Elderly population faces a number of health issues and falls are among the most important ones [1] leading to injury, dependency and death in a considerable proportion [2]. The incidence of falls and related injuries is relatively high among institutionalised elderly compared to subjects living independently in the community [3].
Most falls in elderly result from the complex interplay of intrinsic and extrinsic factors [4]. Studies have shown that elderly subjects who fall, demonstrate impaired functioning in sensori-motor factors accountable for balance or postural stability [3]. Inactive lifestyle [5], and physiological changes related to aging, characterized by senile sarcopenia and progressive decline in muscle strength, joint range of motion, reaction time, and sensory system lead to reduced physical performance and increased risk of fall [6,7].
The relationship between impairments in generation of muscle force and balance has been explored. The force generating capacity of the ankle muscles, weakness of hip flexors, extensors, and abductors, reduced torque and power of knee flexors, knee extensors, ankle dorsiflexors and plantar flexors are found to be either predictors or contributors for postural instability during dynamic activities [8,9].
Studies addressing fall prevention have focused on various group and individualised strength training programmes [10]. Many of the progressive resistance training interventions designed to increase strength [11] and reduce the falls in elderly [11,12] were effective in reducing both rate of falls and risk of falling, especially when some form of balance exercise was an integral part of the programme. Similarly, studies have evaluated the effects of strength training alone and the results of such studies were inconclusive [12,13]. Considerable number of studies lacked the control group and many failed to strengthen key muscles necessary for maintaining balance and postural control [12,14,15].
This study evaluated the effectiveness of individualised progressive resistance strength training (PRT) programme using sand bags in improving balance for forward limits of stability in non-frail elderly with balance impairment, compared to traditional balance exercise (TBE), and a combination of both (COMBI).
Materials and Methods
A randomised controlled trial among elderly subjects aged 65 years and above, residing in 4 old age homes in Mangalore, Southern India, was conducted between June 2008 and December 2012.
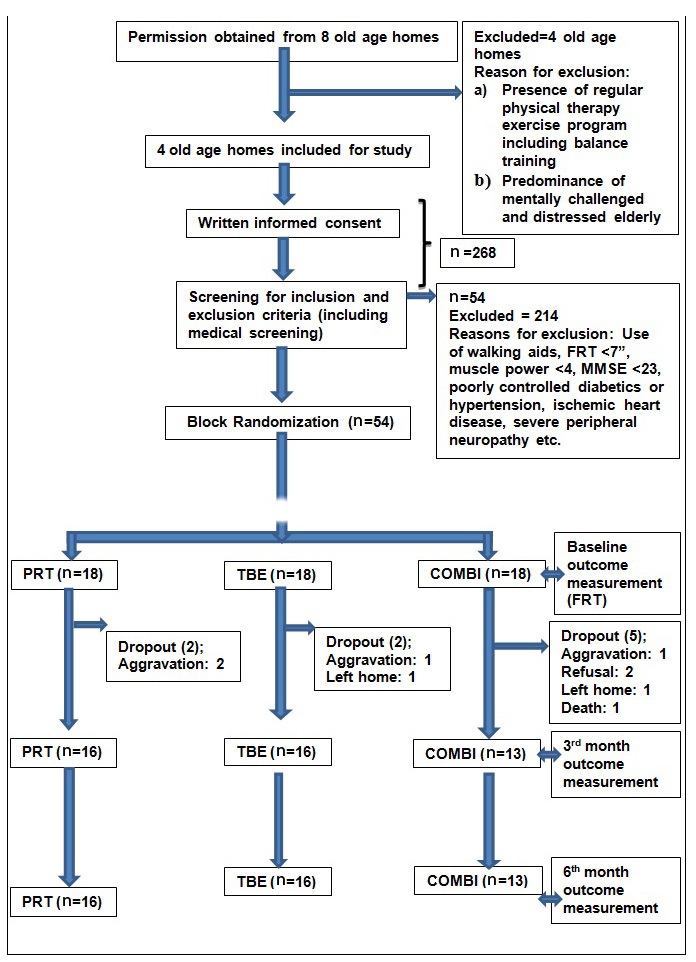
The sample size was calculated using a ready reckoner table [16]; anticipating 4.5cm as the clinical difference for functional reach test (FRT) [17], with an expected standard deviation of 5 each, intraclass correlation coefficient of 0.3 with 3 repeated measures, a significance level of 5%, a power of study of 80% and an expected 10% dropout for each group; the sample size derived was 54 elderly subjects; 18 in each group.
To obtain the sample size, a total of 268 subjects from 4 different old age homes were screened. The eligible subjects were assigned to the study groups by sequenced generation using block randomisation. Block size of 6 was used in the trial to allocate the participants to the three interventions i.e. each block consisted of 2 PRT, 2 TBE and 2 COMBI interventions. The allocation concealment was done using sealed opaque envelopes which was sequentially arranged.
The subjects who gave consent underwent medical screening and screening for inclusion and exclusion criteria. Subjects aged 65 years and older, of both gender, medical screening clearance, Berg balance scale (BBS) score of 41 to 52 [18], Mini Mental State Examination (MMSE) score of ≥23, a minimum score of 17.5 cm (7 inches) on FRT [19] and a muscle strength grade of 4 or above for the lower limb muscle groups were considered as the criteria for including subjects for the study. Symptomatic cardiovascular diseases, neurological conditions, peripheral neuropathy of lower limbs with significant dorsal column sensory loss, musculoskeletal condition of the lower quarter which could interfere with measuring outcome, malignancies, medications which carry the risk of causing falls, diagnosed vestibular disorders and subjects who underwent lower limb strength training and/or balance training during the past 3 months were the criteria to exclude the subjects.
Measurement scale, foam of 3-4″ thickness with length of 6.5 feet and width of 3 feet, standard treatment plinth, sand bags of varying weights ranging from 250gm to 5 kgs, and a medium size Swiss ball were the materials used for the study.
After obtaining the clearance from the Institutional Ethics Committee (IEC) of Kasturba Medical College (Manipal University), Mangalore,India the list of old-age homes, in Mangalore region was prepared. Among the 12 old age homes identified, 8 consented to participate in the study. Out of the 8 old age homes, 4 centres were excluded due to presence of regular exercise therapy including balance training for the inmates and predominance of mentally challenged and distressed elderly. From the remaining homes, after obtaining the permission, written informed consent was collected from the subjects. Following medical screening by a qualified medical practitioner, the independent blinded observer administered the BBS, FRT, manual muscle testing and MMSE on the identified subjects. The baseline values were recorded and preserved for data analysis [Table/Fig-1].
The TBE group received traditional or conventional balance exercise for approximately 45 minutes. Traditional balance exercises consisted of 8 components and they were weight-shifts, standing on one leg, tandem walking, crossover walking, figure of eight walking, forward, backward and sideways walking on foam, sitting balance on a medium size Swiss ball and perturbations of balance in all directions while sitting on plinth, foam and Swiss ball. Based on the ability of the participant, the complexity of the balance training was increased. A rest period of 1 minute was given between each component. All the subjects of the TBE group were given balance exercises for 4 times a week for a period of 6 months.
The PRT group received resistance training for the key muscles of both lower extremities. DeLormes and Watkins protocol [20] was used for progressive resistance strength training, which lasted for approximately an hour per session. The muscle groups strengthened were hip flexors, extensors and abductors, knee flexors, and extensors, and ankle dorsiflexors and plantarflexors. PRT group subjects were instructed to raise or lift the weight (concentric muscle action) within 1-2 seconds and then lower the weight (eccentric muscle action) within 2-3 seconds. A rest period of 1 second between movements and 30 seconds to a minute between sets were given. The starting positions used for strengthening the key muscles were also deployed for determining the 1 RM, for the respective muscle group. Brzycki’s equation [21] i.e. 1 RM = Weight ÷ [1.0278 - (0.0278 × Number of repetitions)], was used to determine Max load or 1RM for each muscle group.
The 1-RM tests were conducted every 2 weeks and to avoid the possibility of undue fatigue and tiredness, the tests were performed on rest days. Similarly, to minimize musculoskeletal injuries, the subjects were given 15RM (65% of 1RM) instead of prescribed 10RM of DeLormes and Watkins protocol during the first four weeks.
The COMBI group received PRT and TBE alternately, thus making 2 days of PRT and 2 days of TBE in a week. The strengthening and balance training procedure received by COMBI group was identical to the exercise regimen of PRT and TBE groups.
All the subjects irrespective of the group were encouraged to perform to their best capability at all times including the test for 1RM calculation. At the end of 3rd and 6th month the blinded outcome assessor re-assessed and recorded the outcome measure.
Most of the subjects who received strength training programme for PRT and COMBI groups had few days of Delayed Onset Muscle Soreness (DOMS), which were symptomatically treated with reassurance and thermal agents. However, 2 subjects of PRT group and 3 of the COMBI group had considerable aggravation of their arthritic joint pain and refused to continue the exercise programme and were omitted from this study [Table/Fig-1]. The number of sets of resistance training and the position of sand bag (resistance) were modified for those subjects who had worsening of arthritic pain or DOMS. Similarly, subjects who felt uneasy, or lacked desire to perform the exercises on the designated day, were exempted from exercises on the same day, but the exercises were given on the subsequent rest day.
Statistical Analysis
The collected data was analysed using Statistical Package for Social Sciences (SPSS) version 15. Comparison of baseline characteristics of the three groups was carried out using one way ANOVA for the continuous variables and chi square test for the categorical variables. Repeated measures ANOVA was used for comparison of outcome measure over time between the three groups. The change score pre-post intervention was analysed using Kruskal Wallis test followed by Mann-Whitney U test adjusted for alpha error for pairwise comparison. The analysis was performed using both per-protocol and intention to treat. A p-value of less than 0.05 was considered as statistically significant.
Results
The study included 54 elderly subjects aged 65 years and older. The mean scores of most of the variables other than FRT, and incidence of falls last year [Table/Fig-2,3], were not statistically significant, suggesting that the three groups were essentially homogeneous with respect to those baseline values. The analysis of FRT scores revealed a statistically significant difference between the three groups (p=0.023). Post-hoc analysis (Tukey) of baseline values for FRT revealed a statistically significant difference between TBE and PRT groups (p=0.014).
Baseline characteristics of the study groups
| Baseline Variables | PRT (n=18) | TBE (n=18) | COMBI (n=18) | Total (54) | Test Statistic | p-value |
|---|
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD |
|---|
| Age | 75.11 ± 5.497 | 75.17 ± 5.894 | 75.22 ± 5.253 | 75.17± 5.449 | f= 0.002 | 0.998 |
| Gender n(%) | Male | 6 (33.3%) | 6 (33.3%) | 1 (5.6%) | 13 (24.1%) | χ2 = 5.412 | 0.1 |
| Female | 12 (66.7%) | 12 (66.7%) | 17 (94.4%) | 41 (75.9%) |
| MMSE | 25.67 ± 2.169 | 26.44 ± 2.148 | 25.72 ± 2.321 | 25.94 ± 2.201 | f= 0.691 | 0.506 |
| BBS | 46.5 ± 3.899 | 48.72 ± 2.675 | 48.61 ± 2.704 | 47.94 ± 3.253 | f= 2.854 | 0.067 |
| FRT(cm) | 20.36 ± 2.674 | 23.66 ± 3.765 | 21.9 ± 3.843 | 21.97 ± 3.665 | f= 4.079 | 0.023* |
*Significant PRT, Progressive Resistance Strength Training; TBE, Traditional Balance Exercise; COMBI, combination of both Progressive Resistance Strength Training and Traditional Balance Exercise; n, no; SD, Standard Deviation; MMSE, Mini-Mental Status Examination; BBS, Berg Balance Scale; FRT, Functional Reach Test
Proportion of subjects with peripheral neuropathy, musculoskeletal disorder, hypertension, diabetic mellitus and incidence of falls last year
| Baseline Characteristics | PRT (s=18) | TBE (s=18) | COMBI (s=18) | p-value |
|---|
| n (%) or Median (IQR) | n (%) or Median (IQR) | n (%) or Median (IQR) |
|---|
| Peripheral Neuropathy | 8 (44.4%) | 9 (50.0%) | 7 (38.9%) | 0.94 |
| Musculoskeletal disorder | 9 (50.0%) | 5 (27.8%) | 7 (38.9%) | 0.449 |
| Hypertension | 5.5 (0,9.25) | 6 (0, 8.5) | 2 (0,8.0) | 0.739 |
| Diabetic Mellitus | 7.5 (0,13.5) | 8.5 (0, 12.25) | 7.5 (0,12.25) | 0.827 |
| Incidence of falls last year | 1.5 (0,3.0) | 0 (0, 1.0) | 1.5 (0, 3.25) | 0.049* |
*Significant
PRT, Progressive Resistance Strength Training; TBE, Traditional Balance Exercise; COMBI, combination of both Progressive Resistance Strength Training and Traditional Balance Exercise; s, subjects; N, no; IQR, Inter-quartile Range
With regard to incidence of falls last year [Table/Fig-3], a statistically significant difference was seen between the three groups (p=0.049). But, the pairwise comparison did not show statistically significant difference between any of the groups (p=0.09). Since there were 9 dropouts [Table/Fig-1], only 45 of the remaining participants were included for the per-protocol data analysis.
For both per-protocol and intention to treat analysis [Table/Fig-4], for functional reach, the PRT had a steady progression from the baseline to 6 months which was highly statistically significant (p<0.001). The TBE and COMBI groups showed considerable improvement from baseline to third month and beyond which moderate improvement was seen. Both methods of analysis revealed a highly statistically significant improvement for COMBI group (p<0.001) and a significant improvement for TBE group (p=0.006).
Changes in FRT in study groups from baseline to 3 Months and 6 Months of intervention
| Variable | Groups | Analysis | Baseline Mean ± SD (n) | 3 Months Mean ± SD (n) | 6 Months Mean ± SD (n) | f-value | p-value |
|---|
| FRT(cm) | PRT | PP | 20.36 ± 2.674 (18) | 25.25± 1.873 (16) | 27.659± 2.305(16) | 63.254 | <0.001† |
| ITT | 24.98±1.923(18) | 27.12±2.666(18) | 43.392 | <0.001† |
| TBE | PP | 23.66 ± 3.765 (18) | 26.52± 5.424 (16) | 28.444± 5.453 (16) | 7.211 | 0.006* |
| ITT | 25.9±5.408(18) | 27.61±5.67(18) | 6.896 | 0.006* |
| COMBI | PP | 21.9 ± 3.843 (18) | 25.67 ± 1.898 (13) | 28.01± 2.316 (13) | 108.644 | <0.001† |
| ITT | 25.46±3.163(18) | 27.15±3.63(18) | 31.625 | <0.001† |
*Significant †Highly Significant SD, Standard Deviation; n, no; FRT, Functional Reach Test; PRT, Progressive Resistance Strength Training; TBE, Traditional Balance Exercise; COMBI, combination of both Progressive Resistance Strength Training and Traditional Balance Exercise; PP, Per-protocol; ITT, Intention to treat
The change scores of FRT [Table/Fig-5] was notable for both PRT and COMBI when compared to TBE group, and per-protocol analysis did reveal a statistically significant difference (p=0.024). Post-hoc analysis (Mann-Whitney U-test) of the same revealed PRT to be statistically significantly better than TBE (p=0.014).
Change scores of FRT in study groups between baseline and 6 Months of intervention
| Variables | Analysis | PRT (n=16) Median (IQR) | TBE (n=16) Median (IQR) | COMBI (n=13) Median (IQR) | p-value |
|---|
| FRT(cm) | PP | 7.6 (4.575, 9.8) | 2.55 (1.675, 8.25) | 7 (5.4, 9.05) | 0.024* |
| ITT | 7.3(4.185, 9.2) | 2.4 (1.2, 6.95) | 5.9 (0, 7.76) | 0.152 |
*Significant PRT, Progressive Resistance Strength Training; TBE, Traditional Balance Exercise; COMBI, combination of both Progressive Resistance Strength Training and Traditional Balance Exercise; n, no; IQR, Inter-quartile Range; FRT, Functional Reach Test; PP, Per-protocol; ITT, Intention to treat
Discussion
The present study maintained strict methodological guidelines with regard to randomisation, outcome assessor blinding and use of gold standard outcome measure. Overall result of the study showed substantial improvement in balance, among all the three groups. However, PRT showed more improvement in balance with enhanced limits of stability compared to TBE and this finding is consistent with the objective.
Among the fall prevention exercise programmes targeted to improve balance impairments, supervised one to one programme were found to be relatively safer with regard to adverse events during the interventions and showed better adherence among the subjects [4,22]. The present study was carried out with complete supervision by a well-qualified physiotherapist on a one to one basis for a period of 6 months and throughout the study period none of the participants experienced any untoward events such as falls or fractures.
Balance training has been considered as an essential component of fall prevention programmes [23] and the exercise components basically train individuals to maintain or regain the centre of gravity inside the base of support thus controlling the postural sway and reducing the incidence of fall [12]. Many of the earlier studies attribute this finding to better neuromuscular coordination and “specificity of the training” [3,6,24]. For the above mentioned reasons, the current study used traditional balance training programme as the control group.
Many studies [25–27] did not target the key muscles required to maintain the balance as against the present study which could explain better forward limits of stability for PRT and COMBI groups compared to TBE group.
Significant improvement in functional reach among PRT and COMBI groups when compared to TBE group and a significantly better functional reach change score for PRT group compared to TBE, clearly indicates that PRT is as good as or possibly superior to conventional balance training, provided the strength training programme is well structured, progressive and supervised, and targets the key muscles.
Strength training increases the muscle size, which is largely the result of an increase in contractile protein content seen especially in type II muscle fibres that contribute mainly for quick reaction time and maintenance of balance. The improvement in the muscle mass, strength, composition, power and torque production and modification of mechanical properties of tendon [7,28] all may have contributed for enhanced balance in PRT group.
The improvement in the functional reach for PRT group, following moderate to high intensity and slow velocity training could be the result of higher neural adaptations such as enhancement of motor neuron firing rate, increased neurotransmitter release at the neuromuscular junction and change in biophysical properties of the motor neuron [29]. The present study also assumes that increase in the strength, specifically of the muscles around the ankle may have provided greater amount of stability to perform a dynamic activity like functional reach. Functional reach requires eccentric rather than concentric muscle contraction of plantarflexors [8]. Low velocity eccentric muscle strength training given for both PRT and COMBI groups also could have led to a difference in functional reach score, compared to TBE.
Balance training improves balance in elderly, but not muscle strength [6,24]. On the contrary, strong evidence supports the view that PRT can increase the ability to generate muscle force in elderly. In addition to the above, PRT programmes are found to be beneficial in improving the bone mineral density, increase fat-free mass and functional activities in elderly and glycemic control in type 2 diabetes mellitus [30]. Although there is no clear evidence on the effectiveness of PRT as a stand-alone intervention on balance [6], the current study, did show significant beneficial effect on forward limits of stability of balance in non-frail elderly, provided structured progressive resistance training is given to the key muscles of lower limbs.
Conclusion
With respect to time, all groups (PRT,TBE and COMBI) had significant improvement in forward limits of stability of balance over 6 month duration. However, between the groups; the PRT group had significantly higher change scores compared to TBE group. Therefore, individualised structured PRT intervention targeting the key muscles of bilateral lower limbs 4 times a week for a period of 6 months is more effective than TBE in improving forward limits of stability of balance among non-frail institutionalised elderly aged 65 years and older.
*Significant PRT, Progressive Resistance Strength Training; TBE, Traditional Balance Exercise; COMBI, combination of both Progressive Resistance Strength Training and Traditional Balance Exercise; n, no; SD, Standard Deviation; MMSE, Mini-Mental Status Examination; BBS, Berg Balance Scale; FRT, Functional Reach Test
*SignificantPRT, Progressive Resistance Strength Training; TBE, Traditional Balance Exercise; COMBI, combination of both Progressive Resistance Strength Training and Traditional Balance Exercise; s, subjects; N, no; IQR, Inter-quartile Range
*Significant †Highly Significant SD, Standard Deviation; n, no; FRT, Functional Reach Test; PRT, Progressive Resistance Strength Training; TBE, Traditional Balance Exercise; COMBI, combination of both Progressive Resistance Strength Training and Traditional Balance Exercise; PP, Per-protocol; ITT, Intention to treat
*Significant PRT, Progressive Resistance Strength Training; TBE, Traditional Balance Exercise; COMBI, combination of both Progressive Resistance Strength Training and Traditional Balance Exercise; n, no; IQR, Inter-quartile Range; FRT, Functional Reach Test; PP, Per-protocol; ITT, Intention to treat