This is a case report of spinal tuberculosis which could not be diagnosed in the early stages. Individuals who work in hospital settings and suffer from psychological stress need to be aware of the various hospital acquired infections and consequences of late diagnoses. A CT scan is indicated to rule out the spinal involvement, at the beginning of a severe backache, which does not respond to painkillers, rest, and if X-ray is normal. It is of immense help and much of the problems like paraplegia and morbidity which are associated with this kind of extra - pulmonary tuberculosis, could be avoided. Once paraplegia sets in, the response to treatment as well as the recovery are slow. The cost of CT Scan or MRI (Magnetic Resonance Imaging), no doubt, is very high, which ranges from Rs.4,500/- to Rs.5,000/- for an average Indian, but which goes a long way in reducing the debilitating conditions, excruciating pain and confinement to bed which occur during the spinal tuberculosis. Prolonged follow-up is essential in cases of Pott’s disease, as it was in the presented case. A strict treatment schedule of 18 months, combined with good nutritional support and bed rest, with spinal braces, is adequate for recovery from immobility and paraplegia caused by an advanced stage of spinal infection. This case therefore, supports an approach of nonoperative treatment over surgery, where the patient had progressive paralysis.
Case Report
Consent : A written informed consent was obtained from the patient for publication of this case report and the accompanying images (X-ray and CT Scans).
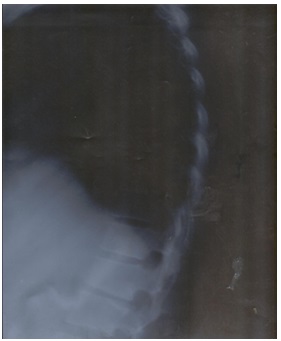
A 36-year-old female patient who worked in a hospital had a brief-history of fever and cough, which subsided after a standard one week therapy of antibiotics, amoxycillin, paracetamol, etc. but her cough persisted for more than 2 months. After few weeks, she felt pain in the ribs initially, which finally shifted to the back. She complained of writhing pain in the back, for which she was given pain killers and was advised rest. The pain disappeared after the use of pain-killer pills (250 mg), but they did not gave total relief. It persisted even after rest and in fact, it would become worse after a short nap or a night’s sleep. The difficulty in getting up after a night’s sleep affected her walking pace as well as her gait. There was low-grade fever in the evenings and a gradual weight loss, from 52 to 42 kgs. Doctors advised an X-ray of Chest A/P, Tubercular IgA and Mantoux test. X-ray was clear [Table/Fig-1] and both the other tests were negative. The complete blood picture was also normal. Even lateral X- ray of the lumbosacral spine did not reveal any of the lesions. X- ray of ribs, done to rule out fracture, even after 5 months of persistent pain, was normal. ASO titre was very high, about 600 IU and ESR was raised, which was 53mm. Penicillin injections were given, but they were of no use. At last, a CT scan (Computed Tomography Scan), a thorough scanning session with two dyes, plain and contrast enhanced, of DL spine revealed Carie’s Spine (Spinal Tuberculosis). Thin serial axial sections were taken from D9 to S1 with coronal and saggital reconstruction of images, which showed lytic areas of bone destruction in D9, D10, D11 and L2, L3, L5 vertebral bodies. Hypodense collections were seen in the pre - and para - vertebral spaces at D9 to D11 levels. Small amounts of collections with bony debris were seen to extend intraspinally at D11 level, which mildly compressed the thecal sac. The neural roots appeared to be normal but the disc height was reduced at D10 - D11 level [Table/Fig-2a,2b] . Culture of CT guided aspiration was positive for M.tuberculosis. Standard ATT (Anti-Tubercular Treatment, EHRZ) was started without delay. Streptomycin injections did not suit her and they resulted in trembling of her entire body, including the lips, with nausea and she could not stand. There was numbness in her feet and it felt like an electric shock when she stood or stepped down. Streptomycin injections were stopped immediately. But she was advised complete bed rest and was given a lumbosacral brace to be worn even while she slept . Multi-vitamin injections were given and a high protein diet was recommended. The condition was paraplegia and the lower part of her body was completely paralyzed. Grade III disability which resulted from weakness and gradual loss of sensation in the limbs were observed. However, there were no complications such as incontinence, i.e., sphincter mobility was unaffected. The acute pain reduced after one month, but spinal movements were restricted. On examination, even after 3 months, spinal movements were limited, with SLR of 80ºC both sides, power, Knee flexor - Grade III, knee extensor - grade III, grade IV, extensors - Grade III, ankle clonus +, plantar sensation which was upgraded with diminished sensation. After 5 months of initiation of treatment, she could move her toes, feet and could sit up straight, in the bed. After this, with a little effort, she could stand, with support, but the lower limbs trembled. The legs were too weak, as there was numbness. She could drag herself with difficulty and could resume her usual routine work, like going to the bathroom, etc. Meanwhile, there was severe itching all over her body and frequent vomiting. A liver function test revealed high SGPT/ALT, SGOT/ALT and high levels of cholesterol, triglycerides. There was a weight gain of 20 kgs. During this period, from 45 kgs to 65 kgs. After 6 months, she joined her duty at the hospital. The spinal condition slowed down the pace of walking as well as movement of any kind. Another CT Scan done at 6 months revealed healing of the scar. Intra-spinal extension was not seen, but small amount of granulation tissue was noted at D10 - D11 in the pre-vertebral space [Table/Fig-3] . Doctors advised her not to bend or lift weight, climb stairs, and/or drive. Treatment continued for 18 months, CT Scans were done after every 6 months [Table/Fig-4] and even after 18 months, when treatment was finally stopped. The last CT scan done of DL spine revealed that hypodense collections in the pre - and para - vertebral spaces at D9 to D11 levels had resolved and that no fresh lesion was seen [Table/Fig-5] .
Joint pains accompanied the weight gain, but RF test (Rheumatoid Factor) was negative. After this, light exercises, walking and low fat intake resulted in slight weight loss and they improved the general well-being of the patient.
Shows the X - Ray image at the initial stage of infection
Shows the CT Scan image at the initial stage of infection

Shows the CT Scan image at the initial stage of infection

Shows the CT Scan image after 6 months of infection / treatment

Shows the CT Scan image after 12 months of infection / treatment

Shows the CT Scan image after 18 months of infection / treatment

Discussion
Spinal TB, a chronic and slowly progressive disease with prolonged symptomatology, is a challenge to physicians. In recent years, there has been an increase in the numbers of spinal TB cases and we, therefore, want to report such a case of our patient who recovered from paraplegia. Pott’s disease results from an infection of the bone caused by the Mycobacterium tuberculosis bacteria via a combination of haematogenous root and lymphatic drainage. TB starts in the lung but it can travel to any organ or structure of the body. The spinal column is often the most affected extra-pulmonary site.
Patients with spinal TB have nonspecific symptoms that can cause a delay in the diagnosis [1,2] . Neural involvement may occur in up to 50% of patients, which can cause irreversible damage, if it is not promptly and adequately treated. The histories and conditions of the patients are important but they not always reliable for making an immediate diagnosis. Pain, the most common presenting symptom, usually has an insidious onset and it may be mechanical in nature during the initial stages. Persistent spinal pain, local tenderness, limitation of spinal mobility, febrile state and neurologic complications, including paralysis, present as the destruction continues. Other systemic symptoms are reflective of chronic illnesses including malaise, weight loss and fatigue [3,4] .
In Pott’s disease, the spinal cord may become involved due to compression by bony elements and/or expanding abscesses or by direct involvement of cord and leptomeninges caused by granulation tissue. Very often, the clinical presentation, together with the radiologic appearance of the spine and a positive tuberculin test, may suggest spinal TB, but the diagnosis must be confirmed by evidence of acid-fast bacilli from the bone or body fluids [5] . A high degree of suspicion is necessary to avoid delays that may result in neurologic deficit, irreversible damage and a high mortality rate. In the era of modern imaging modalities and effective anti-TB medication, spinal TB appears to be a disease which is too frequently forgotten by clinicians and under-emphasized by academicians. Misdiagnoses and delays are common. Several studies have reported that surgery is the mainstay of treatment and it is usually recommended for complications like paraplegia, loss of sensation, etc. which result from spinal tuberculosis, spinal tuberculoma, or abscesses, but we observed that a strict treatment schedule of 18 months, combined with good nutritional support, bed-rest and lumbosacral braces, while ambulant, were the mainstay of management, for complete recovery of patients with Grade III paraplegia. This case, therefore, supports an approach of non-operative treatment over surgery, where the patient had progressive paralysis.
In any patient who presents with a destructive lesion of the spine, CT or MRI of the spine may allow in making an early diagnosis and evaluation of Pott’s disease and para-vertebral and / or intra-spinal extension of the disease, while a biopsy is essential to confirm the diagnosis of TB, bacteriologically and histologically. Correlative CT and MRI have made diagnosis of spinal TB substantially easier and faster. Major advantage of these studies is their ability to show lytic lesions and adjacent abscess formations [6,7] . CT scan was the most useful radiological tool, both for making the diagnosis and for determining the extent of the disease. In our patient, CT scan revealed positive findings such as anterior vertebral body destruction, psoas or para-spinal abscesses. In the reported case, the patient improved without any neurologic deficits. Antituberculosis agents, the standard being a combination of Isoniazid, Rifampicin and Pyrazinamide, with or without Ethambutol, are essential for management, with chemotherapy, for at least 18 months, which are preferred to shorter courses [8] . Moreover, a prolonged follow-up is essential in case of Pott’s disease, as in the presented case. Patients with spinal TB who present withparaplegia and no deformity usually respond well to treatment[9,10] . Several authors have reported differential managementof cases with surgery and/or treatment. Butt et al., reviewed 60cases of spinal tuberculosis and concluded that any young female from a poor social background with backache and a positive familyhistory of tuberculosis should be examined and investigated fullyfor tuberculosis of spine and managed with appropriately selectedtreatment modality and compliance of the patient [11,12] .
Conclusion
We therefore feel that taking a careful history, doing an examination along with CT scan or MRI, be advised in patients who present with severe backache, which does not respond to painkillers and rest, to rule out a spinal involvement. An early treatment, if it is initiated, would help in further managing deterioration and complications which result from paraplegia. Anti-tuberculosis treatment, along with good nutritional support, bed rest and lumbosacral braces, while ambulant, are essential, for complete recovery of patients with grade III paraplegia.
Acknowledgements
I thank Dr. S. Husain and Dr. Harish Chandra for treating and following up the patient.
[1]. ES Nussbaum, GL Rockswold, TA Bergman, Spinal tuberculosis: a diagnostic and management challenge.J. Neurosurg 1995 83:243-47. [Google Scholar]
[2]. MS Moon, Tuberculosis of the spine. Controversies and a new challengeSpine 1997 22(15):1791-97. [Google Scholar]
[3]. SM Tuli, TP Srivastava, BP Varma, GP Sinha, Tuberculosis of the spine. Acta OrthopScand. 1967 38:445-58. [Google Scholar]
[4]. L Huelskamp, S Anderson, M Bernhardt, TB of the spine: Pott’s diseaseOrthop. Nurs 2000 19:31-35. [Google Scholar]
[5]. JP Janssens, R de Haller, Spinal tuberculosis in a developed country. A review of 26 cases with special emphasis on abscess and neurologic complications.Clin. Orthop. Rel. Res 1990 257:67-75. [Google Scholar]
[6]. HS Sharif, JL Morgan, MS Al Shaled, Role of CT and MR imaging in the management of tuberculosis spondylitis. Radiologic Clinics. ofNorth America. 1995 33:787-804. [Google Scholar]
[7]. DJ Shanley, Tuberculosis of the spine: imaging features.Am. J. Res 1995 164:659-64. [Google Scholar]
[8]. SM Tuli, Results of treatment of spinal tuberculosis by “Middle Path” RegimeJ Bone and Joint Surg 1975 57(B):13-23. [Google Scholar]
[9]. Halil Yanardag B Canbaz, ¼lent. Pott’s Disease: The Clinical Features And Treatment outcomes of eight patients of Spinal Tuberculosis. The InternetJ. Int. Med. 2004 :4-2. [Google Scholar]
[10]. NS Martin, Pott’s paraplegia. A report on 120 casesJ. Bone and Joint Surg. 1971 53(B):596-608. [Google Scholar]
[11]. AR Rezai, M Lee, PR Cooper, Modern management of spinal tuberculosisNeurosurgery. 1995 36:87-89. [Google Scholar]
[12]. MA Butt RM Bokhari, S Shams, Spinal Tuberculosis: easy to diagnose, difficult to manageProf. Med. J 1997 4(4):339-44. [Google Scholar]