Introduction: Chronic Obstructive Pulmonary Disease (COPD) has considerable effects on cardiac functions primarily affecting the pulmonary vasculature and then right ventricle along with left ventricle. One of the important causes of increased morbidity and mortality associated with COPD is cor pulmonale. Echocardiography provides a rapid, non-invasive method to evaluate cardiac changes. Our aim was to evaluate RVfunction in COPD as per guidelines of American Society of Echocardiography with an aim to find a simpler way of predicting cardiac morbidity.
Materials and Methods: A cross sectional observational study was conducted on 17 COPD patients attending Respiratory Medicine outdoor of R. G. KAR Medical College, Kolkata, India, through history taking, clinical examination, PFT (PFT) and Echocardiography. Statistical analysis was done by using Statistical Package for the Social Sciences (SPSS) version-17.
Results: Fractional area change of RV (FAC-%) was positively correlated with Forced Expiratory Volume in One Second (FEV1) (r = 0.4879), FEV1/ Forced Vital Capacity (FVC) ratio (r = 0.5048) and Peak Expiratory Flow Rate (PEFR) (r = 0.5361). There was strong negative correlation of Systolic Pulmonary Artery Pressure (SPAP) with FEV1/FVC ratio (r = -0.5553) and PEFR (r = - 0.4604). Right Index of Myocardial Performance (RIMP) of right ventricle was negatively correlated with FEV1/FVC ratio (r = - 0.598), PEFR (r = - 0.619), Forced Expiratory Flow (FEF) 25-75 (r = -0.515). Tricuspid annular plane systolic excursion (TAPSE) did not show any association with PFT parameters though it showed strong positive correlation with RV wall thickness.
Conclusion: This study substantiates that FAC% and RIMP can be vital prognostic factors for RV function apart from SPAP, TAPSE to define RV dysfunction and predict morbidity in COPD.
Introduction
(COPD) has been defined by the Global Initiative for Chronic Obstructive Lung Disease (GOLD) as a disease state characterized by airflow limitation which is not fully reversible [1]. Measurement of lung function is the key test necessary for diagnosis of COPD but individually it is not sufficient to predict the morbidity.
COPD is a disease of increasing public health importance around the world. GOLD estimates suggest that COPD will rise from the sixth to the third most common cause of death worldwide by 2020. Presently, COPD is the fourth leading cause of death and affects >16 million people in the United States [2].
COPD is associated with significant extra-pulmonary (systemic) effects among which cardiac complications are most common. Cardiovascular disease accounts for approximately 50% of all hospitalization and nearly one-third of all deaths in cases where (FEV1) is 50% of predicted [3]. So, a timely prediction about the cardiac involvement is of immense importance.
COPD affects primarily the right side of heart and echocardiography provides a rapid, non-invasive and accurate method to evaluate the RVfunctions along with left ventricular function [3].
The purpose of our study was to evaluate the RV functions in patients of different stages of COPD by echocardiography as per guidelines of American Society of Echocardiography [4] with an aim to find a simple way of predicting cardiac morbidity in COPD.
Material and Methods
A cross-sectional observational study was conducted on 17 COPD patients (age >-40 years, all male) for six months. First, the diagnosis of COPD was confirmed and evaluated for staging; by history, clinical examination, and PFT (according to GOLD criteria) in the Department of Physiology and Respiratory Medicine of RGKMCH, SectionKolkata, India. Subsequently, all the patients have undergone echocardiography in the Department of Cardiology of RGKMCH with special emphasis on the function of the right heart. Patients with other cardiac or respiratory problems (like bronchial asthma, Pulmonary Tuberculosis (TB), lung malignancy, lung fibrosis, heart failure, myocardial infarction); very poor echo window and who were unable to perform PFTs were excluded from this study.
All the patients gave their informed consent prior to inclusion in the study and the study protocol was approved by the ethics committee of RGKMCH.
All the patients were investigated by spirometry with electronic spirometer (model: Recorders and Medicare systems [RMS] Helios 702). The PFTs parameters included were FEV1, FVC, FEV1/FVC ratio, PEFR, FEF25-75 [5,6]. The results of the PFTs were recorded in percent of predicted values.
All the patients were subjected to echocardiography using model: ACUSON CV 70, SIEMENS, Equip ID: 1006730741.
The echocardiography parameters were RV basal, mid-level and apical diameter, RV wall thickness, right atrial major and minor dimensions, TAPSE, RIMP, FAC%, SPAP [4].
All data collected were analyzed by SPSS version-17 for mean, SD and Pearson Correlation Test.
Results
Seventeen patients were recruited in our study according to the inclusion and exclusion criteria.
The demographic profile, PFT, spo2 (oxygen saturation by pulse oximetry) and RV function test data were given in terms of mean±SD in [Table/Fig-1].
All the PFT parameters were below normal limit. RV parameters and SpO2 were within normal limit except RV wall thickness which was increased suggesting RVH without dilatation.
Correlation of PFT parameters with echocardiographic parameters were presented in[Table/Fig-2] along with scatter diagram.
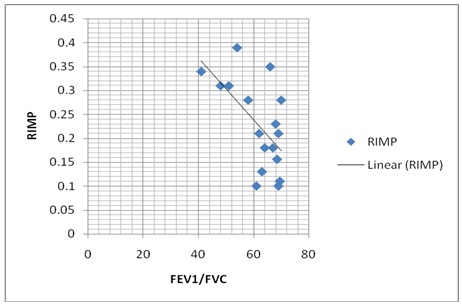
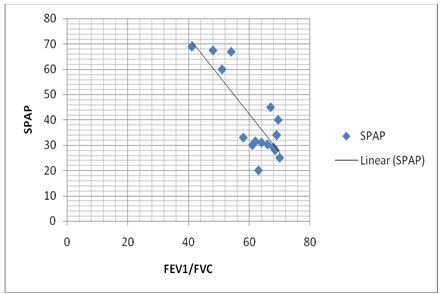
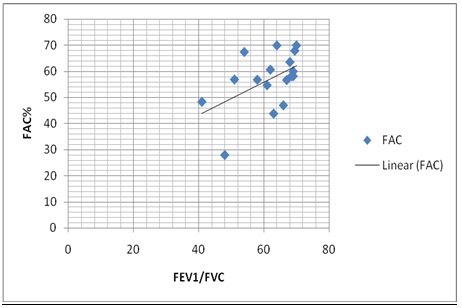
Fractional area change of RV (FAC-%) was positively correlated with Forced Expiratory Volume in One Second (FEV1) (r = 0.4879), FEV1/ Forced Vital Capacity (FVC) ratio (r = 0.5048) and Peak Expiratory Flow Rate (PEFR) (r = 0.5361). There was strong negative correlation of Systolic Pulmonary Artery Pressure (SPAP) with FEV1/FVC ratio (r = -0.5553) and PEFR (r = - 0.4604). Right Index of Myocardial Performance (RIMP) of right ventricle was negatively correlated with FEV1/FVC ratio (r = - 0.598), PEFR (r = - 0.619), Forced Expiratory Flow (FEF) 25-75 (r = -0.515)
The demographics, PFTs and right ventricular function tests data are given Abbreviations: FAC%- Fractional Area Change, RIMP- Right Index of Myocardial Performance, SPAP- Systolic Pulmonary Artery Pressure, TAPSE- Tricuspid Annular Plane Systolic Excursion
| Total No. of Patients(n) | 17 |
| Male | 17 |
| Female | 0 |
| Age (in years) | 56.294±10.294 |
| BMI(kg/m2) | 19.958±4.427 |
| FEV1(% of predicted) | 42.823±12.511 |
| FEV1/FVC (% of predicted) | 61.705±8.587 |
| PEFR(% of predicted) | 22.323±6.961 |
| FEF25-75%(% of predicted) | 16.058±6.279 |
| FAC (%) | 56.888±10.657 |
| SPAP | 35.488±10.993 |
| RIMP | 0.227±0.093 |
| TAPSE | 27.005±7.231 |
| RV basal diameter | 35.194±9.184 |
| RV mid-level diameter | 25.112±8.355 |
| RV apical diameter | 8.929±3.361 |
| RV wall thickness | 7.069±1.172 |
| RA major dimension | 37.8±7.757 |
| RA minor dimension | 35.558±9.233 |
| SpO2 | 96.266±1.486 |
Shows strong positive correlation between FAC% and FEV1 (r = 0.4879), FEV1/FVC ratio (r = 0.5048) and PEFR (r = 0.5361) but not with FEF25-75 (r = 0.3745) and strong negative correlation between SPAP and FEV1/FVC ratio (r = -0.5553), PEFR(r = -0.4604),) but not with FEF25-75 (r = -0.3511) and FEV1 (r = -0.2917). There is also strong negative correlation between RIMP and FEV1/FVC ratio (r = -0.598) PEFR (r = -0.619), FEF25-75 (r = -0.515) but not with FEV1 (r = -0.336)
| Correlation of PFT Parameters W ith Echocardiographic parameters | P earson Correlation Coefficient (r) |
| FEV1 | FEV1/FVC | P EFR | FEF25-75 |
| FAC% | 0.4879 | 0.5048 | 0.5361 | 0.3745 |
| SPAP | -0.2917 | -0.5553 | -0.4604 | -0.3511 |
| RIMP | -0.336 | -0.598 | -0.619 | -0.515 |
Shows strong negative correlation between RIMP and FEV1/FVC ratio (r = -0.598)
Shows strong negative correlation between SPAP and FEV1/FVC ratio (r = 0.5553)
Shows strong positive correlation between FAC% and FEV1/FVC ratio (r = 0.5048)
Discussion
COPD is associated with significant extra-pulmonary effects among which cardiac complications are most common. The cardiac manifestations of COPD are numerous. Impairment of RV function and alteration of pulmonary blood vessels are well known to complicate the clinical course of COPD and correlate inversely with survival [3].
So far the echocardiographic parameters are concerned; MPI (Myocardial performance index) is well correlated with tricuspid regurgitation which is a manifestation of dilated right ventricle [7]. The index reflects RV impairment and the severity of impairment is proportional to the velocity of tricuspid regurgitation [8]. Other Workers measured MPI as Tei index which combines both diastolic and systolic parameters to assess global RV function [9-12].
We studied MPI by taking RIMP as RV performance indicator found similar changes as in other studies [8,10-12]. Furthermore, RIMP showed a strong negative correlation with PFT parameters except FEV1 [Table/Fig-2,3].
Gupta et al., showed that prevalence of Pulmonary Arterial Hypertension (PAH) has a linear relationship with severity of COPD and severe PAH is usually associated with cor pulmonale [3]. PAH is well correlated with severity of COPD in many other studies [13,14]. But resting patients of moderate COPD with oxygen saturation > 90% [15] and pao2 > 60 mm Hg [16-18] do not show pulmonary hypertension.
In our study, oxygen saturation was found to be within normal limit in all patients [Table/Fig-1]. SPAP was estimated in our study, which showed strong negative correlation with FEV1/FVC ratio and PEFR [Table/Fig-2,4] but SPAP in most of our patients (64.7%) was within normal limit.
Measurement of ejection fraction is another important criterion to define morbidity and also an important predictor of exercise capacity, mortality, etc. [19-21]. But a proper measurement requires sophisticated method like angiography, radionuclide techniques using equilibrium angiography, thermo dilution in right heart catheterization, first pass radionuclide scan by (multiple-gated acquisition) MUGA etc [19,20,22]. FAC% correlates with Right Ventricular Ejection Fraction (RVEF) measured by Magnetic Resonance Imaging MRI also [23,24].
In our study, FAC% was measured; it was used as a guide for assessing ejection fraction and was found to correlate positively with all PFT parameters except FEF25-75 [Table/Fig-2,5].
In present study, the RV diameters, wall thickness and RA dimensions were measured as per guidelines of American Society of Echocardiography (ASE) [4] [Table/Fig-1]. It shows increased RV wall thickness suggesting RVH but RV and RA dimensions were within normal limit suggesting no dilatation [Table/Fig-1]. These results showed similar changes as in other studies [16]. TAPSE was also measured in our study but it did not show any association with PFT parameters, but it showed strong positive correlation with RV wall thickness.
Conclusion
This study substantiates that FAC% and RIMP can be vital prognostic factors for RV function apart from SPAP and, TAPSE. Our study may be helpful to define RV dysfunction in COPD and predict cardiac morbidity in a very simple manner which will help in modification of treatment strategies in COPD. However, the study population was small and further studies with larger number of subjects with multicentric design are required for confirmation.
Future scope: Simple echocardiography as per recommendation of ASE seems to be a satisfactory tool to find out the cardiac involvement in COPD before undertaking any invasive and sophisticated methods like Modified Discrete Cosine Transform MDCT, MRI, first pass radionuclide scan, strain rate imaging, etc. in our set up and can be helpful in management of cardiac complications, treatment modification and timely intervention so that cardiac morbidity as well as mortality associated with COPD can be cut down.
[1]. Global initiative for chronic obstructive lung disease. Global strategy for the diagnosis, management and prevention of chronic obstructive lung disease. http://www.goldcopd.com/. [Google Scholar]
[2]. Reilly John J, Edwin Jr, Silverman K, Shapiro Steven D, Chronic obstructive pulmonary disease. In: Anthony S. Fauci, Eugene Braunwald, Dennis L. Kasper, Stephen L. Hauser, Dan L. Longo, J. Larry Jameson, Joseph Loscalzo. Harrison’s Principles of Internal Medicine 2008 217th EditionGraw Hill:1635-43. [Google Scholar]
[3]. NK Gupta, RK Agarwal, AB Srivastav, Echocardiographic evaluation of heart in chronic obstructive pulmonary disease patient and its co-relation with the severity of disease.Lung India. 2011 28(2):105-9. [Google Scholar]
[4]. Rudski Lawrence G, Lai Wyman W, Afalilo Jonathan, Guidelines for the echocardiographic assessment of the right heart in adults: A report from the American Society of EchocardiographyJ Am Soc Echocardiogr. 2010 23:685-713. [Google Scholar]
[5]. American Thoracic Society. Standardization of spirometry 1995 updateAm J Respire Crit Care Med 1995 152:1107-36. [Google Scholar]
[6]. Brusasco V, Crapo R, Series ‘ATS/ ERS Task Force’ Standardization of lung function testingEur Respire J 2005 26(5):319-38. [Google Scholar]
[7]. JC Grignola, F Gines, D Guzzo, Comparison of the Tei index with invasive measurements of RVfunctions.Int J Cardiol. 2006 113:25-33. [Google Scholar]
[8]. Grapsa Ioulia, Pavlopoulos Harry, Dawson David, Retrospective Study of Pulmonary Hypertensive Patients: Is RVMyocardial Performance Index a Vital Prognostic Factor?Hellenic J Cardiol. 2007 48:152-60. [Google Scholar]
[9]. C Tei, New non-invasive index for combined systolic and diastolic Ventricular functionJ Cardiol. 1995 26(2):135-36. [Google Scholar]
[10]. C Tei, KS Dujardin, DO Hodge, Doppler echocardiographic index for assessment of global RVfunction.J Am Soc Echocardiogr. 1996 9:838-47. [Google Scholar]
[11]. T Sugiura, S Suzuki, MH Hussein, Usefulness of a new Doppler index for assessing both ventricular function and pulmonary circulation in newborn piglet with hypoxic pulmonary hypertensionPediatr Res. 2003 53:927-32. [Google Scholar]
[12]. K Yasuoka, K Harada, M Toyono, Tei index determined by tissue Doppler imaging in patients with pulmonary regurgitation after repair of tetralogy of Fallot.Pediatr Cardiol. 2004 25:131-36. [Google Scholar]
[13]. Minai Omar A, Chaouat Ari, Adnot Serge, Pulmonary Hypertension in COPD: Epidemiology, Significance, and Management: Pulmonary Vascular Disease: The Global PerspectiveCHEST 2010 137(6):39S-51S. [Google Scholar]
[14]. Sims Michael W, Margolis David J, Localio Russell, Impact of Pulmonary Artery Pressure on Exercise Function in Severe COPDCHEST. 2009 136(2):412-19. [Google Scholar]
[15]. Levi-Valensi P, Weitzenblum E, Rida Z, Sleep-related oxygen desaturation and daytime pulmonary haemodynamics in COPD patientsERJ. 1992 5(3):301-7. [Google Scholar]
[16]. Vonk-Noordegraaf Anton, Tim Marcus J, Holverda Sebastiaan, Early Changes of Cardiac Structure and Function in COPD Patients with Mild Hypoxemia.CHEST. 2005 127:1898-1903. [Google Scholar]
[17]. M Oswald-Mammosser, M Apprill, P Bachez, Pulmonary hemodynamics in chronic obstructive pulmonary disease of the emphysematous type.Respiration. 1991 585(6):304-10. [Google Scholar]
[18]. CC Christensen, MS Ryg, A Edvardsen, Relationship between exercise desaturation and pulmonary haemodynamics in COPD patientsEur Respir J. 2004 244:580-86. [Google Scholar]
[19]. Y Juilliere, G Barbier, L Feldmann, Additional predictive Value of both left and RVejection fractions on long term survival in idiopathic dilated cardiomyopathy.Eur Heart J. 1997 18:276-80. [Google Scholar]
[20]. D Jain, B Zaret, Assessment of RVfunction: role of nuclear imaging techniques.Cardiol Clin. 1992 10:23-39. [Google Scholar]
[21]. Kjaergaard Jesper, Akkan Dilek, Iversen Kasper Karmark, RVdysfunction as an independent predictor of short- and long-term mortality in patients with heart failure.European Journal of Heart Failure 2007 9:610-16. [Google Scholar]
[22]. Gao Yan, DU Xiangying, Qin Wen, Assessment of the RVfunction in patients with chronic obstructive pulmonary disease using MRIActa Radiologica. 2011 52(7):711-5. [Google Scholar]
[23]. WW Lai, K Gauvreau, ES Rivera, Accuracy of guideline recommendations for two-dimensional quantification of the right ventricle by echocardiographyInt J Cardiovasc Imaging. 2008 24:691-8. [Google Scholar]
[24]. NS Anavekar, D Gerson, H Skali, Two-dimensional assessment of RVfunction: an echocardiographic-MRI correlative studyEchocardiography. 2007 24:452-6. [Google Scholar]