Hypertension is a disease affecting about 65.4% of people aged over 60 years and is responsible for 6% of all deaths worldwide [1,2]. Its prevalence in India is 22% – 45% among men and about 16% – 38% among women [3]. Long standing hypertension often progresses to left ventricular hypertrophy (LVH), an independent risk factor for predicting acute coronary syndrome, stroke, sudden cardiac death or heart failure [4]. Although LVH can be caused by other cardiovascular conditions too, this study specifically considers LVH caused by hypertension alone due to the large disease burden of hypertension in our country. Further, this study intends to evaluate patients with hypertension in particular and not patients with other cardiac illnesses.
The electrocardiogram (ECG) is an easily available and cost effective tool to evaluate LVH easy to use described criteria. Its efficacy is often questionable as compared to more specific tools like echocardiography, magnetic resonance imaging, and autopsy studies. However, the two-dimensional echocardiography is often referred to as the gold standard to evaluate LVH, its efficacy is not as much as that of higher imaging modalities. Further, being equipped with at least echocardiographic facilities requires not just the infrastructure but also the presence of skilled personnel. The lack of financial support and manpower in the medical field especially in rural primary health centres certainly poses a challenge to the feasibility of echocardiographic evaluation at the grass root level of medical care. Hence it is essential to find out whether the ECG can be used as a tool to screen for LVH in the rural setup (or even in urban areas as echocardiography is more expensive if the only indication is ‘screening’) instead of echocardiography. If so, it may be utilised effectively in identifying LVH at rural primary health centres thus reducing the already saturated patient load at higher centres and the facilities could be availed by the more deserving patients.
Certainly, there are better imaging modalities than two-dimensional echocardiography to measure left ventricular mass index like three-dimensional echocardiography and cardiac magnetic resonance imaging. These advanced imaging modalities definitely have better sensitivity, specificity and accuracy of diagnosis of LVH. However, they are time-consuming and expensive and are not employed as often as the gold standard – two-dimensional echocardiography. In fact, these advanced modalities are not common even at tertiary health centres, and even when available, they are too expensive to be considered as tools to screen for left ventricular hypertrophy. Hence this study compares the diagnostic efficacy of ECG with that of two-dimensional echocardiography.
(1) To assess the efficacy of ECG criteria to screen for left ventricular hypertrophy in comparison to echocardiography.
(2) To determine whether ECG can be used as a screening tool for LVH in rural primary health centres.
Materials and Methods
A retrospective diagnostic study was conducted in January 2012 at a tertiary care hospital in Mangalore, Southern India. Purposive sampling method was employed and patients admitted to the hospital during the past 6 months with a history of hypertension were considered. The study population belonged to the rural, semi-urban and urban areas in South-Western Karnataka and Northern Kerala.
The Inclusion Criteria were: Age above 18 years, diagnosed hypertension as per JNC - 7 guidelines, either on or off treatment, and having a documented ECG and echocardiogram done in the same 48 hours.
The Exclusion Criteria were: Congenital heart disease, valvular heart disease, ischemic heart disease, pericardial disease, eccentric hypertrophy by echocardiography, right ventricular hypertrophy, and arrhythmias or conduction abnormalities.
Among the 418 patients initially considered, a total of 50 patients fulfilling the above criteria were included in the study. Details such as age, gender, height, weight, treatment for hypertension, and clinical findings of pulse, blood pressure and cardiovascular examination were recorded in the data sheet. Among the 50 patients, 30 were males and 20 were females. Most patients (66%) were from the age group of 51 - 70 years.
ECGs had been recorded using the ‘BPL Cardiart 6108T’ machine using standard calibration.
The Romhilt-Estes and Sokolow-Lyon criteria were applied to all 50 patients as follows:
The Romhilt-Estes point-scoring system [5]: (RE1: Amplitude: ANY of these three = 3 points. (Largest R or S in the limb leads ≥ 20mm; S wave in V1 or V2 ≥ 30mm; R wave in V5 or V6 ≥ 30mm). RE2: ST-T change of typical LV strain = 3 points. RE3: Left atrial involvement (Terminal negativity of P in V1 > 1mm and longer than 40 milliseconds) = 3 points. RE4: Left axis deviation -30 or more = 2 points. RE5: QRS duration ≥ 90 milliseconds = 1 point. RE6: Intrinsicoid deflection in V5, V6 ≥ 50 ms = 1 point). A score of 4 or more was taken as LVH.
Sokolow-Lyon Voltage Criteria of Precordial Leads for LVH [6]: (S in V1) + (R in V5 or R in V6) > 35mm; (R in V5) or (R in V6) > 26mm). Any of the above two conditions being positive was taken as LVH.
Body surface area for each patient was calculated using Dubois formula as follows:
BSA (m2) = 0.007184 x (weight in kg) 0.425 x (height in cm) 0.725.
Echocardiography had been performed using the 6S probe (2.7-8.0MHz) of the ‘GE Vivid S5’ machine and dimensions were measured while visualizing the heart in the long axis view. Left ventricular mass was calculated according to the formula proposed by the American Society of Echocardiography [7] as: LV mass (g) = 0.8 x 1.04 [(IVS+LVID+LVPW)3- (LVID)3] + 0.6. LV mass index (LVMI) was calculated as: LVMI: LV mass (g) / BSA (m2).
Patients were divided into two groups based on LVMI by 2D echocardiography as follows: LVH group: Those patients whose echocardiography reveals concentric LVH and LVMI greater than or equal to 116 g/m2 for males and 104 g/m2 for females. Non-LVH group: Those patients whose echocardiography reveals no evidence of concentric LVH and LVMI less than 116 g/m2 for males and 104 g/m2 for females.
The obtained data was analysed based on sensitivity, specificity, positive predictive value and negative predictive value by Kappa statistics. Scatter plot to determine correlation between the criteria and LVH by echocardiography was also done.
Results
Among the 50 patients in this study, 23 (46%) had LVH documented by echocardiography.
The diagnostic power of LVH analysed by the Romhilt-Estes and Sokolow-Lyon ECG criteria is represented in [Table/Fig-1]. We observed high specificities (96.3%, 88.9%) and positive predictive values (90.9%, 76.9%) of LVH by the Romhilt-Estes and Sokolow-Lyon ECG criteria respectively, but both had low sensitivities (43.5%, 43.5%). Romhilt-Estes point score system was better than Sokolow-Lyon criteria considering sensitivity, specificity, positive as well as negative predictive value. Further combining the Romhilt-Estes and Sokolow-Lyon criteria for LVH improved the sensitivity from 43.5% to 60.9%.
Sensitivity, specificity, predictive values of Romhilt-Estes and Sokolow-Lyon ECG criteria in determining LVH
| Parameter | Patients | Romhilt-Estes | Sokolow – Lyon | Combined |
|---|
| Sensitivity | Male | 57.1% | 42.9% | 64.3% |
| Female | 22.2% | 44.4% | 55.6% |
| All 50 | 43.5% | 43.5% | 60.9% |
| Specificity | Male | 93.8% | 81.3% | 75.0% |
| Female | 100% | 100% | 100% |
| All 50 | 96.3% | 88.9% | 85.2% |
| Positive predictive value | Male | 88.9% | 66.7% | 69.2% |
| Female | 100% | 100% | 100% |
| All 50 | 90.9% | 76.9% | 77.8% |
| Negative predictive value | Male | 71.4% | 61.9% | 70.6% |
| Female | 61.1% | 66.8% | 73.3% |
| All 50 | 66.7% | 64.9% | 71.9% |
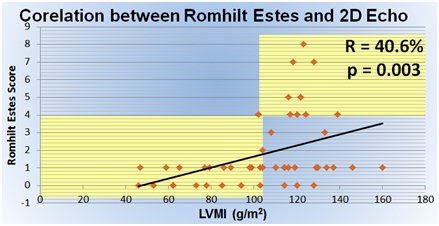
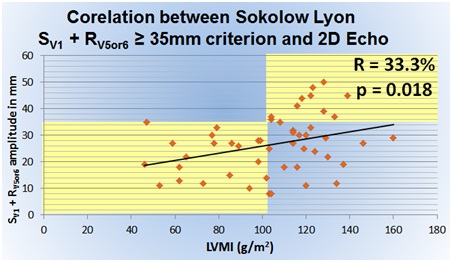
The correlation between the ECG criteria and echocardiography are represented in the [Table/Fig-2,3and4]. In these figures, the patients are represented by plotted dots; with the x-axis representing the left ventricular mass index calculated from echocardiography and the y-axis representing the ECG scores. The areas shaded yellow indicate those patients in whom the ECG criteria and echocardiographic findings showed correlation (the top right area shaded yellow indicating ECG and echo positive for LVH; the bottom left area shaded yellow indicating ECG and echo negative for LVH).
Romhilt-Estes point score system showed a moderate correlation of 40.6% and this value was significant (p=0.003)
The first criterion of Sokolow-Lyon criteria showed a poorer correlation of only 33.3% and this value was significant (p=0.018)
The second criterion of Sokolow-Lyon criteria showed no significant correlation with echocardiography (p=0.206)
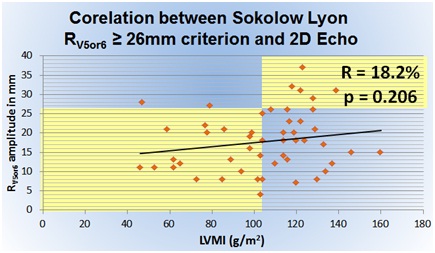
Romhilt-Estes point score system showed a moderate correlation of 40.6% with LVMI by echocardiography [Table/Fig-2]. Here only 45 dots are seen instead of 50 as five pairs of patients incidentally had the same ECG score and LVMI value. This occurred because the Romhilt-Estes score has a narrow range of 0 to 13, and over 70% of our patients scored less than 2 on the Romhilt-Estes point score. The correlation of the first Sokolow Lyon criteria (33.3%) is less than that of Romhilt-Estes score (40.6%). The second of Sokolow-Lyon criteria showed no significant correlation with LVMI (p=0.206).
Discussion
This study compared the diagnostic power of the Romhilt-Estes and Sokolow-Lyon criteria to detect LVH by ECG with that measured by echocardiography. Most patients (46%) in our study had LVH by echocardiography. In the original study by Romhilt and Estes 360 hearts were autopsied by chamber dissection and 44.4% of the subjects were found to have LVH [5]. Although they did not use echocardiography, LVH was graded by the weight of left ventricular myocardial tissue. Romhilt and Estes introduced the point score system and observed a sensitivity and specificity of 54% and 3% respectively as compared to LVH detected by chamber dissection autopsy. Our study had a comparable sensitivity of 43.5% but a specificity of 96.3%. Similarly, Romhilt and Estes also evaluated the Sokolow Lyon criteria by comparing them with the chamber dissection technique and found out that it had a sensitivity and specificity of 42.5% and 5%. The present study detected a similar sensitivity of 43.5%, but a specificity of 88.9%. While the sensitivities between our study and the original study by Romhilt et al., are similar, the specificities show disparity. This difference could be from the non-exclusion of aortic stenosis, right ventricular hypertrophy, eccentric hypertrophy, possible pericardial disease and ischemic heart disease in the original study by Romhilt and Estes [5].
Morrison et al., evaluated 127 patients using ECG and echocardiography, of whom 60 patients had LVH by echocardiographically determined LVMI [8]. Their methods were similar to those of our study. Their study revealed sensitivities of the Romhilt-Estes and Sokolow-Lyon criteria to be very low; 16.7% and 6.7% respectively, which contradicts our values of 43.5% and 43.5% respectively. However the specificities of the two criteria by Morrison et al., were 95.7% and 95.7% comparable to 96.3% and 88.9% in our study.
Reichek N and Devereux RB studied 34 patients by comparing similar ECG criteria with echocardiography and chamber dissection findings of LVH [9]. Their methods were a combination of those adopted by Romhilt and Estes and those used in our study. According to them, the Romhilt-Estes and Sokolow-Lyon criteria were poorly sensitive (50% and 21% respectively) as compared to results of our study (43.5% and 43.5% respectively). But the specificities of the two criteria were 95% and 95% as comparable to 96.3% and 88.9% measured in our study.
Our results of correlation of ECG criteria with echocardiography were in agreement with those of Reichek N and Devereux RB (40.6% vs 64.0% correlation with echocardiography by Romhilt Estes point score system; poor correlation by Sokolow Lyon criteria) [9]. Sohaib SMA et al., also found that Sokolow-Lyon criteria have a poor correlation of 28% with LVMI [10]. Various studies have found out that while the sensitivity of ECG criteria for LVH is less than 57%, the specificity is often about 85 -90% [11–16].
The sensitivity of both criteria was 43.5%, while specificity was 96.3% for Romhilt-Estes criteria and 88.9% for Sokolow-Lyon criteria. When combining Romhilt-Estes and Sokolow-Lyon criteria for determining LVH by ECG, we observed an increase in sensitivity to 60.9% but a decrease in specificity to 85.2%.
India has a dual burden of high rates of cardiovascular disease and barriers in access of diagnostic centres and referral protocols [17]. Socio-economic disparities exist in our health care response in both public and private health facilities and policy efforts have been suggested to improve these disparities at the health system level [18]. In a country like India, where the disease burden of hypertension is overwhelming, it is important to decide which patients are to be evaluated for LVH. Prevalence of hypertension in India according to the recent NPCDCS study is 15.95%, with and incidence of 3.7% [19]. It is projected that by 2025, the number of hypertensive individuals in India will be over 214 million [20]. It is not feasible to subject all hypertensive patients to echocardiography to detect LVH. If ECGs were to be efficiently utilised at the primary health centres to identify LVH, only those patients could be referred at a higher centre for evaluation.
Conclusion
Both Romhilt-Estes and Sokolow-Lyon ECG criteria are inadequate as screening tools due to lower sensitivity. But during routine screening of hypertensive patients, if any patient is positive by Romhilt-Estes criteria, he/she would require further evaluation by echocardiography or referral to a centre with such facilities. Although echocardiography cannot be recommended to evaluate every patient with hypertension in a country like India, initial evaluation using ECG can certainly help in selecting those needing echocardiographic evaluation.
Limitations of The Study
1. Small sample size of 50 patients.
2. Advanced imaging modalities could not be used to compare the efficacy of ECG in this study as they were expensive and time-consuming.
Recommendations
1. In a rural primary health centre with limited resources and infrastructure, ECG is a cheap and easily available tool to identify LVH with good specificity and positive predictive value.
2. All hypertensive patients should undergo a screening ECG for LVH as early detection and intervention could prevent or delay further complications, morbidity and mortality.