Extraskeletal Chondroma (ESC) is uncommon which occurs predominantly in hands and feet. It has a variable histology, with two thirds of the ESCs showing mature hyaline cartilage which is arranged in distinct lobules with fibrosis, or ossification, or myxoid areas and few showing immature patterns, with chondroblasts mimicking extraskeletal myxoid chondrosarcomas (ESMCSs). ESCs can recur but they never metastasize, whereas ESMCSs can metastasize, which require aggressive treatment.
We are reporting a case of ESC which was located in the distal phalanx of right foot great toe in a 58-year-old male patient. The histopathology in our case showed features of ESC, with some foci showing myxoid stroma and few chondroblasts with atypical pleomorphic nuclei mimicking ESMCS. Hence, the case had to be carefully evaluated to exclude ESMCS and to make the diagnosis of ESC. The treatment was limited to simple excision of the tumour and extensive surgery and post operative radiotherapy were avoided.
Benign tumour, Mimics, Soft tissue
Case Report
A 58-year-old male presented to the Outpatients Department for a painless swelling of great toe of right foot, of six months duration. Physical examination revealed a well-defined, firm, fixed, swelling of 2x2 cms on the distal phalanx of great toe of right foot. X-ray of the mass showed a dense soft tissue mass, with no bone involvement. The same was excised and sent for a histopathological examination.
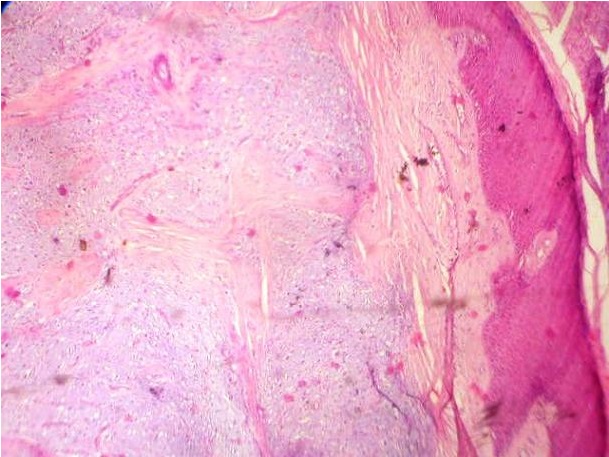
Gross examination revealed a well-defined mass of 2x2 cms. Cut section showed a firm, whitish tumour with gelatinous and chalky white areas of calcification, which were covered by a piece of skin on one side [Table/Fig-1] .
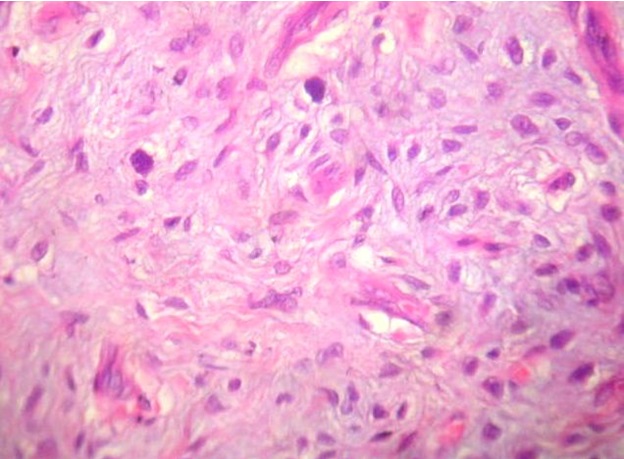
Microscopic examination showed structure of skin with a tumour in the dermis, which was arranged in lobules which were separated by fibrous septa [Table/Fig-2 , 3] . There were islands of mature hyaline cartilage, myxoid areas and foci of granular calcification. Some of the chondrocytes showed atypical nuclei [Table/Fig-3,4] . A histopathological diagnosis of an extraskeletal chondroma was made.
Well-defined nodule covered by skin on one side

Photomicrograph showing well-defined lesion with chondrocytes arranged in lobules separated by fibrovascular septa with myxoid areas (H and E, X 100)
Photomicrograph showing specks of calcification (H and E, X 400)
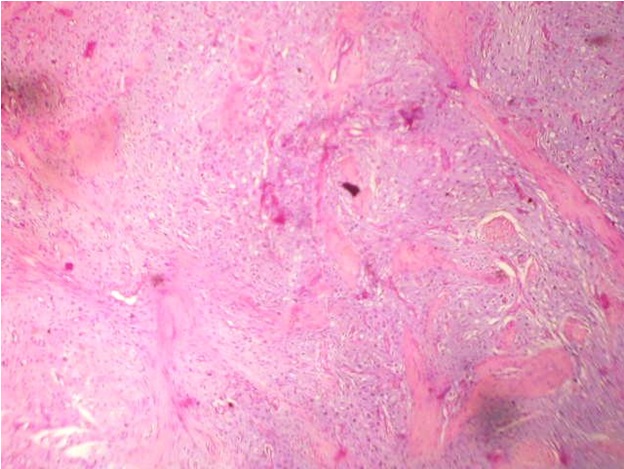
Photomicrograph showing well-defined lesion with chondrocytes arranged in lobules separated by fibrovascular septa with few chondrocytes showing large atypical nuclei (H and E, X 100)
Discussion
ESC- Soft tissue chondroma is a rare benign cartilaginous tumour and nearly 80% of ESCs are found in the fingers and the rest is seen in hands, feet, toes and trunk [1-5]. Few cases are reported at rare sites like dura, larynx, pharynx, oral cavity, skin, fallopian tube and parotid gland [6-12].
Anatomic distribution of soft tissue chondroma as seen in published studies has been shown in [Table/Fig-5] .
It usually arises as a slowly growing, painless mass in adults, with an age range of 30-60 years, with a slight male predominance, as in our case. It is solitary in nature and may occasionally involve multiple sites. It is often associated with tendons, tendon sheath and joint capsules [13,15]. Dahlin and Salvadore suggested a synovial origin [2]. Though it does not involve bones, it may leave compression deformities or bone erosions. Radiographically discrete, irregular, ring like, or curvilinear calcifications are often seen [13,14]. ESCs are well demarcated, firm, rounded small masses, which seldom exceed 3 cms in greatest diameter [1]. Histopathologically, they can be diverse, ranging from a mature form with hyaline cartilage which is arranged in distinct lobules with fibrosis, or ossification or with myxoid areas, to an immature pattern with a pre-ponderance of chondroblasts [1,13-15]. One thirds of them can display granular, floccular, or crystalline calcifications which can be focal or diffuse [1,13-15]. In our case, few chondrocytes showed atypical nuclei and focal calcifications were seen. [Table/Fig-3]. Occassional cases may even show granuloma formations [1,2,13,14] Like normal chondrocytes, the cells of ESC are positive for Vimentin and S100 protein.
ESCs have to be differentiated from benign conditions like calcifying aponeurotic fibroma (CAF), tumoural calcinosis (TC), giant cell tumour of the tendon sheath (GCT), synovial chondromatosis (SC) [1,3,13,14]. More importantly, ESCs with cellular pleomorphism and myxoid changes have to be specially differentiated from ESMCSs which are malignant tumours that can metastasize, which require extensive surgery and post-operative radiotherapy [1,3]. CAF occurs in young patients in hands rather than in the digits. Short bar like foci of cartilaginous metaplasia in a dense fibromatous background are seen in CAF.
TC may mimic a heavily calcified ESC. But it lacks cartilage and it has a distinct histiocytic response to calcified material.
GCT has a uniform cellular pattern and it rarely has metaplastic cartilage or bone.
Most importantly, ESCs have to be differentiated from ESMCSs. ESCs can be differentiated from ESMCSs, as in our case, by their smaller sizes, characteristic locations in extremities,Low cellularities, and the chondrocytes being better differentiated in the peripheral portions of the tumour. Foci of calcification and ossification are features which are commonly seen only in ESCs, in contrast to ESMCSs [1].
The potential problem with ECSs is that they can recur. In the fifty four cases seen by Dahlin and Salvador, there was recurrence in eight during an observation period of one year to ten years[2].
In the fifty six cases which Chung and Enzinger reported, in which follow up information was available for duration of 5.6 median years, ten patients had recurrence after initial excision[1]. Our patient, now, after a follow up of three years, is disease free without recurrence.
In summary, ESCs are a rare, benign, soft tissue tumours with a variable histologies. ESCs may mimic ESMCSs, frequently leading to a misdiagnosis and aggressive management. Hence, caution should be exercised, to arrive at a diagnosis of ESC, as complete excision of the tumour is the treatment of choice.
Anatomic distribution of soft tissue chondroma in published studies
| Published Studies | Upper Extremity n=131 | Lower Extremity | Head and Neck n=7 | Trunk n=2 | Skin n =1 | Fallopian Tube n=1 | Total Number of Cases n=193 |
| | Foot n=47 |
| Dahlin and Salvador [2] | 50 | 20 | 20 | | | | | 70 |
| Chung and enzinger [3] | 75 | 25 | 21 | 2 | 2 | | | 104 |
| Anthouli-Anagnostopoulou [4] | | | 1 | | | | | 1 |
| Delsignore et al., [] | 1 | | | | | | | 1 |
| Bergmann et al., [6] | | | | Dura-2 | | | | 2 |
| Lewis et al., [7] | | | | Larynx-1 | | | | 1 |
| Totios et al., [9] | | | | Gingiva -1 | | | | 1 |
| Ando et al., [10] | | | | | | 1 | | 1 |
| Kostopoulos et al., [11] | | | | Parotid gland-1 | | | | 1 |
| Han et al., [12] | | | | | | | 1 | 1 |
| Bansal et al., [13] | 1 | | 2 | | | | | 3 |
| Zlatskin et al., [14] | 4 | | 2 | | | | | 6 |
| Moosa Bahnassy [15] | | | 1 | | | | | 1 |
[1]. FM Enzinger, SW Weiss, Cartilaginous tumors and tumorlike lesions of soft tissue. In:Teratology 1977 8th EditionCV Mosby coSt. Louis:1017-38. [Google Scholar]
[2]. DC Dahlin, AH Salvador, Cartilaginous tumors of the soft tissues of the hands and feet.Mayo Clin Proc 1974 :49-721. [Google Scholar]
[3]. EB Chung, FM Enzinger, Chondroma of soft parts.Cancer 1978 :41-1414. [Google Scholar]
[4]. FA Anthouli-Anagnostopoulou, G Papachristou, Extraskeletal Extraskeletal, a rare soft tissue tumor. Case report.Acta Orthop Belg 2000 :66-402. [Google Scholar]
[5]. JL Delsignore, BA Torre, RJ Miller, Extraskeletal chondroma of the hand. Case report and review of the literature.Clin Orthop. 1990 :254-147. [Google Scholar]
[6]. M Bergmann, W Pinz, S Blasius, Chondroid tumors arising from the meninges – report of 2 cases and review of the literatureClin Neuropathol 2004 :23-149. [Google Scholar]
[7]. JE Lewis, KD Olsen, CY Inwards, Cartilaginous tumors of the larynx: clinicopathological review of 47 cases.Ann Otol Rhinol Laryngol 1997 :106-94. [Google Scholar]
[8]. DH Wang, XL Guan, LF Xiao, Soft tissue chondroma of the parapharyngeal space: a case treportJ Laryngol Otol 1998 :112-294. [Google Scholar]
[9]. K Tosios, G Laskaris, J Everson, Benign cartilaginous tumor of the gingiva . A case reportInt J Oral Maxillofac Surg 1993 :22-231. [Google Scholar]
[10]. K Ando, G Laskaris, J Everson, Cutaneous cartilaginous tumorDermatol Surg 1995 :21-239. [Google Scholar]
[11]. IS Kostopoulos, I Daniilidis, G Velegrakis, Chondroma of the parotid gland. Clinicalhistologic- immunohistochemical findings of a rare case.Laryngorhinootologie 1993 :72-261. [Google Scholar]
[12]. JY Han, HS Han, YB Kim, Extraskeletal chondroma of the fallopian tube. J Korean Med Sci. 2002 :17-276. [Google Scholar]
[13]. M Bansal, AB Goldman, EF Dicarlo, Soft tissue chondromas: diagnosis and differential diagnosisSkeletal Radiol 1993 :22-309. [Google Scholar]
[14]. MB Zlatskin, PH Lander, LR Begin, Soft tissue chondromasAJR 1985 144:1263-7. [Google Scholar]
[15]. Bahnassy Moosa, Khalik Hala Abdul, Soft tissue chondromas: A case Report and literature and reviewOMJ 2009 24:296-7. [Google Scholar]