Prevalence of Invasive Aspergillosis Among (PTB) Patients in Kanchipuram, India
Sivasankari S1, Senthamarai S2, Anitha C3, Apurba Sankar Sastry4, Sandhya Bhatt5, Kumudhavathi M.S6, Amshavathani S.K7
1Assistant Professor, Department of Microbiology, Meenakshi Medical College and Research Institute, Enathur, Kachipuram, Tamil Nadu, India.
2Assistant Professor, Department of Microbiology, Meenakshi Medical College and Research Institute, Enathur, Kachipuram, Tamil Nadu, India.
3Assistant Professor, Department of Microbiology, Meenakshi Medical College and Research Institute, Enathur, Kachipuram, Tamil Nadu, India.
4Assistant Professor, Department of Microbiology, JIPMER, Pondicherry, Tamil Nadu, India.
5Assistant Professor, Department of Microbiology, PIMS, Pondicherry, Tamil Nadu, India.
6Tutor, Department of Microbiology, Meenakshi Medical College and Research Institute, Enathur, Kachipuram, Tamil Nadu, India.
7Professor & HOD, Department of Microbiology, Meenakshi Medical College and Research Institute, Enathur, Kachipuram, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sivasankari S., Assistant Professor, Department of Microbiology, Meenakshi Medical College and Research Institute, Enathur, Kachipuram, Tamil Nadu, India.
Phone: (0)9444145904,
E-mail: murugansivasankari1@gmail.com
Background: Tuberculosis (TB) remains a major health problem worldwide. (PTB) is commonly associated with secondary aspergilloma. Repeated exposure of Aspergillus spores can aggravate the bronchial pathology and can manifest as asthmatic episodes.
Aim and Objective: Pulmonary invasive aspergillosis is difficult to evaluate. Culture based diagnosis is time consuming. Hence (PCR) was done to evaluate the invasive fungal aspergillosis in (PTB) patients.
Materials and Methods: Eighty sputum samples collected from TB patients were processed as per standard protocol. Species level identification was done using PCR.
Results: Among 80 patients, 26 isolates were obtained, only 8 were Aspergillus species. All Aspergillus were taken up for PCR evaluation.
Conclusion: Fungal infection should be suspected in all sputum positive patients. PCR is an effective tool to diagnose invasive aspergillosis.
Aspergillus, PulmonaryTuberculosis, Polymerase chain reaction
Introduction
TB remains a health problem worldwide [1]. The lungs are primarily involved but the infections also occur in other organs [2]. The load of opportunistic infections have increased tremendously due to increase in immunocompromised conditions of host [3]. Fungal infections are becoming more frequent because of expansion of high risk population and use of treatment modalities that prolong the survival of these patients. (PTB) is the most commonly associated disease in cases of secondary aspergilloma [4]. The reason for increased prevalence of disease is the inefficiency of immune system and the use of Antituberculosis Treatment (ATT), which promote growth and reproduction of fungal flora and in turn aggravate the underlying pathology [5].
Invasive aspergillosis infections may manifest in several different forms, but more common in bronchopneumonia [4]. The opportunistic fungi cause disease in immunocompromised patients with pre-existing disease and with long history of antibiotics. In the world more than a million people develop Chronic Pulmonary Aspergillosis (CPA) while having retreatment for TB [6].
The spores are released in large numbers ambient air, remain airborne for many hours and they are inhaled by humans [6]. Aspergillus finds a comfortable abode in damaged or scarred pulmonary tissue like pre existing cavities or bronchiectatic areas. Mycelia grows inside the cavity and forms ball like mass, without invading into viable tissue or blood vessels, the predisposing cause may range from TB, sarcoidosis, cavities in rheumatoid lung etc [7]. The pathologic reaction in human beings varies from simple colonization, allergic alveolitis, aspergilloma and invasive aspergillosis [8-10]. Repeated exposure of Aspergillus spore can precipitate and aggravate this immune mediated bronchial pathology and can manifest as asthmatic episodes [10]. The present study was carried out to assess the prevalence of invasive aspergillosis among (PTB). Culture based diagnosis of aspergillosis infection is time consuming and often has diagnostic sensitivity. The Galactomannan assay is to detect pathogens from Aspergillus genus but is susceptible to false positive result due to cross reactivity. PCR is the potential tool for diagnosis of Aspergillosis. Hence this study was taken up to find the prevalence of fungal infection among TB patients and also confirm the species of fungi by PCR.
Materials and Methods
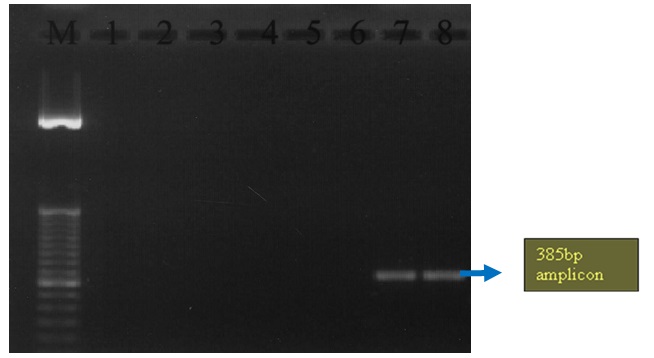
This study was done at Meenakshi Medical College Hospital and Research Institute Kanchipuram, Chennai - Bangalore, India, from Jan 2012 to Dec 2012. Study was approved by Institutional Ethical Committee. Informed written consent was obtained from all the study and control groups. The study group includes 80 sputum samples that were positive for pulmonary TB as per Revised National TB Control Programme protocol. 20 patients without TB were taken as control group and sputum samples were collected. Direct smear was done with 10% potassium hydroxide, Lacto Phenol Cotton Blue (LPCB) mount for identifying the fungus and culture on Saburoudes dextrose agar. All samples were processed and identified according to standard protocol. Growth was confirmed by repeated isolation for atleast 3 times. The species level identification was done. All Aspergillus were taken up for PCR. Universal primer and spices specific primer were used. After amplifications the amplicons were visualized on 1.5 % agarose gel for presence of band and the gels were scanned under UV illumination, visualized, and digitized with the Gel Doc documentation system.
Result
Out of 80 (PTB) sputum collected only 26 (32.50%) isolates were grown from 24 patients. All 24 patients showed smear and culture positive. Smear and culture were negative for control group [Table/Fig-1]. Among the 26 isolates only 8 (30.76%) were found to be Aspergillus spp [Table/Fig-2]. All the Aspergillus were taken up for PCR using species specific primer. The Aspergillus was amplified at 385 bp [Table/Fig-3,4]. No fungus was isolated from control group.
Showing the fungal growth in study and control group
| Type of patients | Total number of cases | Number of fungal isolates | Percentage |
| Study group | 80 | 26 | 32.50% |
| Control group | 20 | 0 | 0 |
Showing the fungal growth in study and control group
| Number of fungal isolates | Number and percentage of Aspergillus spp. | Distribution of Aspergillus spp. | Number and percentage |
| 26 | 8 (30.76%) | Aspergillus fumigatus | 2 (25%) |
| Aspergillus flavus | 3 (37.5%) |
| Aspergillus niger | 3 (37.5%) |
aGt e7l2 pºcic ftourr e1 5o fm PinCR showing amplification of Aspergillus fumigatus
| Aspergillus fumigatus | Sequence | Product size (bp) |
| AFUMI | CGC CGA AGA CCC CAA CAT GAA CGC | ˜385 |
| AFUM2 | TAA AGT TGG GTG TCG GCT GGC | ˜385 |
| Initial denaturation at 96ºc for 5 minutes |
| 40 cycles | Denaturation at 94ºc for 30 seconds |
| Primer annealing at 58ºc for 30 seconds |
| Extension at 72ºc for 30 seconds |
Aspergillus fumigatus was confirmed by PCR
Discussion
The prevalence of PTB with fungal co-infection is well documented in late 1960s.Treated PTB can lead to progressive loss of pulmonary function and chronic Aspergillosis [11]. CPA is a sequale and is a differential diagnosis of smear negative PTB after successful ATT [12]. In our present study the percentage of mycotic infection in (PTB) patients was 30.8%, which is comparable with the study of Sunita and Mahendra [3]. Tejal Patel et al., [13] found that Aspergillus is the most common invasive fungal infection in humans. Our study is concordant with the above study that Aspergillus is common isolates. Sunita and Mahendra [3] isolated 46% of Aspergillus from TB patients. In our study we had isolated 30.7% of Aspergillus. Current diagnostic methods such as culture, biopsy and serology lack rapidity and efficiency. PCR has potential to improve fungal diagnosis as it is faster, more sensitive and specific [14]. Guizhen Luo et al., [15] did a multiplex PCR evaluation of fungal colonies and it provided 100% sensitivity. In their study they could amplify only one half of molds directly from mycelia fragments. In our study, among the 8 Aspergillus species, only 2 Aspergillus fumigatus were amplified and in addition we describe the use of whole hyphal cells as template for PCR. Omission of DNA extraction procedure significantly decreases the time required to make an accurate identification by PCR. In our study also only 2 Aspergillus fumigatus were amplified from mycelial fragments. Diagnosis using culture is time consuming and limitations in diagnostic sensitivity. Serology like β-D glucon is non-specific because it is found in many fungal cell walls such as Fusarium, Acremonium species [16]. For diagnosing invasive aspergillosis Galactomannan assay has a sensitivity of 71% and specificity of 80% [17]. False positive and false negative values are common in Galactomannan assay because of certain antibiotics, histoplasma fungal infection and even certain foods can increase values of galactommanan assay [18] PCR can be used as a tool to detect invasive aspergillosis. Lack of standardization has limited its acceptance as a diagnostic tool and preventing its inclusions in disease forming criteria[19].
Conclusion
Diagnosis of opportunistic respiratory fungal infections poses a difficult diagnostic challenge due to lack of any pathognomonic clinical syndromes. Our opinion is to suspect fungal infection in all sputum positive patients. Fungal screening is highly recommended as routine investigation in microbiology for all cases of TB for aspergillosis to start antifungal therapy at the right time. PCR is a useful tool to diagnose the invasive aspergillosis and can guide for antifungal therapy.
Abbreviation
ATT-Antituberculosis treatment, PTB- (PTB), PCR- Polymerase chain reaction , IA-Invasive aspergillosis.
[1]. Ganguly D, Tuberculosis – triumphs and tragediesJ. Indian. Assoc 2000 14:96-8. [Google Scholar]
[2]. Mukerji K, Jain D, Agarwal SK, Prasad R, A study on anaerobic infections in patients of (PTB)Indian J Tuberculosis 1989 36:171-5. [Google Scholar]
[3]. Bansod S, Rai M, Emerging of mycotic infection in patients infected with Mycobacterium tuberculosis.World Journal of Medical Sciences 2008 3(2):74-80. [Google Scholar]
[4]. Reichenberger F, Habicht J, Matt P, Diagnostic yield of bronchoscopy in histologically proven invasive pulmonary aspergillosisBone Marrow Transplant 1999 24:1195-9. [Google Scholar]
[5]. Wheat LJ, Hackett E, Durkin M, Histoplasmosis-associated cross-reactivity in the BioRad Platelia Aspergillus enzyme immunoassay.Clin. Vaccine Immunol 2007 14:638-40. [Google Scholar]
[6]. Patterson FT, Advances & challenges in management of invasive mycosisLancet. 2015 366:1013-25. [Google Scholar]
[7]. Research Committee of British Thoracic and Tuberculosis Asso. Aspergillosis and Residual Tuberculous cavities -The Result of Survey.Tubercle. 1970 50:227-45. [Google Scholar]
[8]. Fraser RS, Pare JAP, Eraser RG, Pare PD, In: Infectious Diseases of Lungs in Synopsis of Diseases of Chest 1994 2nd EditionPhiladelphiaWB Saunders & Co:332-54. [Google Scholar]
[9]. Davies SF, Saros GA, In: Fungal Infection in Murray JG, Nadel JA, edit Text Book of Respiratory Medicine. 1994 PhiladelphiaWBSaunders Co.:1161-70. [Google Scholar]
[10]. Hinson KFW, Moon AJ, Plumme NS, Broncho Pulmonary Aspergillosis: A Review and Report of Eight New CasesThorax. 1952 7:317-33. [Google Scholar]
[11]. Denning DW, Latge JP, Steinbach WJ, Aspergillus fumigatus and aspergillosis 2009 WashingtonASM Press [Google Scholar]
[12]. Nam HS, Jeon K, Um SW, Suh GY, Chung MP, Kim H, Clinical Characteristics and treatment outcome of chronic necrotizing Pulmonary Aspergillosis; A Review of 43 casesInt J Inf.Dis 2010 14:479-82. [Google Scholar]
[13]. Patel T, Clifton IJ, Kastelik JA, Packam DG, Concurrent pulmonary zygomycosis and Mycobacterium infection.Journal of medical case reports. 2007 :1-7. [Google Scholar]
[14]. Kourkoumpetis TK, Fuchs BB, Colomanjj , Desalermoss A, Mylonakis E, Polymerase Chain reaction based assay for detection of Invasive fungal infections.Clin Infect Dis 2012 54(9):1322-31. [Google Scholar]
[15]. Luo G, Mitchell TG, Rapid identification of pathogenic fungi directly from cultures by using multiplex PCR.J. Clin. Microbiol 2002 40(8):2860-5. [Google Scholar]
[16]. Karageorgopoulos DE, Vouloumanou EK, Ntzirora F, Michalopoulos A, Rafailidis PI, PI.Beta D glucan assay for diagnosis of invasive fungal infections;a meta analysisClin Infect Dis 2011 52:750-70. [Google Scholar]
[17]. Walsh TJ, Shoham S, Petraitiene R, Detection of galactomannan antigenemia in patients receiving Pipercillin –Tazobactum and correlation between in vitro,in vivo and clinical properties of drug antigen interaction.J Clin Microb. 2004 42:4744-8. [Google Scholar]
[18]. Boonsarngsuk V, Niyompattama A, Teosirimongkol C, Sriwanichrak K, False positive serum and broncheoalveolar lavage Aspergillus galactomannaan assay caused by different antibiotics.Scand J Inf Dis. 2010 42:461-8. [Google Scholar]
[19]. White PL, Bretagne S, Klingspor L, Melchers JG, Mccolloch E, Schulz B, B. Aspergillus PCR; one step closer to standardizationJournal of Clinical Microbiology. 2010Ap 48(4):1231-40. [Google Scholar]