Perforated GIST in Jejunum – A Rare Cause of Abdominal Cocoon
Usha M1, Vijay Kumar2, Rau Aarathi R3, Sulatha Kamath4
1Assistant Professor, Department of Pathology, M.S. Ramaiah Medical College, MSRIT Post, Bangalore, Karnataka, India.
2Professor, Department of Surgery, M.S. Ramaiah Medical College, MSRIT Post, Bangalore, Karnataka, India.
3Professor, Department of Pathology, M.S. Ramaiah Medical College, MSRIT Post, Bangalore, Karnataka, India.
4Professor, Department of Pathology, M.S. Ramaiah Medical College, MSRIT Post, Bangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Usha M, 150, 9th Cross, HIG Colony Bangalore- 560094, India.
Phone: 08971961860,
E-mail: usharavihitha@gmail.com
Gastrointestinal stromal tumours [GISTs] are rare but they commonly arise in stomach, and small or large intestines. They are usually accompanied with gastrointestinal bleeding. We are reporting a case of GIST which occurred in a 52-year-old male,who presented with acute abdomen. On laparotomy, the entire segment of jejunum was found to be partially encased in fibrocollagenous tissue, which formed a cocoon. Moreover, the intestine showed diffuse thickening with multiple tumour masses, which is an uncommon gross finding in GIST. This case report highlights variable clinical and morphological manifestations of GIST. Awareness on its rare clinical manifestations, including abdominal cocoon, may help in making an early diagnosis and providing timely appropriate treatment.
Abdominal cocoon, GIST, Multiple, Peritonitis
Case Report
A 52-year-old male was brought to casualty with complaint of pain in abdomen of two months duration. Pain was reported to aggravate since one day. On examination, diffuse abdominal tenderness with guarding and rigidity was seen. X- ray showed gas under the diaphragm and a provisional diagnosis of a hollow viscous perforation was considered. The patient was taken up for emergency exploratory laparotomy, which revealed faecal peritonitis, multiple perforations and abdominal cocooning of jejunum, with multiple nodules in the peritoneum. The entire segment of jejunum was resected along with peritoneal deposits and it was sent for histopathological examination.
Gross findings
The abdominal cocoon was composed of jejunum which was encased partially in fibrocollagenous membrane which measured 16x12.5x8cm. On opening, the cocoon revealed loops of intestine with exudation on the serosal surface and multiple perforations. Cut surface revealed diffuse thickening of the intestinal wall with multiple nodular gray white masses, [Table/Fig-1a] with the largest mass measuring 3.5 cm in diameter [Table/Fig-1b].
Microscopy
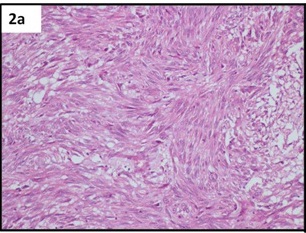
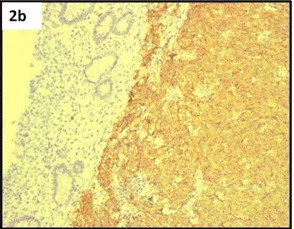
Microscopic examination revealed a spindle cell tumour, with tumour cells being arranged in interlacing fascicles, with large vesicular elongated nuclei [Table/Fig-2a]. Mitotic activity was high, with 10 mitoses per 50 high power fields. Also seen on the serosal surface was extensive fibrosis, with mixed inflammatory infiltrate. The peritoneal deposits revealed tumour with similar microscopic features. Immunohistochemistry was done by using markers, CD 117[c-kit], CD 34, S-100 and EMA. CD 117 [Table/Fig-2b] and CD 34 showed strong positivities and S-100 and EMA showed negativities. Final diagnosis of high-risk type GIST was declared, based on the mitotic index, tumour size, site and peritoneal deposits. The patient was referred to Oncology Department for further treatment and he was started on Imatinib Mesylate.
shows small intestine showing diffuse thickening with multiple nodular gray white masses

shows closer view of the largest mass

shows interlacing bundles of spindle shaped tumor cells (H and E; X100 )
shows tumor cells with strong positivity for CD 117 (c-kit)
Discussion
GISTs are rare stromal tumours representing 0.1-3% of all gastrointestinal tumours, which are thought to arise from the interstitial cells of Cajal or from the common intestinal mesenchymal precursor cells [1]. GISTs, in 95% of the cases, show c-kit mutation and about 5% cases show PDGFRA mutation.
C-kit positive cases respond well to treatment with ImatinibMesylate, which is a tyrosine kinase inhibitor.The most common site of occurrence of GISTs is stomach (60%), followed by small and large intestines (15%) and less commonly the omentum, mesentery and retroperitoneum [1]. Patients are typically over the age of 50 years. Clinical manifestations are highly variable and they depend on the location and size of the tumour. The common clinical presentations of GISTs are gastrointestinal bleeding (50%), abdominal pain (20-50%) and obstruction (20%) and approximately one third are detected incidentally [1]. Some rare clinical presentations include hypoglycaemia, abdominal pain caused by torsion of an exophytic tumour and GISTs which mimick acute appendicitis [1]. Our case presented with signs and symptoms of peritonitis caused by multiple perforations of jejunum and per-operatively, abdominal cocoon was seen. To the best of our knowledge, our case is the first one of GIST which presented as an abdominal cocoon. ‘Abdominal Cocoon’, also known as ‘sclerosing encapsulating peritonitis’ (SEP), is a rare condition which is characterized by the encasement of the small bowel by a fibrocollagenic cocoon like sac [2]. This condition was first observed by Owtschinnikow and it was called as peritonitis chronica fibrosa incapsulata [3]. Later, Foo et al., named this as an abdominal cocoon [4].
Primary and secondary types of abdominal cocoons have been described; the primary form is commoner, and it has been described in young adolescent females from the tropical and subtropical countries. The exact stimulus for the inflammatory reaction is not known. It has been suggested that it may arise from a subclinical primary viral peritonitis, as an immunological reaction to gynaecological infections, or from retrograde menstruation [2,5]. Secondary form has been reported in association with intake of drugs like practolol, propranolol and intraperitoneal instillation of drugs, chronic ambulatory peritoneal dialysis, ventriculoperitoneal and peritoneovenous shunts, sarcoidosis, systemic lupus erythematosus, cirrhosis, multiple leiomyomas of the uterus, endometriotic cysts or tumours of the ovary, recurrent peritonitis and abdominal tuberculosis [2,5]. An extensive literature search did not show any reported case of GIST which presented as an abdominal cocoon. Abdominal cocooning in this case could probably be explained by multiple perforations which had led to peritonitis, which was the stimulus for inflammatory reaction which had led to formation of fibrocollagenous membrane which had encased the intestine.
The gross appearance of the tumour, in this case, was unusual. GISTs most often present as solitary, well-circumscribed tumours in submucosa of the intestine. The surface epithelium shows ulceration, which is responsible for gastrointestinal bleeding. In our case, the intestine showed diffuse thickening caused by grey white tumour, with multiple grey white nodular masses. The largest nodule measured 3.5 cm in the greatest dimension. Even though the intestinal wall was thickened by the tumour, it was associated with multiple perforations. Multiple GISTs may be sporadic or familial. Familial form is associated with germline mutations of c-kit or it may be associated with Type 1 neurofibromatosis [6,7]. In our case, there were no clinical features or family history of Type 1 neurofibromatosis. Though there was no family history of GIST, germline mutations for c-kit could not be studied, to rule out the familial association.
In conclusion, we presented a case of jejunal GIST with a rare clinical presentation and gross appearance, thereby including GIST in the differential diagnosis of an abdominal cocoon. Recognition of the GIST at the time of emergency laparotomy is required, for doing a complete clean surgical resection, to prevent local recurrence.
[1]. SKP John, S Basu, RJ Lawrance, N Davies, An unusual presentation of a gastrointestinal stromaltumour (GIST)World J Surg Oncol. 2007 :5-78. [Google Scholar]
[2]. R Kaushik, RPS Punia, H Mohan, AK Attri, Tuberculous abdominal cocoon – a report of cases and review of the literature.World Journal of Emergency Surgery 2006 :1-18. [Google Scholar]
[3]. B Kirschtein, S Mizrahi, I Sinelnikov, L Lantsberg, Abdominal Cocoon as a Rare Cause of Small Bowel Obstruction in an Elderly Man: Report of a Case and Review of the Literature.Indian J Surg. 2011 73:73-75. [Google Scholar]
[4]. KT Foo, NgKC A Rauff, WC Foong, R Sinniah, Unusual small intestinal obstruction in adolescent girls: the abdominal cocoonBr J Surg 1978 65:427-30. [Google Scholar]
[5]. S Ranganathan, BJJ Abdullah, V Sivanesaratnam, Abdominal Cocoon SyndromeJ HK Coll Radiol 2003 6:201-03. [Google Scholar]
[6]. DY Kang, CK Park, JS Choi, SY Jin, HJ Kim, M Joo, Multiple gastrointestinal stromal tumors: Clinicopathologic and genetic analysis of 12 patientsAm J Surg Pathol. 2007 31:224-32. [Google Scholar]
[7]. HJ Kim, K Park, YJ Yuh, SJ Jang, J Choi, Multiple gastrointestinal stromal tumors with a germline c-kit mutation.Pathol Int 2005 55:655-59. [Google Scholar]