratinized Odontogenic cyst, LPC=Lateral periodontal cyst, EC= Eruption cyst, COC= Calcifying Odontogenic cyst, PAC= Periapical cyst, ABC= Aneurysmal bone cyst, KCOT=Keratinizing Cystic odontogenic Tumour, AMELO= Ameloblastoma, UA= Unicystic ameloblastoma, AOT= Adenomatoid Odontogenic tumour, AF= Ameloblastic fibroma, AFO= Ameloblastic fibro odontoma, ODO= Odontoma, CMNB= Cementoblastoma, OM= OdontohenicMyxoma, CGCG= Central giant cell Granuloma, FD= Fybrous dysplasia, OF= Ossifying fibroma, CHERU= Cherubism. RL=Radiolucent, RO=Radiopaque, WD= Well defined, ILD=ill defined, UE=unerupted, Exp= Expansile, ML=Multilocular UL= Unilocular, SCLR=Scelorsed. MIX=Mixed
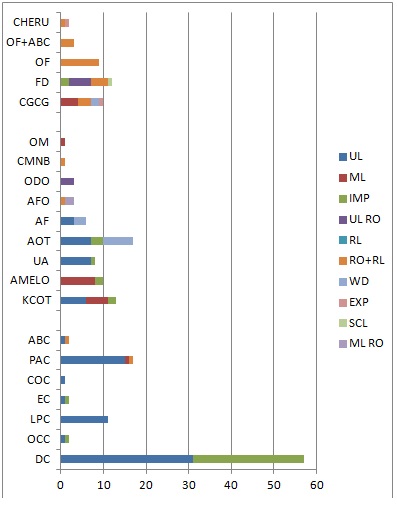
The results for odontogenic tumours are summarized in [Table/Fig-5]. The predominant types noticed were keratocystic odontogenic tumour (KCOT) (n=11), ameloblastoma (n=8), unicysticameloblastoma (UA) (n=7), adenomatoidodontogenictumour (AOT) (n=7), and others. KCOTs showed an almost equal sex predilection, with posterior mandible being the favoured site [Table/Fig-2]. Unilocular radiolucencies were observed in five cases, multilocular radiolucencies were observed in four cases and only two cases showed associations of impacted teeth with unilocular radiolucencies [Table/Fig-4].
summaries the details of odontogenic tumours
| Odontogenic Tumour | NO. | Gender | Site | R/G | Treatment |
|---|
| Keratocystic odontogenic Tumour (KCOT) | 11 | Male=6 Female=5 | 1*=2, 2†=1, 3‡=2, 4§=6 | ML RL||=5, UL RL**=6, IMP††=2 | Resection=5/11, Enucleation=6/11 |
| Ameloblastoma |
| Follicular | 3 | Male=1 Female=2 | 1*=0, 2†=0, 3‡=1, 4§=2 | ML RL|| =3 | Enucleation-1/3 Segmental resection =2/3 |
| Plexiform | 4 | Male=2 Female=2 | 1*=0, 2†=0, 3‡=1, 4§=3 | ML RL||=4, IMP††=2 | Enucleation followed by curettage= 2/4 Segmental resection =2/4 |
| Basal | 1 | Male=0, Female=1 | 1*=0, 2†=1, 3‡=0, 4§=0 | ML RL||=1 | Segmental resection =1/1 |
| Unicystic (UA) Ameloblastoma | 7 | Male=3 Female=4 | 1*=2, 2†=1, 3‡=0, 4§=4 | UL RL**=7, IMP††=1 | Enucleation 7/7 |
| Adenomatoid odontogenic Tumour (AOT) | 7 | Male=2 Female=5 | 1*=4, 2†=0, 3‡=3, 4§=0 | UL RL**, WD***=7 IMP††=3 | 7/7 Enucleation |
| Ameloblastic fibroma (AF) | 3 | Male=3 Female=0 | 1*=0, 2†=0, 3‡=2, 4§=1 | UL RL**=3, WD***=3 | 3/3 Enucleation |
| Ameloblastic fibro-odontoma (AFO) | 3 | Male=3 Female=0 | 1*=0,2†=0, 3‡=0, 4§=3 | MXRL‡‡=1, MLRO§§=2 | 3/3 Enucleation |
| Odontoma (O) | 3 | Male=3 Female=0 | 1*=2, 2†=0, 3‡=0, 4§=1 | UL RO||||=3 | 3/3 Enucleation |
| Cementoblastoma | 1 | Male=1 Female=0 | 1*=0, 2†=0, 3‡=0, 4§=1 | MXRL‡‡=1 | 1/1 excision + Extraction |
| Odontogenic Myxoma | 1 | Male=1 Female=0 | 1*=0, 2†=1, 3‡=0, 4§=0 | ML RL||=1 | 1/1 Excision with wide margin with close follow up |
| Calcifying Ghost Cell Odontogenic Tumour | 1 | Male=1 Female=0 | 1*=0, 2†=0, 3‡=0, 4§=1 | MX RL‡‡=1 | – |
*=Anterior Maxilla, †= Posterior Maxilla, ‡= Anterior Mandible, §= Posterior Mandible, ||=Multilocular radiolucency, **= Unilocular radiolucency, ††= Impacted, ‡‡= Mixed Radiolucency, §§=Multilocular radiopacity, ||||=Unilocularradiopacity, ***= Well defined
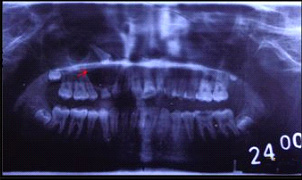
With respect to ameloblastomas, females showed a slightly higher prevalence. Most common site of occurrence was posterior mandible [Table/Fig-2]. All cases showed multilocular radiolucencies [Table/Fig-6]. Two cases showed associations with impacted tooth [Table/Fig-4]. Similar results were seen with respect to sex and site for UA, with unilocular radiolucencies being predominant [Table/Fig-4]. AOT showed a high female predilection with preponderance for anterior maxilla [Table/Fig-2]. All cases were well-defined unilocular radiolucencies [Table/Fig-4,7].
Shows soap bubble appearance at right angle of mandible (Ameloblastoma)

Shows well-defined circumscribed radiolucency with impacted maxillary right first premolar (Adenomatoid odontogenic tumour)
The distribution of bone pathology is explained, which showed almost an equal number of cases of Central Giant Cell Granuloma (CGCG), Fibrous Dysplasia (FD) and Ossifying Fibroma (OF). Male/female ratio was 0.6:1. Twenty-three cases showed involvement of mandible, while 10 cases showed involvement of maxilla. CGCGs showed male and posterior mandible predilections, whereas FD showed predilections for females and posterior maxillary region respectively [Table/Fig-2]. However, two cases were found to show involvements of both maxillary and mandibular anterior and posterior segments [Table/Fig-2]. OFs showed a female predilection, with mandible being the site of occurrence [Table/Fig-8]. The radiographic appearance [Table/Fig-4] was varying as represented in the [Table/Fig-4,9].
Shows expansile osteolytic lesion from 33 till 37 region with bowing of inferior border of mandible. Inset: CT shows well circumscribed mixed radiolucent-radiopaque lesion (Ossifying fibroma)
Summaries the distribution of bone pathology
| Bone Pathology | No. | Gender | Site | R/G | Treatment |
|---|
| Central Giant Cell Granuloma | 10 | Male=6 Female=4 | 1*=1, 2†=1, 3‡=3, 4§=5 | WD RL††=2, MLRL‡‡=4, EXP§§=1, MXRL||||=3 | curettage=5/10, resection=5/10 |
| Fibrous Dysplasia | 10 | Male=2 Female=8 | 1*=1, 2†=4, 3‡=1, 4§=2 1+2||=1, 3+4**=1 | MIX RL||||=4,RO***=4, RL†††=1, SClR=1, IMP||||||=2 | recontouring=10/10 |
| Ossifying Fibroma | 9 | Male=3 Female=6 | 1*=0, 2†=0, 3‡=4, 4§=4 1+2||=1 | MX RL||||=9 | Surgical excision=9 |
| Ossifying Fibroma + Aneurysmal Bone Cyst | 3 | Male=1, Female= 2 | 1*=0, 2†=1, 3‡=0, 4§=2 | MX RL||||=3 | Surgical excision=1,marginal resection=1, Curettage=1 |
| Cherubism | 1 | Male=1 Female=0 | 1*=0, 2†=0, 3‡=0, 4§=1 | MLRL‡‡+ EXP§§=1 | Recontoured=1 |
*=Anterior Maxilla, †= Posterior Maxilla, ‡= Anterior Mandible, §= Posterior Mandible, ||= Anterior & Posterior maxilla, **=Anterior & Posterior Mandible, ††=Well defined radiolucency, ‡‡= Multilocular radiolucency, §§=Expansile, ||||= Mixed radiolucency, ***= Radiopacity, †††=Radiolucency, §§§=Sclerosed, ||||||=Impacted tooth
Connective tissue pathology was extremely rare, with one case of myofibroma and one case of malignancy, namely, “round cell tumour” being reported in our institution. Three cases showed recurrences in the present study. AOT exhibited recurrence within a short duration of 11 months. One case of dentigerous cyst showed transformation into a Calcifying Ghost Cell Odontogenic Tumour (CGCOT) after a period of four years. Another recurrence was noted in fibrous dysplasia which had reappeared after three years.
[Table/Fig-10] encompasses the miscellaneous groups, connective tissue pathologies, malignant lesions (round cell tumour) and their distribution.
Summaries the distribution of miscellaneous group, connective tissue pathology and malignant lesion
| Miscellaneous | No. | Gender | Site | R/G | Treatment |
|---|
| Periapical granuloma | 5 | Male=3 Female=2 | 1*=0, 2†=3, 3‡=2, 4§=0 | UL RL††=5 | Associated tooth extracted + curettage=1, Surgical excision with apicoectomy=4 |
| Chronic infection | 6 | Male=4 Female=2 | 1*=0, 2†=0, 3‡=2, 4§=4 | UL RL††=5, ILD RL**=1 | - |
| Chronic granulation tissue | 1 | Male=0 Female=1 | 1*=0, 2†=0, 3‡=0, 4§=1 | RL||=1 | Curettage=1 |
| Chronic Osteomyelitis | 1 | Male=0 Female=1 | 1*=0, 2†=0, 3‡=0, 4§=1 | RL||=1 | - |
| Primitive follicular tissue | 1 | Male=1 Female=0 | 1*=0, 2†=1, 3‡=0, 4§=0 | - | - |
| Cyst wall | 12 | Male=8 Female=4 | 1*=0, 2†=4, 3‡=3, 4§=5 | RL||=12 | Enucleation=12 |
| Infected keratinizing cyst | 5 | Male=2 Female=3 | 1*=1, 2†=1, 3‡=2, 4§=1 | RL||=5 | Enucleation=5 |
| Early cyst | 2 | Male=1 Female=1 | 1*=0, 2†=0, 3‡=1, 4§=1 | RL||=2 | Curettage=2 |
| Infected non keratinising cyst | 3 | Male=1 Female=2 | 1*=1, 2†=0, 3‡=2, 4§=0 | RL||=3 | Enucleation=1Curettage + Extraction=2 |
| Connective tissue pathology |
| Myofibroma | 1 | Male=1 Female=0 | 1*=0, 2†=0, 3‡=0, 4§=1 | UL RL†† + Exp‡‡=1 | Resection |
| Malignant lesions |
| Round cell tumour | 2 | Male=1 Female=1 | 1*=0, 2†=0, 3‡=0, 4§=2 | RL||=2 | Referred for further treatment |
*=Anterior Maxilla, †= Posterior Maxilla, ‡= Anterior Mandible, §= Posterior Mandible ||=Radiolucency, **=Ill Defined Radiolucency, ††= Unilocular radiolucency, ‡‡=Expansile
Discussion
Analysis of data of the current study showed a predominance of odontogenic cysts (31.5%), followed by odontogenic tumours (26.3%) in the paediatric age group of 0-16 years. Intra-osseous jaw lesions comprised only 4.55% of the total biopsies which were received in the institute. Jones & Franklin have noticed an occurrence of 8.2% which included both hard and soft tissue pathologies with the incidence of odontogenic cysts being 11.78% and that of odontogenic tumours being 5.52% [1]. Our study has shown a substantial increase in incidence of odontogenic cysts and tumours. The institute which was under consideration, being a tertiary referral institute, could only partially account for this high incidence rate. The present study revealed a male predominance (1.3:1). Our study showed an increased number of cases in posterior mandible region, with involvement of mandible: maxilla in a 1.2:1 ratio. Information for predominant mandibular localization has been given by Lawoyin [2] and is in contrast with the data of Salako and Taiwo [3] and Lima et al., [4] who found more frequent afflictions in the maxilla. Lima et al.,’s study included both hard and soft tissues [4]. Hence, a direct comparison would not be fruitful.
Data received in the present study showed prevalence of DC (57%), followed by RC (31%). This was in confirmation with findings of Dhanuthai et al., who reported that DC was the most frequent oral pathology which was seen [5]. Similarly, Bodner also showed that 45% of cystic lesions seen in children were DC, while RC represented only 13.3% of such leasions [6]. Manor et al have attributed that RCs arising from primary teeth are very rare. RCs arising from permanent teeth in the Paediatric age are also infrequent because RC arises from epithelial remnants in the periodontal ligament as a result of inflammation that follows necrosis of dental pulp. Recently erupted permanent teeth, as in the Paediatric age are usually intact [7].Opposing results were shown by Skiavounou et al., wherein RCs were the most frequent type (36.3%), followed by DC (18%) [8]. In current series of cases, DC showed association with impacted teeth in 26/31 cases, with mandibular premolar region being predominantly afflicted. This was well consistent with Shibata et al.,’s findings [9]. Hence DC in relation to these impacted teeth was quite common in the transitional dentition.
Odontogenic tumours constituted 26.3% cases, which represented quite a huge number of cases, which was in contrast to findings of study of Jones and Franklin., and other researchers, which showed that odontogenic tumours were rare in children [1].Odontogenic tumours showed a male predilection in our study, with maximum number of cases being seen in posterior mandible, whereas the study of Jones and Franklin, showed a female predilection [1]. KCOT showed unilocularity (6/11) and multilocularity (5/11) patterns radiographically, with only two cases showing association of impacted tooth. Shear suggested that larger lesions which were seen mainly in the third molar mandibular ramus area, were usually multilocular [10]. Six out of eleven cases seen in the present study were enucleated.Enucleation provides the advantage of preservation of anatomical structures, including teeth. This was advocated because KCOTs are commonly present in younger patients [7]. Browne proposed that recurrence of the keratocysts was caused by the nature of lesion itself i.e. the presence of additional remnants of dental lamina from which a cyst could develop, and which was not related to its method of treatment [11].
Ameloblastomas are rare in children [12]. It was also observed radiographically that, follicular variant showed multilocularity, but that plexiform variant showed multilocularity, unilocularity in association with impacted teeth. In our study, one case was enucleated, 5/8 cases underwent segmental resections and two cases were enucleated, followed by curettage. While treating ameloblastomas in children, few authors advocated only enucleations [13] or minimal treatment [14]. Fung stated that in younger patients, there would be maximum cancellous bone, with the lesion growing more rapidly, with extensive destruction [15].Hence, segmental resections which were advocated in five cases appeared to have been an appropriate treatment modality.
According to Ord et al., majority of ameloblastomas in children are unicystic [12]. However, in the current study, UA was only one less in number as compared to conventional ameloblastoma. Unilocularity was noticed in maximum number of cases, with only one case showing association with impacted tooth. Hence, the non dentigerous variant was predominantly encountered in our study, which resembled the finding of study of Philipsen and Reichart, where non dentigerous variants predominated dentigerous variants [16].
AOT shows female predilection with propensity towards anterior maxilla [17]. Similar findings were noticed in the current study also. However, only three cases were associated with impacted teeth. Hence, extra follicular variant showed predominance over follicular variant, which appeared to be a unique finding, which was in contrast with the findings of Philipsen and Reichart, who showed predominance for follicular variant [18].
Odontoma comprised a very low percentage in the present study. This can be attributed to odontomas being asymptomatic or being discovered on routine radiographic examinations done for other reasons [19].
With respect to bone pathology, CGCGs were observed in 10/33 cases in the present study, which was similar to Saxena et al.,’s finding [20]. OFs showed a female predilection in the present study, which was similar to finding of Scholl RJ et al., [21]. Mandibular predominance in OF is seen similar to Liu Y et al.,’s finding [22]. Radiographic patterns vary according to the degree of mineralization. Associations of aneurysmal bone cysts with OFs were also noted, but they were only few (3/33) in number, which presented with aggressive and reactive behaviours, which caused a significant facial asymmetry, according to Silva et al., [23].
AOT is a benign lesion, although the tumour can enlarge. It is not invasive & does not recur after conservative surgery [24]. However, we noticed recurrence in one case. FD recurred after three years. This suggested that regrowth after a surgical reduction seemed to be more common in younger individuals. Hence, surgery should be delayed [25]. Transformation of DC into CGCOT after four years was noticed, which is a unique finding in this study. To conclude, a clinicopathological correlation is necessary for making an appropriate diagnosis, since the radiographic patterns may overlap in a variety of conditions. In the current study, preponderance of odontogenic pathosis, which comprised mainly of dentigerous cysts, keratocystic odontogenic tumours and ameloblastomas (solid and unicystic), were noted in the paediatric age groups which were studied.