Cow’s Milk Protein Allergy Mimicking Acrodermatitis Enteropathica
John Solomon1, Rugmini Kamalammal2, Mohammed Yaseen Sait3, Harita Lohith3
1 Professor and Head, Department of Paediatrics, Sree Balaji Medical College and Hospital (Bharath University), Chromepet, Chennai, India.
2 Associate Professor, Department of Paediatrics, Sree Balaji Medical College and Hospital, (Bharath University), Chromepet, Chennai, India.
3 Postgraduate Student, Department of Paediatrics, Sree Balaji Medical College and Hospital, (Bharath University), Chromepet, Chennai, India.
4 Postgraduate Student, Department of Paediatrics, Sree Balaji Medical College and Hospital, (Bharath University), Chromepet, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. John Solomon, Professor of Paediatrics, Paediatric Haematology and Oncology and Head of the Department of Paediatrics, Sree Balaji Medical College and Hospital, Chennai-600044, India.
Phone: +91 9444610092,
E-mail: pjohnsolomon@yahoo.co.in
Cow’s milk protein allergy is an adverse immune reaction to one or more of the constituent proteins of milk obtained from any animal, most commonly alpha s 1-casein cow’s milk. In many cases, the allergy is genetic in origin. The infants may experience symptoms within minutes after feeding (rapid onset) or commonly after 7-10 days of consuming the cow’s milk (slower onset). Many children with cow’s milk protein allergy develop symptoms in at least two of the following organ systems: gastrointestinal, skin and respiratory tract. Acrodermatitis Enteropathica (primary or secondary zinc deficiency) can also produce lesions in the skin and also gastro intestinal symptoms which can mimic milk protein allergy and differentiating between these two may be difficult. We are reporting a case of cow’s milk protein allergy in an infant, which was initially diagnosed as Acrodermatitis Enteropathica and treated with zinc. The lesions did not subside completely even after achieving adequate zinc levels, but on stopping the cow’s milk all the symptoms and signs disappeared completely and there was no recurrence on long term follow up.
Cow’s milk protein allergy, Acrodermatitis enteropathica
Case Report
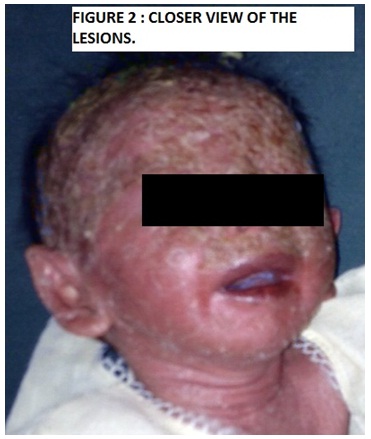
A 5-month-old boy was brought to us with a history of diarrhoea of 4 days duration and generalized skin rash. On examination, the patient was found to have erythematous plaques and scaly lesions which were more prominently seen over the face, especially in the periorbital and periorificial areas, buttocks, thighs, legs, arms, back of hands and feet. The hair on the eyebrows had fallen. Scalp hair was thin and fragile. The baby was delivered in a teaching hospital. Its birth weight was 2.5kg. The skin lesions had started in the early newborn period itself on introduction of cow’s milk and they had not subsided with many medications which had been tried in that institution. Hence, they brought the child to our institution. On admission, his weight was 1.75kg (below 3rd percentile) and his length was 58cm (below 5th percentile), thus showing evidence of failure to thrive. His systemic examinations showed a normal picture. Laboratory investigations showed normal complete blood count and the serum albumin was 3.4 mg %. We made a diagnosis of Acrodermatitis Enteropathica due to zinc deficiency. The serum zinc level was 54 micro g/dl (normal 60 – 120 micro g/dl). The serum Ig E was 540 IU (normal value is below 120 IU by chemiluminescence method). We treated the child with zinc 20mg/day (therapeutic dose). In addition, emollients and topical antibiotics were given. Even though some improvement was seen in the beginning, it was not complete and the rashes recurred 2 times in a florid manner, even while the child was on zinc treatment. Repeated studies done on zinc level estimates showed normal levels at the time of recurrence of symptoms. Considering the recurrences of skin lesions and diarrhoea and elevated serum IgE levels, inspite of normal zinc levels, cow’s milk protein allergy was suspected. Hence, cow’s milk was completely stopped and the baby was put on a soy based formula and a cereal based diet which gave adequate calories. All the lesions subsided and diarrhoea stopped and they have not recurred so far. At 8 months of age, he weighed 6kg [Table/Fig-1,2].
Generalised skin lesion, more on the face

Closer view of the lesions showing scalp and face
Discussion
Cow’s milk protein Allergy (CMPA), is seen in 2-7.5% of infants globally and the amount of milk which is required to elicit an immediate reaction can be as low as one drop [1]. CMPA usually appears within the first few months of life, often within days or weeks after the introduction of a cow’s milk based formula into the diet. Symptoms may also occur with exclusive breast feeding, if the mother ingests cow’s milk [1].
The slower onset reaction is more common. Symptoms may include gastrointestinal symptoms like vomiting, abdominal pain, diarrhoea, and occasional bloody stools. Respiratory symptoms are rare, but nasal pruritus and congestion, rhinorrhoea, and sneezing occur in some cases. Most of the children will outgrow this type of reaction after 2 years of age and some of them may outgrow it after adolescence. Rapid onset reactions come on suddenly, with symptoms like irritability, vomiting, wheezing, urticaria, itchy bumps on the skin and bloody diarrhoea. Severe allergic reactions (anaphylaxis) can occur in some cases. The risk of atopy increases if a parent or sibling has atopic disease (20-40% and 25-35% respectively) and it is higher still if both parents are atopic (40-60%). In our case, there was no history of atopy in the family [1,2].
In most of the cases, the condition is IgE-mediated and manifestation is usually atopic eczema, allergic rhinitis or Asthma. In our case cow’s protein allergy was confirmed by observing the elevated Serum Ig E levels and the resolution of the lesions on stopping cow’s milk. The possibility of rashes being caused by zinc deficiency alone was not considered, as third recurrence of lesions occured inspite of the normal zinc levels at that period of time. The low zinc levels initially may have been caused by chronic diarrhoea which may have led to secondary zinc deficiency. Undiagnosed food allergy can also lead to mild zinc deficiency and the presentation can be dermatitis, diarrhoea and increase in Serum Ig E levels [3].
The message is that zinc deficiency and cow’s milk protein allergy can give rise to same kind of symptoms and signs and that a differentiation between them is possible only on excluding cow’s milk from the diet. Reintroduction of cow’s milk may bring back the symptoms and signs, but it may sometimes be dangerous Alternative diets which have been suggested are an extensively hydrolyzed formula (eHF), amino acid formula or partially hydrolysed formula based on rice protein which were not used here due to non availability [1].
[1]. Vandenplas Y, Brueton M, Dupont C, Hill D, Isolauri Erika, Koletzko Sibylle, Guidelines for the diagnosis and management of cow’s milk protein allergy in infantsArch Dis Child 2007 92:902-8. [Google Scholar]
[2]. Fiocchi A, Brozek J, Schunemann H, Bahna SL, von BA, Beyer K, World Allergy organization (WAO) diagnosis and rationale for action against Cow’s milk allergy (DRACMA) guidelinesWorld Allergy Organ J 2010 3(4):57-161. [Google Scholar]
[3]. Martin Diana P, Tangsinmankong Nutthapong, Sleasman John W, Day-Good Noorbibi K, Wongchantara Danita R, Acrodermatitis enteropathica-like eruption and food allergyAnnals of Allergy, Asthma and Immunology 2005 94(3):398-401. [Google Scholar]