Sclerosing Peritonitis (SP) is characterized by fibrous thickening and adhesions of the peritoneum and it is encountered frequently in association with peritoneal dialysis, practolol and anticonvulsant therapy. Rarely does it present as a gynaecological complication, most commonly in conjunction with luteinized thecoma of ovary. Very rarely has sclerosing peritonitis been reported to occur with ovarian cystic teratoma and a luteinized variant of adult granulosa cell tumour, among which only one case has been reported in the English literature.
An 18-year-female presented with a history of lower abdominal pain, of one month’s duration. At surgery, an ovarian mass was noted, along with adhesion of bowel loops which were enclosed within a diffusely thickened peritoneal membrane, forming a cocoon. Adhesions were seen in bilateral paracolic gutter and infracolic omentum, which were suggestive of metastatic deposits.
Histopathology of ovarian lesion was interpreted as a juvenile granulosa cell tumour. The peritoneal process revealed sclerosing peritonitis.
We emphasize this rare association of sclerosing peritonitis with juvenile granulosa cell tumour and that the peritoneal process of sclerosing peritonitis in a juvenile granulosa cell tumour should not lead to over staging of an ovarian tumour.
Case Report
An 18-year-old female presented with lower abdominal pain of one month’s duration. She had fever, two days prior to her admission. There was no history of weight loss, loss of appetite or bleeding per vagina. Age of menarche was 14 years. Menstrual cycles were normal. General examination was normal.
Per-abdomen examination revealed diffuse distension, guarding and rigidity. Per-rectum showed fullness in the right fornix caused by a mass of size, 5 x 5 cm, which was felt in the right adnexae, which was hard and fixed. Uterus could not be felt separately.
Clinically, a diagnosis of a right tuboovarian mass with ascitis was made. Ultrasound and computed tomography suggested presence of a solid cystic mass in the right ovary. Exploratory laparotomy was performed.
Per-operative findings: Ascitis was noted along with a right ovarian tumour, the posterior wall of which was ruptured. Also seen were multiple grey white indurated nodules which were approximately one cm in diameter, over the peritoneal surface. Marked adhesions were seen in the bilateral paracolic gutter, pouch of Douglas, posterior wall of the uterus and the adjacent rectum. Hysterectomy with unilateral salpingooophorectomy, with sampling from the bilateral paracolic gutter, pouch of Douglas and peritoneal nodules was done.
Gross: Right ovary was replaced by a tumour which measured 12 x 9 x 7 cm. External surface was bosselated. Cut surface was solid grey, white to grey yellow, with areas of myxoid changes, fine cystic changes and haemorrhage. Tissue which was sampled from bilateral paracolic gutter and pouch of Douglas consisted of grey white to grey brown flap like tissue which measured 4.5 x 2.5 x 1.3 cm. Omentum consisted of fibro fatty tissue with tiny nodules, which were 0.5 cm across.
Endometrium and cervix were unremarkable.
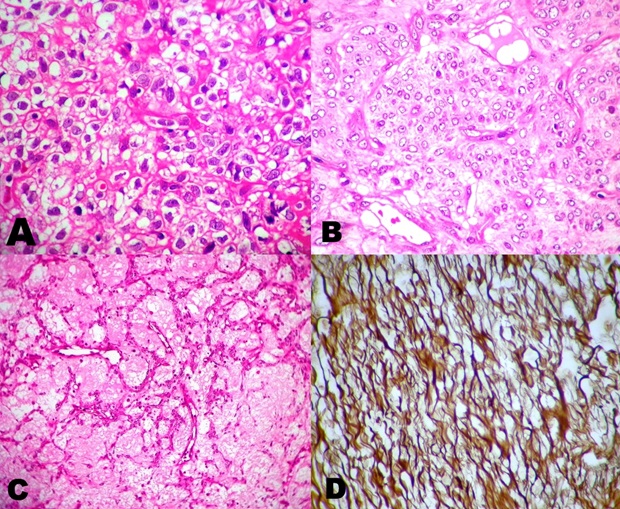
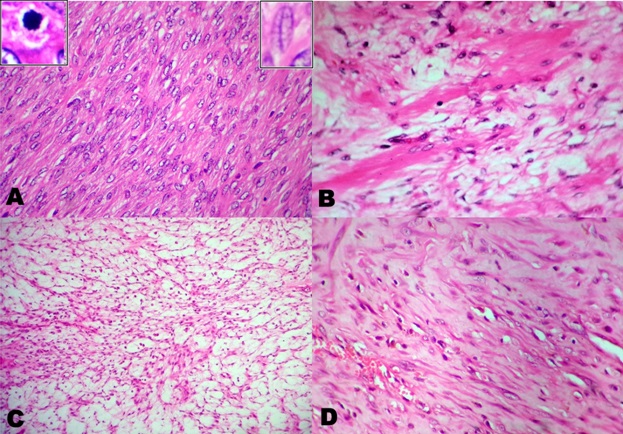
Microscopy: Sections from the tumour consisted predominantly of oval cells which were arranged in diffuse sheets, fascicles, interlacing bundles and in a vague storiform pattern. The individual cells were uniform, with moderate amount of eosinophilic cytoplasm, which were vacuolated at places, with nuclei which had angulated nuclear membranes, fine chromatin, prominent nucleoli and infrequent nuclear grooving. Admixed within these were clusters of round to polygonal cells with vacuolated cytoplasm. Brisk mitotic activity (20 to 30 / 10 HPF) was noted. Extensive areas of oedema, collagenization, myxoid changes, micro cyst formations, vague macro follicles, haemorrhage and foci of necrosis were noted. In silver impregnation staining, the reticulin fibres were found to surround the clusters of tumour cells [Table/Fig-1,2].
At immunohistochemistry, positivities for calretinin and inhibin were noted.
Sections from the posterior wall of the uterus, paracolic gutter, pararectal and omental tissue showed extensive fibroblastic proliferation, along with congested blood vessels and mixed inflammation [Table/Fig-2]. Ascitic fluid was negative for malignancy.
Hence, a final diagnosis of a juvenile granulosa cell tumour with sclerosing peritonitis was made.
Patient is doing well 24 months post-surgery.
A. Microphotograph from ovarian tumor showing polygonal cells with clear cytoplasm (Luteinization) Hematoxylin and Eosin (H & E) B. Microphotograph showing clusters of polygonal cells with pale eosinophilic cytoplasm (H&E 400) C. Microphotograph showing macro follicular pattern (H&E) D. Reticulin stain showing reticulin fibers surrounding nests of tumor cells (Reticulin)
A. Microphotograph from ovarian tumor showing spindle cells in fascicles (H&E)Inset left depicts mitosis. Inset right depicts nuclear grooving (H&E) B. Microphotograph from ovarian tumor shows interspersed collagen (H&E) C. Microphotograph from ovarian tumor showing edematous areas (H&E) D. Microphotograph from peritoneal nodules showing fibroblastic proliferation and blood vessels (H&E)
Discussion
Juvenile granulosa cell tumour of ovary (JGCT) is a rare subtype of granulosa cell tumour (GCT) and such tumours constitute 5 % of all GCTs [1]. Microscopically, it differs from adult GCT by infrequent presence of nuclear grooves, absence or rarity of typical call exner bodies, presence of macrofollicles and cells with extensive luteinization [2,3]. Sometimes, rarity of macrofollicles, predominance of theca cells and extensive leuteinization, may lead to an erroneous diagnosis of luteinized thecoma.
Sclerosing Peritonitis (SP), which was first described by Owtschinnikow,describes a nonneoplastic inflammatory condition which is characterized by proliferation of fibroblastic and myofibroblastic tissues in the peritoneum, which leads to fibrosis [4]. It presents as white to brown nodules on the surface of the peritoneum, with adhesions. Being most frequently associated with peritoneal dialysis, this condition has been associated with certain drugs, sarcoidosis, SLE, liver cirrhosis, leiomyomata of the uterus, endometriotic cysts or tumours of the ovary, and, recurrent peritonitis [5]. An idiopathic variant has also been reported [6].
Luteinized thecoma of the ovary has been since long found to be associated with sclerosing peritonitis [6]. Clement et al., proposed that luteinized cells of thecoma secrete certain steroid hormones that stimulate fibroblastic proliferation, leading to SP [7]. Later, in a study done on 27 cases of luteinized thecomas with SP, authors observed that the ovarian lesions in SP were rather non neoplastic and they preferred the term, ‘thecomatosis’ over ‘thecoma’ [8]. This was further substantiated by a report on SP which occurred in ovarian thecomatosis, which dramatically responded to medical line of management [9]. Stenram reported a case of benign cystic teratoma which was coupled with SP in a 52-year-old female [10]. Recently, Walker et al., reported for the first time, the occurrence of a luteinized adult granulosa cell tumour of ovary with SP in a 84-year-old female. Patient had an associated FIGO I A endometrioid endometrial carcinoma and she responded well to surgical line of management. Here, the authors suggested that some unknown chemical substance which was secreted by luteinized cells was accountable for sclerosis[6]. Since JGCT primarily exhibits extensive luteinization, a similar substance such as is present in adult GCT, may have led to submesothelial fibroblastic proliferation, leading to SP in the present case.
Clinically, the patients may present with symptoms caused either by SP or JGCT. As far as SP is concerned, it may remain asymptomatic or it may lead to ascitis, abdominal pain, small bowel obstruction, which may be recurrent and at times fatal [7-10]. JGCT occurs in the first two decades of life, but it may span through adulthood. In a large series of 125 cases of JGCT, 82% of the patients presented with isosexual pseudo precocity. A minority of the cases present with abdominal pain, swelling or abnormal uterine bleeding, especially in elderly group. At times, it is detected at the time of pathologic examinations. Its association with Ollier’s disease and Maffucci’s disease has been reported rarely [2].
JGCT is stage 1 disease in a majority of the cases and it has a favourable outcome [3]. Surgery remains the primary mode of treatment [3]. Role of chemotherapy is restricted to advanced or recurrent disease, which gives excellent results. Nodules of SP in peritoneum closely mimic metastatic deposits that may wrongly lead to overstaging of the disease. Awareness on its association with JGCT and an accurate diagnosis are important in view of differing treatment protocols and prognosis.
Treatment options of SP in ovarian tumours have not been standardized, due to rarity of the condition. In some of the cases, peritoneal disease had regressed after treatment of the underlying ovarian pathology, while in others; complication caused by the peritoneal disease had led to considerable morbidity and mortality [8].
To conclude, we present the first case report on association of SP with juvenile GCT of ovary. Pathologists and gynaecologists should be aware of the fact that peritoneal nodules caused by SP should not lead to over staging of ovarian tumours.
[1]. S Sivasankaran, P Itam, L Ayensu-Coker, J Sanchez, RA Egler, ML Anderson, Juvenile granulosa cell ovarian tumor: a case report and review of literature.J Pediatr Adolesc Gynecol 2008 10:1016-20. [Google Scholar]
[2]. RH Young, Sex cord- stromal tumors of the ovary and testis: their similarities and differences with consideration of selected problemsModern Pathology 2005 18:81-98. [Google Scholar]
[3]. RH Young, GR Dickersin, RE Scully, Juvenile granulosa cell tumor of the ovary. A clinicopathological analysis of 125 cases.Am J Surg Pathol 1984 8:575-96. [Google Scholar]
[4]. PJ Owtschinnikow, Peritonitis chronica fibrosa incapsulataArch Klin Chir 1907 83:623-34. [Google Scholar]
[5]. R Kaushik, RP Punia, H Mohan, AK Attri, Tuberculous abdominal cocoon – a report of 6 cases and review of the LiteratureWorld Journal of Emergency Surgery 2006 1(18) [Google Scholar]
[6]. J Walker, EL Moss, R Ganesan, L Hirschowitz, Sclerosing peritonitis associated with a luteinized adult granulosa cell tumor.Int J Gynecol Pathol 2012 31:141-4. [Google Scholar]
[7]. PB Clement, RH Young, W Hanna, RE Scully, Sclerosing peritonitis associated with luteinized thecomas of the ovary: a clinicopathological analysis of six cases.Am J Surg Pathol. 1994 18:1-13. [Google Scholar]
[8]. PN Staats, WG McCluggage, PB Clement, RH Young, Luteinized thecomas (thecomatosis) of the type typically associated with sclerosing peritonitis: a clinical, histopathologic, and immunohistochemical analysis of 27 casesAm J Surg Pathol. 2008 32:1273-90. [Google Scholar]
[9]. JR Mellembakken, V Engh, T Tanbo, B Czernobilsky, E Edelstein, O Lunde, Mitotically active cellular luteinized thecoma of the ovary and luteinized thecomatosis associated with sclerosing peritonitis: case studies, comparison, and review of the literature.Pathol Res Pract 2010 206:744-8. [Google Scholar]
[10]. U Stenram, Sclerosing peritonitis in a case of benign cystic ovarian teratoma: a case report.APMIS. 1997 105:414-6. [Google Scholar]