Alkaptonuric Arthropathy with Periprosthetic Fracture:A Case Report
S Durgaprasad Hegde1, Siva Ranjan D2, Muralidhar B.M3, Epari Sanjeeva Rao4, P.S.B. Hussain5
1Senior Resident, Department of Orthopaedics, Konaseema Institute of Medical Sciences, , Chaitanya Nagar, Amalapuram, India.
2Assistant Professor,Department of Pathology, Konaseema Institute of Medical Sciences, Chaitanya Nagar, Amalapuram, India.
3Assistant Professor,Department of Orthopaedics, Konaseema Institute of Medical Sciences, Chaitanya Nagar, Amalapuram, India.
4Professor, Department of Pathology, Konaseema Institute of Medical Sciences, Chaitanya Nagar, Amalapuram, India.
5Senior Resident, Department of Orthopaedics, Konaseema Institute of Medical Sciences, Chaitanya Nagar, Amalapuram, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. S. Durgaprasad Hegde, Senior Resident, Department of Orthopaedics, Konaseema Institute of Medical Sciences, Chaitanya Nagar, Amalapuram, India.
Phone: 9705507384,
E-mail: dr_sdhegde@rediffmail.com
Alkaptonuria or Ochronosis is an autosomal recessive congenital metabolic error due to absence of enzyme homogentisic acid oxidase. Recently, we had an opportunity to diagnose this condition in one of our patients. An old aged man developed a pathological fracture of femur after a trivial fall at home. He was diagnosed to have intracapsular fracture neck of femur. Intraoperatively we noticed blackish discoloration of femoral head which lead us to investigate the case for alkaptonuria. Hemiarthroplasty was done with Austin moore prosthesis. Patient had cutaneous pigmentation and gross arthritic changes at multiple joints including spine. After one and half year patient developed a periprosthetic fracture of the femur for which open reduction and internal fixation was done. A periprosthetic fracture in ochronotic patient has never been reported till date which makes it a rarer entity. This article presents the clinico-radiologic manifestations of the case with surgical management and a follow up of two years.
Ochronosis, Homogentisic oxidase, Pathological fracture, Austin Moore prosthesis
Case Report
A 75-year-old male came with complaints of pain in left hip and unable to bear weight on that side after he had a trivial fall at home. On Roentgen examination he was diagnosed to have intracapsular fracture neck of left femur. Hemiarthroplasty was done with Austin Moore prosthesis. After surgery patient was made ambulatory on second day. Patient was put on regular physiotherapy to maintain normal range of motion. Intraoperatively there was thickened capsule; erosion of overlying cartilage was noted with blackish discoloration of femoral head.
After one and a half year, again he had a trivial fall in his bathroom. Immediately there was swelling in mid thigh and he was unable to bear weight. Radiographs showed periprosthetic fracture in left femur and it was fixed with dynamic compression plate [Table/Fig-1]. Post-operatively non weight bearing mobilization was started after two weeks, partial weight bearing at 6 weeks. He was started with calcium supplements, vitamin D and alendronate therapy. Patient was put on regular physiotherapy to maintain the range of movements in major joints as well as reduce muscle wasting. Patient started full weight bearing at 5 months after radiological union.
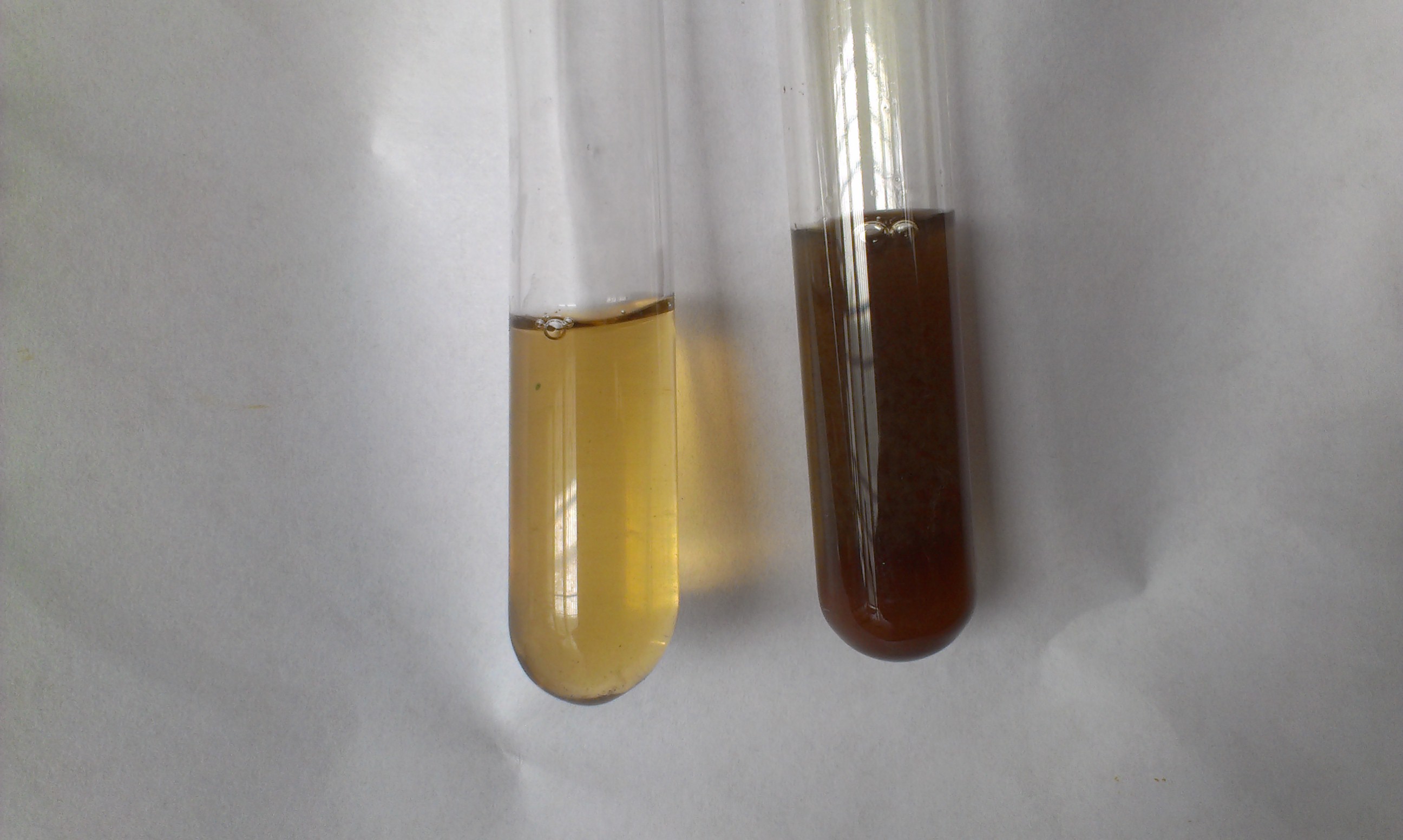
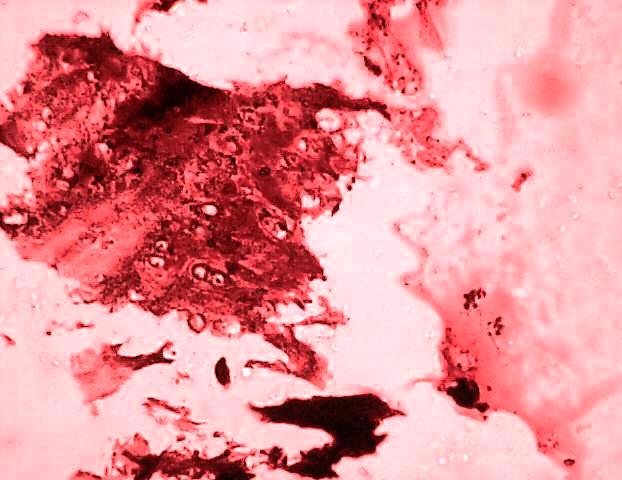
Clinical examination showed bluish black discoloration of skin of hands, nail beds, sclera and ear lobes [Table/Fig-2]. The pinnae were bony hard on palpation. Biopsy of ear cartilage revealed visualization of black pigment deposition [Table/Fig-3]. Urine turned black on long standing [Table/Fig-4]. A diagnostic reaction of dark brownish discoloration on addition of drop of dilute ferric chloride solution to urine was produced. Benedicts test was positive. Rheumatoid factor and HLA-B27 were negative. Renal function tests were within normal range. Histopathological examination showed black pigment deposition in cartilage [Table/Fig-5].
Radiological examination of spine showed osteoporosis, gross narrowing of disc spaces, and calcification of intervertebral disc in dorsolumbar region [Table/Fig-6]. Cervical spine showed reduction in intervertebral disc space and limitation of neck movements. Osteoarthritic changes were seen in both the hips, knees and shoulder joints. He had flexion deformity of both knee joints and marked limitation of movements. Range of motion in both shoulders platewas also reduced and more painful on the right side. The joints of the hands and feet were not affected.
Discussion
The term alkaptonuria was first used in 1859 by Boedeker to describe urine discoloration due to a reducing compound.
In ochronosis, breakdown of Homogentisic acid (HGA) is not possible; it forms a polymer which is deposited in the body tissues. A part of HGA is excreted in urine and sweat. Thus urine of such patients turns dark on standing or when alkalinized, owing to the oxidation of homogentisic acid [1] . In our case, patient was not aware of urine turning black on long standing, until we diagnosed.
Cutaneous manifestations are one of the earliest manifestations and alerting feature by which patient may be subjected to further investigation for diagnosis of ochronosis. But in this case intraoperative blackish discoloration of femoral head with thick capsule lead us to investigate the case for ochronosis. In our patient there was bluish black pigmentation of palmar surface of bilateral hands, nail beds, sclera and ear lobes. The pinnae were hard on palpation due to pigment deposition.
Intraoperatively we had great difficulty in delivering out femoral head. We were unable to cut the capsule with surgical knife due to thickening and a saw blade had to be used. The patient’s family history was unremarkable for genetic disorders, including alkaptonuria. His parents were not consanguineous.
The clinical manifestations are caused by the accumulation of HGA in the fibrillary collagens of connective tissues to which it binds irreversibly by polymerization and oxidation [2] Our patient used to get bilateral knee pain with morning stiffness after 60 years and was discstreated symptomatically with analgesics without any roentogenic screening and was missed in earlier examination by different clinicians. He noticed gradual decrease in knee and shoulder movements and developed mild fixed flexion deformity of bilateral knees. Radiographs of the shoulders and knees disclosed marked narrowing of the joint space with subchondral sclerosis.
To our knowledge, the case we present here is the first report of low trauma periprosthetic femur fracture in an ochronotic patient. While degenerative changes of the spine and major joints have been frequently reported, there are only few reports of femoral neck fractures and in some, spine fractures. Since it was very osteoporotic bone, locking compression plate would have been ideal implant but due to financial constraints, dynamic compression plate was used.
Spine is usually the first area to be affected, with patients complaining of stiffness and low back pain. The spine and major weight-bearing joints are most commonly affected and symptoms usually start by the fourth decade[3,4] . Our patient presented with low backache and stiffness at a later stage after large weight bearing joints were affected which is quite uncommon. In ochronotic spondylosis, although the entire is spine is affected, symptoms are mainly related to the lumbar region. Our patient had flattening of the lumbar lordosis, decreased movements, narrowing of the disc spaces with calcification of the cartilage and intervertebral discs.
In one ochronotic patient fracture neck of femur was treated by excision arthroplasty [5] whereas most of them were treated by total joint arthroplasty [6] . There was a case in which patient of 63 years had a stress fracture of left femoral neck in which surgical repair was done with pinning without any complications [7] .Severe joint arthritis is the indication for joint arthroplasty in ochronotic patients. Though our patient had arthritic changes in opposite hip as well as both knees, arthroplasty was not done due to financial constraints. In a series of 58 ochronotic patients, 8 (13.8%) had three or more joints replaced [8] .
One of differential diagnosis is ankylosing spondylitis where there are syndesmophytes, annular ossification and the bamboo sign which were absent in this case. Our patient lacked rheumatoid factor and the HLA-B27 antigen. In contrast to rheumatoid arthritis, the small joints of the hands and feet are usually not affected.
It has been suggested that clinical manifestations of alkaptonuric ochronosis are usually delayed, not appearing until the fourth decade of life because with ageing the renal clearance of homogentisic acid decreases. However, there were no signs of renal impairment in our patient.
Renal calculi, biliary calculi and cardiac failure secondary to valve calcification may occur. In our case there was absence of cardiac, renal or ocular complications and these were ruled out by relevant investigations.
In the respiratory system, dyspnea can develop owing to limited chest excursion as a result of stiffening of cartilage in the chest wall. Our subject had normal range of chest excursion without any symptoms nor any anaesthetic complications. Usually the disorder does not affect life span. After receiving alendronate therapy for two years after the periprosthetic fracture there was improvement in bone mineral density. It now seems practical that adequate antiresorptive therapy to prevent bone fractures in ochronotic patients should be considered much earlier in the course of treatment.
Our patient has been followed for 2 years post-periprosthetic fracture with good radiological union with regular exercises, antiresorptive therapy and he is able to carry out his activities of daily living with walking aid now at the age of 79.
X-ray showing (a) periprosthetic fracture of left femur with Austin moore prosthesis and (b) postoperative fixation with Dynamic Compression platewas

Photograph of eye showing ochronotic pigmentation in sclera

Photograph of ear showing black pigment deposition in cartilage with bony hard pinna

Photograph showing urine specimen immediately on voiding (left) and conversion to brownish black color on long standing (right)
Photomicrograph showing brownish black pigment deposition in cartilage. (Haematoxylin and eosin stained magnification 400 X)
X-ray lateral view of lumbar spine showing osteoporosis, gross narrowing of disc spaces, and calcification of intervertebral discs

Conclusion
Early diagnosis to prevent contracture, timely treatment of fractures and antiresorptive therapy to prevent fractures is absolute necessary to prevent further disability. Physicians and surgeons should be aware of multiple system involvement in this disorder, as early recognition and appropriate treatment may significantly improve the quality of life in these patients.
[1]. J Cervenansky, S Sitaji, T Urbanek, Alkaptonuria and ochronosis.J Bone Joint Surg Am 1959 41:1169-77. [Google Scholar]
[2]. E Emel, F Karagoz, IH Aydin, S Hacisalihoglu, MH Seyithanoglu, Alkaptonuria with lumbar disc herniation: a report of two cases.Spine 2000 25:2141-4. [Google Scholar]
[3]. S Aydogdu, E Cullu, MG Ozsoy, H Sur, Cementless total knee arthroplasty in ochronotic arthropathy: a case report with four-year follow-up.J Arthroplasty 200 15:539-43. [Google Scholar]
[4]. DM Carrier, CM Harris, Bilateral hip and bilateral knee arthroplasties in a patient with ochronotic arthropathy. Orthop Rev. 1990 19:1005-9. [Google Scholar]
[5]. B Zacharia, J Golan, Ramakrishnan V., Krishnankutty R. M., Veluthedath R., Puthezhath K., al et, Black hip, fracture neck of femur and scoliosis:A case of ochronosis.Journal of Inherited Metabolic Disease. 2009 32:215-20. [Google Scholar]
[6]. Siavashi Babak, Zehtab Mohammad J, Pendar Ehsan, Ochronosis of hip joint; a case report.Cases J. 2009 2:9337 [Google Scholar]
[7]. E Collins, R Hand, Alkaptonuric ochronosis: a case report.AANA J 2007 73(1):41-6. [Google Scholar]
[8]. C Phornphutkul, WJ Introne, MB Perry, I Bernardini, MD Murphey, Dl Fitzpatrick, al et, Natural history of alkaptonuria. N Engl J Med. 2002 347:2111-21. [Google Scholar]