Obstructive jaundice is one of the most frequent and grave form of hepatobiliary disease. It can pose problems in diagnosis and management, particularly intrahepatic cholestasis [1]. Despite the technical advances, the operative modes of management of obstructive jaundice were associated with very high morbidity and mortality. Yet, during the last decade significant advances have been made in our understanding with regard to the pathogenesis, diagnosis, staging and the efficacy of management of obstructive jaundice [2]. The expanding spectrum of therapeutic options for the jaundiced patient has made it necessary for the radiologist to do more than simply discriminating between obstructive and non-obstructive jaundice. Correct choices among therapeutic options usually rest upon a precise assessment of etiology, location, level and extent of disease [3].
So, it is mandatory to determine pre-operatively the existence, the nature and site of obstruction because an ill chosen therapeutic approach can be dangerous. US has been always considered the first choice technique in the study of biliary obstructive disease, due to its accessibility, speed, ease of performance and low cost [4]. Traditional Computed Tomography (CT) scan is usually considered more accurate than US for helping determine the specific cause and level of obstruction [5]. Both ultrasound and CT scan are regarded as safe and non-invasive procedures in evaluating the status of the biliary tract. Ultrasound is used as an initial modality to confirm or exclude duct obstruction, which it does with at least 90% accuracy [6]. The range of application of CT has been partially restricted by MRCP [7]. MRCP techniques have greatly evolved, providing high resolution images of the biliary tree with short exam duration, while remaining non invasive without contrast medium injection [8].
This prospective study aimed to compare the diagnostic accuracy of Magnetic Resonance Cholangiopancreatography (MRCP) with Ultrasound and Computed Tomography (CT) in evaluation of patients with obstructive jaundice taking direct cholangiographies (ERCP and PTC), hystologic tests and anatomo-pathological findings after surgical intervention as gold standard.
Materials and Methods
The ethics committee of our institute approved this prospective study. Informed consent was taken from all patients undergoing this study. We prospectively studied 50 patients (28 females and 22 males) in the age range 14-82 years over a period starting from January 2012 to December 2013 at SGRD medical college, Amritsar. Initial USG evaluation was followed by CECT and MRI/MRCP, however in patients with Obstructive Jaundice with CBD calculi as diagnosed on USG,CT was performed if required.
Transabdominal ultrasonography was done with convex 1 to 5 Mhz probe on GE Voluson E8 followed by Contrast enhanced Computed Tomography (CECT) done on multislice CT (Siemens – Erlanger, Germany) with collimation of 2 mm. However in cases of benign pathologies where USG findings were unequivocal CECT was not done to avoid unnecessary radiation exposure. MRCP was done in all patients on Philips GyroscanAchieva 1.5 Tesla MRI using our standard MRCP protocol [Table/Fig-1]. The USG, CECT and MRCP results were read by radiologists blinded to other imaging findings.
| TR | TE | FOV | RFOV | NSA | THK | GAP |
|---|
| BFFE TRA | 1500 | 70 | 350-450 | 100 | 2 | 5 | 5 |
| BFFE COR | 1500 | 70 | 350-450 | 100 | 2 | 5 | 5 |
| T1W TFE TRA | SHORTEST | IN PHASE | 350-450 | 100 | 4 | 5 | 5 |
| T2W SPIRRT TRA | 1500 | 70 | 350-450 | 100 | 3 | 5 | 5 |
| SSH MRCP RAD* | 8000 | 800 | 300 | 100 | 1 | 40 | |
As the gold standard we used direct cholangiographies (ERCP and PTC), hystologic tests and anatomo-pathological findings after surgical intervention, in accordance with the appropriate diagnostic and therapeutic approach to the case considered.
All patients with clinical features of biliary obstructive disease were included in the study. Following patients were excluded:
Patients less than 12 years of age.
With contraindications to MRI.
Patients with Prehepatic/Hepatic Jaundice.
Results
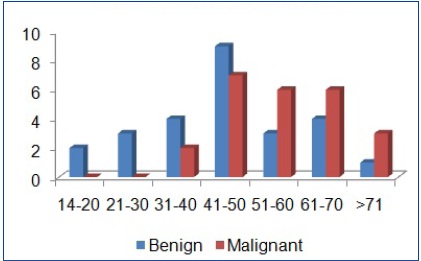
Of the 50 patients included in this study, benign and malignant lesions constituted 26 (52%) and 24 (48%) cases respectively. Age distribution of benign vs milgnant lesions is shown in [Table/Fig-2,3].
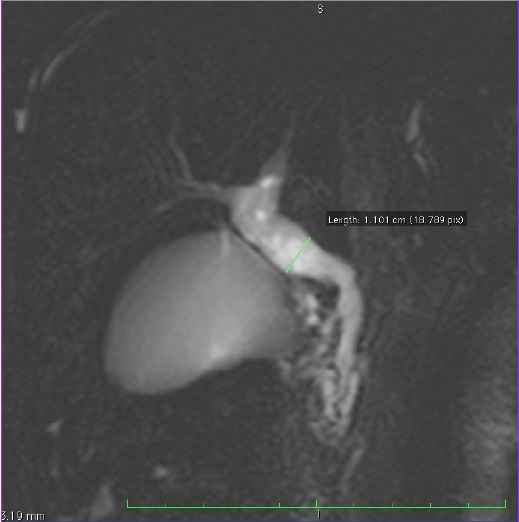
MRCP images shows multiple well defined filling defects(arrow), suggestive of multiple calculi, in the lumen of CBD and CHD

Benign Pathologies
The diagnostic accuracy, sensitivity and specificity of USG,CT and MRCP for different benign pathologies were as shown in [Table/Fig-4,5and6]
Showing Age Distribution of Benign V/S Malignant
| Mode | Total | Percentage |
|---|
| Choledocholithiasis | 15 | 57.7 |
| Benign stricture | 05 | 19.2 |
| Cholangitis | 04 | 15.4 |
| Other benign conditions* | 02 | 7.7 |
| Total | 26 | 100 |
*one case was diagnosed as choledochal cyst while the other showed iatrogenic stenosis as a result of laproscopic cholecystectomy.
“Diagnostic accuracy, sensitivity and specificity - benign pathologies”
| USG | CT | MRCP |
|---|
| DA% | SE% | SP% | DA% | SE% | SP% | DA% | SE% | SP% |
|---|
| Choledo-cholithiasis | 96 | 93.3 | 97.14 | 94.29 | 75 | 96.77 | 98 | 100 | 97.12 |
| Benign Stricture | 100 | 40 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
MRCP image demonstrates cystic dilatation of CHD and Proximal CBD - Choledochal cyst
Fourteen cases confirmed to be choledocholithiasis on final diagnosis were accurately diagnosed on ultrasound. One case was falsely diagnosed as choledocholithiasis on ultrasound that later on ERCP biopsy was diagnosed as cholangiocarcinoma. Ultrasound was unable to diagnose a specific cause for one case where ERCP confirmed the diagnosis to be choledocholithiasis.
Three out of four cases of choledocholithiasis in which CT scan was performed were accurately diagnosed. One case was falsely diagnosed as choledocholithiasis that later on ERCP biopsy was diagnosed as cholangiocarcinoma. CT scan was unable to diagnose a specific cause for one case where ERCP confirmed the diagnosis to be choledocholithiasis.
All fifteen cases were accurately diagnosed on MRI/MRCP. One case was falsely diagnosed as choledocholithiasis on MRI/MRCP that later on ERCP biopsy was diagnosed as cholangiocarcinoma.
Benign Stricture
Ultrasound accurately diagnosed benign stricture in two out of five cases (40%) included in the study.Ultrasound was unable to diagnose a specific cause for three cases where ERCP confirmed the diagnosis to be benign stricture.
CT scan was performed in two cases of benign strictures and both were accurately diagnosed.
All five cases of benign stricture in which MRI/MRCP was performed were accurately diagnosed and findings accurately correlated with the final diagnosis.
Malignant Pathologies
[7,8,9a,9band9c]
| Mode | Total | Percentage |
|---|
| Cholangiocarcinoma | 06 | 25 |
| Periampullary carcinoma | 07 | 29.2 |
| CA head of pancreas | 05 | 20.8 |
| CA gall bladder | 06 | 25 |
| Total | 24 | 100 |
overall accuracy, sensitivity and specificity - malignant lesions
| Malignant | USG | CT | MRCP |
|---|
| DA% | SE% | SP% | DA% | SE% | SP% | DA% | SE% | SP% |
|---|
| Periampullary ca | 94 | 57.14 | 100 | 97.14 | 85.71 | 100 | 100 | 100 | 100 |
| Cholangio-carcinoma | 96 | 66.67 | 100 | 97.14 | 83.33 | 100 | 98 | 83.33 | 100 |
Ultrasound image showing heterogenously hyperechoic mass lesion at the ampullary region causing dilatation of the CBD and MPD
Axial CT image showing a hypoattenuating mass lesion at the ampullary region(arrow) protuding into the lumen of duodenum

T2W SPAIR axial MR image shows a hypointense mass lesion at the ampullary region
MRCP sequence image shows dilated IHBR`s, CHD, CBD and Pancreatic duct – “Double Duct” sign

The diagnostic accuracy, sensitivity and specificity of USG, CT and MRCP for different malignant pathologies were as shown in [Table/Fig-8].
Four out of seven cases of Periampullary carcinoma in which ultrasound was performed were accurately diagnosed. Ultrasound was unable to diagnose a specific cause for three cases where final diagnosis confirmed the diagnosis to be periampullary carcinoma.
Six out of seven cases of Periampullary carcinoma in which CT scan was performed were accurately diagnosed. It was unable to diagnose a specific cause for one case where final diagnosis confirmed the diagnosis to be periampullary carcinoma.
All cases of periampullary carcinoma in which MRI/MRCP was performed were accurately diagnosed.
Four out of six cases of cholangiocarcinoma were accurately diagnosed on ultrasound. One case was falsely diagnosed as choledocholithiasis on ultrasound that later on ERCP biopsy was diagnosed as cholangiocarcinoma. Ultrasound was unable to diagnose a specific cause for one case where ERCP confirmed the diagnosis to be cholangiocarcinoma.
Five out of six cases of cholangiocarcinoma were accurately diagnosed on CT scan and MRI/MRCP. one case was falsely diagnosed as choledocholithiasis that later on ERCP biopsy was diagnosed as cholangiocarcinoma.
The overall accuracy, sensitivity and specificity of USG, CT and MRCP in benign and malignant lesions observed in this study are as shown in [Table/Fig-10].
Overall accuracy, sensitivity and specificity of USG, CT and MRCP in benign and malignant lesions
| Malignant | USG | CT | MRCP |
|---|
| DA% | SE% | SP% | DA% | SE% | SP% | DA% | SE% | SP% |
|---|
| Benign Conditions | 88 | 80.77 | 95.83 | 82.86 | 54.55 | 95.83 | 98 | 100 | 95.83 |
| Malignant Conditions | 88 | 79.17 | 96.15 | 91.43 | 91.67 | 90.91 | 98 | 95.83 | 100 |
Discussion
The opinion is broadly shared that US is the first choice option in the diagnosis of choledocholithiasis. Our results for US diagnostic accuracy, sensitivity and specificity are in accordance with those reported in literature. Boraschi et al., reported a specificity of over 90% [9]. In the literature, a sensitivity range of 20 to 80% is often documented [10]; these considerable differences in sensitivity among various case series are partially attributable to the impossibility of approaching the distal CBD and ampullary region in obese patients and patients with abdominal meteorism, as well as to the variability of the US technique applied.
The high sensitivity in our study presumably derives from the use of dosed compression, and to THI, which allowed for better study of the distal tract of the CBD. As described by Ortega et al., [11], harmonic imaging, by improving contrast resolution, stresses the difference between the anechoicity of the duct lumen and the surrounding soft tissues.
Todua et al., [12], has mentioned that for choledocholithiasis, CT is similar to ultrasound, with a sensitivity range of 23% to 85% and specificity of 97%. Present study showed similar results.
MRCP diagnostic accuracy, sensitivity and specificity are comparable to those reported in the literature (Calvo et al., [10], Huassein et al., [13], Boraschi et al., [9] Varghese et al., [14]) where sensitivity, specificity and diagnostic accuracy respectively range between 81–100%, 84–100% and 90– 96%.
Study conducted by Al-Obaidi et al., [15] showed higher sensitivity (100%), specificity (98.5%), accuracy (98.7%) of MRI/MRCP for cases with benign stricture as compared to sensitivity of USG (44.4%) which is consistent with present study.
Andersson M et al., [16] concluded in their study that MRI with MRCP was more accurate than CT in differentiating between malignant and benign lesions in patients with suspected periampullary tumors. This is consistent with present study where MRI/MRCP showed 100 % accuracy in diagnosing cases with periampullary carcinoma.
The overall sensitivity was 66.67%, specificity was 100% and accuracy was 96% for cases with cholangiocarcinoma on ultrasound with a negative predictive value of 95.65%. The finding of our study approximate with findings by Hann et al., [17] who reported that ultrasonography detected 87% of Klatskin tumor.
Verma et al., [18] demonstrated the sensitivity and specificity of 85.3% and 88.4% on ultrasound, 84.6% and 94.2% on CT, 92.3% and 86% on MRCP for detecting the benign etiology of obstruction. Ferrari FS et al., [19] demonstrated similar findings for benign lesions in their study. The diagnostic accuracy, sensitivity and specificity of USG was 78.62%,16.67% 97.29%, of CT it was 92.59%,92.3%.92.85% and of MRCP was 93.13%,90%,94% respectively.
Similar results were found in present study in which the overall sensitivity was 80.77%, specificity was 95.83% and accuracy was 88% for cases with benign conditions on ultrasound.The sensitivity for CT is inconsistent with the study conducted by Verma et al., [18]. This discrepancy could be because of the small subject size in our study. However the specificity demonstrated in their study was 94.2%, which is consistent with present findings.
Verma et al., [18] demonstrated the sensitivity and specificity of 88.4% and 85.3% on ultrasound, 94.2% and 85% on CT, 86% and 92% respectively for detecting the malignant etiology of obstruction. Ferrari FS et al., [19] demonstrated the diagnostic accuracy, sensitivity and specificity of USG 93.13%, 61.12%, 98.23% and 92.59%, 90.9%, 93.75% of CT and 93.13%, 90%, 94% of MRCP respectively.
Similar results were found in present study in which the overall sensitivity was 79.17%, specificity was 96.15% and accuracy was 88% for cases with malignant conditions on ultrasound.
Limitations
1) In some cases, pancreatic head and peripancreatic region were poorly visualized on ultrasonography due to bowel gas shadows.
2) Some patients were unable to hold their breath for the interval required. This compromised the quality of the 3D MRCP sequence in these cases.
Recommendations
Ultrasound as a screening modality is useful to confirm or exclude biliary dilatation and to choose patients for MRCP examination. It accurately demarcates the level of obstruction and therefore influences clinician’s diagnosis and management plans. Participating patients preferably should be in a fasting state four hours prior to the ultrasound and MRCP investigation.Ultrasound and Spiral CT have high diagnostic accuracy and specificity and along with MRCP have largely confined the role of invasive cholangiography (ERCP) to therapeutic/palliative procedures, rather than primary diagnostic tests in modern setup.
Conclusion
MRI-MRCP was superior to ultrasound and CT scan in studying both the benign and malignant lesions. Periampullary carcinoma was the commonest malignant etiology, while choledocholithiasis was the commonest benign cause. MRCP is the modality of choice for optimal characterization of the causative lesions in most of the cases of obstructive jaundice. MRI-MRCP was superior to ultrasound and CT scan in studying both the benign and malignant lesions.