Cerebral Stroke After Valvular Surgery in Young Patients: Case Studies
Ravi Ghatanatti1, Sundeep Sanjivan Tirkey2, Anita Teli3
1Senior Resident, Department of Cardiothoracic Vascular Surgery, Vascular Surgery, SSKM Hospital and IPGME&R, Kolkata, India.
2Senior Resident, Department of Cardiothoracic Vascular Surgery, Vascular Surgery, SSKM Hospital and IPGME&R, Kolkata, India.
3Assistant Professor, Department of Physiology, SSKM Hospital and IPGME&R Kolkata, Kolkata, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ravi Ghatanatti, Duke Appartment, Bhowanipur, Kolkata-26, India.
E-mail: drravighatnatti@rediffmail.com
Intracranial haemorrhage (ICH) is a dreaded complication caused by oral anticoagulants (OAC) after valvular heart surgeries. Anticoagulant use in conventional doses increases the risk of ICH 7-10 fold. Intracerebral haematomas constitute 70% of the anticoagulant-related intracranial haemorrhages, with mortalities approaching 60%. Predisposing factors for anticoagulant-related ICH in Indian patients are unique as compared to those seen in their western counterparts. In anticoagulated patients, ICH evolves rapidly within hours; hence, emergency reversal of anticoagulation is crucial. We are reporting four cases of cerebral strokes which followed valvular surgeries in our institution, who were admitted during August 2012 to July 2013. There is an increasing need to educate the patients and update the physicians regarding the various issues which are involved in anticoagulation management.
Oral anticoagulants, Intracranial haemorrhage, Cardiac surgery
Case Report
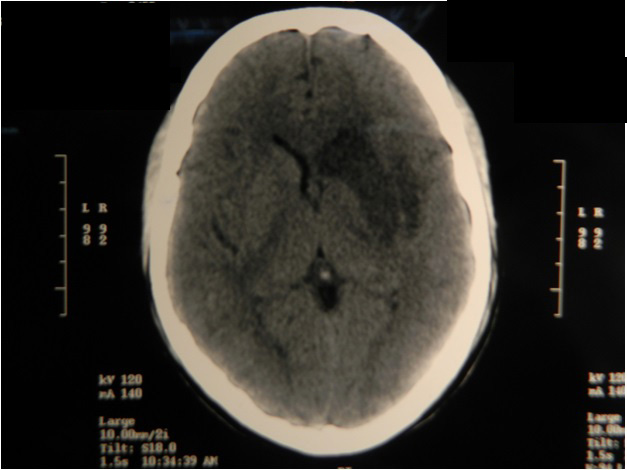
Case Vignette 1: Presented to emergency clinic with a history of fever, loose motions and altered sensorium. Prothrombin time/ INR and CT of brain were done. Findings shown in [Table/Fig-1]. Inj. Vit amin K administered and fresh frozen plasma infused. Patient deteriorated rapidly in the next 6-8 hours due to ongoing ICH, with Glasgow coma scale 3/15 and died after 72 hours.
Case Vignette 2: Brought in a state of altered sensorium with focal neurological deficites. Patient was diagnosed with ICH based on findings of CT of brain. Patient was intubated and fresh frozen plasma was infused with Vit K supplementation. Patient succumbed on the 5th day of admission.
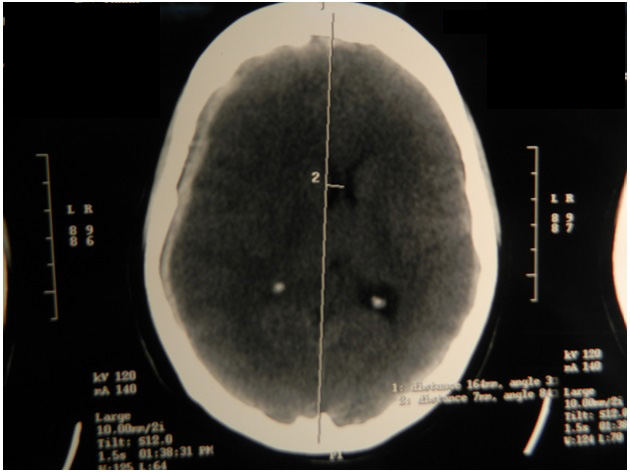
Case Vignette 3: Young male patient underwent double valve replacement for rheumatic valve disease. Patient developed fever and right sided paraplegia postoperatively. Blood culture and echocardiography were done and endocarditis was ruled out. On evaluation, INR was 1.44 and CT of brain showed an infarct involving left basal ganglia [Table/Fig-2]. During recovery phase, antiplatelets and heparin therapy was started, target INR was achieved with OAC titration dose.
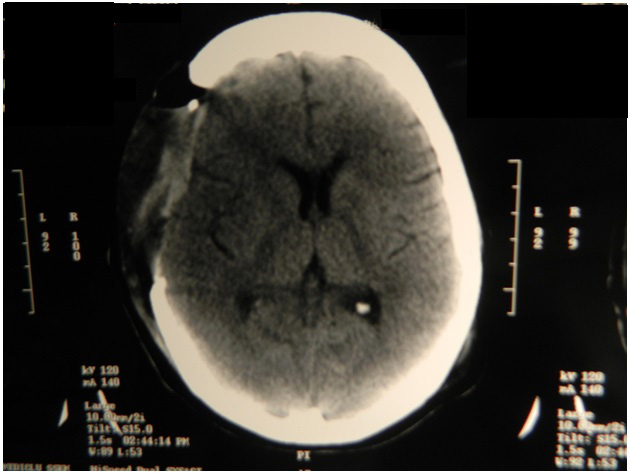
Case Vignette 4: Presented with right sided, subdural haematoma with a midline shift [Table/Fig-3] INR was 7.2. Oral anticoagulants were withheld and patient was treated with inj Vitamin K and fresh frozen plasma. Patient underwent decompressive craniotomy with evacuation of subdural haematoma on 3rd day of admission. Follow-up image was taken later [Table/Fig-4]. Patient recovered without any residual deficits.
[Table/Fig-1] depicts four cases of anticoagulation related ICH following valvular heart surgeries and their outcomes.
Patient profile, ICH and outcome VR: Mitral valve replacement, DVR: Double valve replacement
| SI. No | Age(years) | Sex | Surgery | Valve Type | Duration/event | INR | CT finding | Outcome |
| Case 1 | 17 | F | MVR | Tilting disk | 6 months | 8 | Intracerebral hematoma | Expired |
| Case 2 | 24 | F | MVR | Tilting disk | 12 months | 6 | Right extradural hematoma with intraventricular hemorrhage | Expired |
| Case 3 | 30 | M | DVR | Tilting disk | 2 weeks | 1.44 | Left hemispheric infarct | Revived |
| Case 4 | 38 | F | DVR | Bileaflet | 6 months | 7.2 | Right subdural hemorrhage | Revived |
Showing infarction in the region of left basal ganglia
Showing Right sided subdural hemorrhage with midline shift to left
Post- operative image after decompressive craniotomy and evacuation of Subdural Hematoma
Discussion
We performed 134 valvular surgeries during August-2012 to July-2013, out of which three patients presented with ICH and one patient with thromboembolic stroke. All cases were evaluated with CT scan of brain and prothrombin time/INR. Two patients succumbed and two patients were revived. The estimated mortality and morbidity rates were 0.2 and 2.2 episodes per 100 patient-years respectively. Inspite of anticoagulant therapy, the incidence of thromboembolic complications with the best mechanical prosthesis is still about 0.2 fatal complications and 1.0-2.0 nonfatal complications per hundred patient-years in aortic position. It increases to 2-3 nonfatal complications for mitral valve [1] .
ICH is a known and dreaded neurological complication of OACs [2] . Coumadin, followed by acenocoumarol, are the most commonly used oral anticoagulants in India. Indians are more prone for warfarin-food interactions as compared to western population. Diets which are rich in Vitamin K (cabbage, cauliflower, spinach, etc,) are typically consumed, which decreases INR. Indians consume over the counter medications (NSAIDs) or herbal products/foods (e.g., garlic, fenugreek) for various disorders. Data from Chinese and Japanese studies suggest that Asians may require lower INR for protection from thromboembolism and that they may be at an increased risk of bleeding at lower INR[3,4] . Many patients omit OAC during concurrent illnesses like fever and diarrhoea and come with low INR or they take antibiotics like metronidazole or macrolides more commonly and come with high INR/bleeding. Smoking addiction potentially lowers the INR. In the present study, 4 out of 134 patients who suffered OACs related strokes were in the age group of 17-38 years, which was in contrast to findings of a study done by Landefeld CS, where the incidence of stroke was more common in elderly patients[2] .
All the four cases in this study had inadequate outpatient based anticoagulant monitoring. Kakkar and collegues also showed that outpatient anticoagulant control was generally poor, with inadequate pretherapeutic assessment, an unacceptably high proportion of subtherapeutic PT/INR values and high complication rates [5] .
Diseased valve replacement was done with mechanical prosthetic valves in this study and OACs were administered, which increased the risk of stroke, as has been shown in other studies. Praveen et al found that the morbidity was increased in patients who were using mechanical heart valves on OACs and that inadequate anticoagulation was associated with an increased risk of stroke [6] .
In patients with ICH, apart from emergency neurosurgical interventions, rapid correction of INR has to be undertaken. Warfarin therapy has to be withheld and inj. Vitamin K 10 mg, which is diluted in D5W or NS, has to be administered by slow IV infusion over 30mins and this has to be repeated every 12 hourly, if needed [6] .
Anticoagulants can safely be withheld for short periods of upto 1-2 weeks in patients with ICH, who are on OAC and they can safely be reinstituted as early as 3 days with heparin and 7 days with OAC, without a major risk of rebleeding [7] .
Hence, we conclude that compliance and dietary patterns need to be kept in mind while prescribing OACs in India and for Indians who live abroad. For better patient compliance and to achieve target INR values as per the ACCP guidelines 2008 for OAC [8] , there is an acute need for better patient education and physician update of the above issues which are involved.
[1]. CM Otto, RO Bonow, Valvular heart disease. Bonow RO, Mann DL, Zipes DP, Libby P. (Eds) In: Braunwald’s Heart Disease Text of Cardiovascular Medicine 2011 9th EditionElsevier India Private Limited:1523 [Google Scholar]
[2]. CS Landefeld, L Goldman, Major bleeding in outpatients treated with warfarin: incidence and prediction by factors known at the start of outpatient therapyAm J Med 1989 87:144-52. [Google Scholar]
[3]. JH You, FW Chan, RS Wong, Is INR between 2.0 and 3.0 the optimal level for Chinese patients on warfarin therapy for moderate-intensity anticoagulation?Br J Clin Pharmacol. 2005 59:582-7. [Google Scholar]
[4]. S Suzuki, T Yamashita, T Kato, Incidence of major bleeding complication of warfarin therapy in Japanese patients with atrial fibrillationCirc J. 2007 71:761-5. [Google Scholar]
[5]. N Kakkar, R Kaur, M John, Outpatient oral anticoagulant management: an audit of 82 patients.JAPI 2005 53:847-52. [Google Scholar]
[6]. SV Praveen, V Sankar, M Fassaludeen, Predictors of morbidity in mechanical prosthetic heart valvesIndian Heart J. 2005 57(464) [Google Scholar]
[7]. D Chandra, A Gupta, V Grover, VK Gupta, When should you restart anticoagulation in patients who suffer an intracranial bleed who also have a prosthetic valve?Interact Cardiovasc Thorac Surg 2013 16:520-23. [Google Scholar]
[8]. SM Bates, IA Greer, I Pabinger, Venous thromboembolism, thrombophilia, antithrombotic therapy, and pregnancy: American College of Chest Physicians Evidence-Base Clinical Practice GuidelinesChest. 2008 1338th Edition:844S-886S. [Google Scholar]