The solitary, nodular lesions of the oral mucosa present a diagnostic dilemma to the dentist with their analogous presentation. The lesions that appear on the tongue, a soft muscular organ are distinct and even rarer with varied manifestations. Oral mucosa presents lesions of the tongue in all age groups that may range from a small nodular swelling and ulcer formation in an infant of a few days old to an ulcer or a lesion in a 70-year-old. The reason for the appearance of an ulcer may be trauma to the soft tissues in an infant may be due to the presence of natal teeth to the presence of a sharp tooth in the older individuals. These lesions have to be clinically and histologically correlated for the final outcome of the diagnosis, so that there is no chance of any recurrence. We present a unique case of a solitary nodular lesion on the ventral surface of tongue On a 6 year female, where there was a recurrence after surgical excision and after an unusual therapy of non surgical resolution, no recurrence was observed.
Case Report
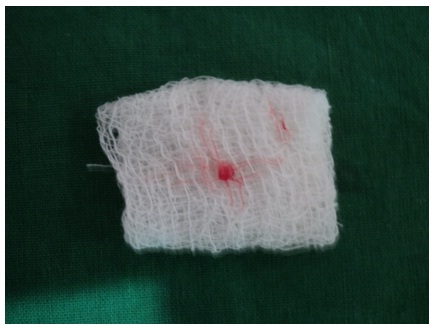
A 6-year-old female patient was referred to the Department of Pedodontics with a painless swelling of 4 days duration on the ventral surface of the tongue in the medial plane. There was no pain associated with the swelling. The parent and the patient could not recollect any history of trauma. The clinical appearance was that of a mucocele. On examination the swelling was of the same color as that of normal mucosa, soft in consistency, fluctuant and translucent measuring about 2mm x 2mm [Table/Fig-1].The differential diagnosis, included pyogenic granuloma,vascular lesions,lipoma,polyp and squamous papilloma. Since the child was cooperative it was decided to excise the lesion under local anesthesia [Table/Fig-2]. The mucocele was excised together with the minor salivary glands by dissection down to the muscle layer [Table/Fig-3]. The wound was left to heal by primary intention without suturing.
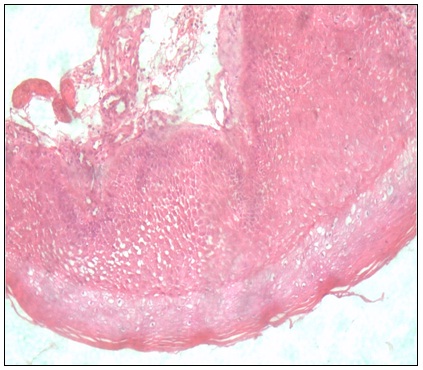
It is important that excision followed by anatomic-pathological examination be performed, to avoid having them misdiagnosed. The lesion was removed completely and all the fragments were sent for histopathological analysis. On histopathological examination, The H&E stained section showed parakeratinised stratified squamous epithelium, overlying the cystic lumen. The lumen consisted of inflammatory cell infiltrate in the form of foamy macrophages, leukocytes, plasma cells, and few blood vessels. Mucinophages that are faint and eosinophilic are observed. Salivary acini that consisted of serous and mucous acini were observed. Overall picture is suggestive of “Mucocele-Mucous Extravasation cyst” [Table/Fig-4]. After one week of surgical excision, patient seemed to be fine and after 15 day of follow-up, the patient reported with first recurrence [Table/Fig-5]. The lesion was of the same size as before. Since the patient was not willing for the second surgery an alternative method of management by non-surgical resolution was advised. The patient was advised to apply a highly potent topical corticosteroid clobetasol propionate 0.05% in the area of the lesion,and retain it for 2-3 minutes and spit it out ,it has to be repeated for three times a day . The patient was advised to use this treatment modality for one month after which she was asked to discontinue the usage and follow up after every week. After three weeks there was complete resolution of the mucocele. The patient has not reported second recurrence for six weeks. On follow-up of the patient after 18 months there was no recurrence of the lesion [Table/Fig-6].

Surgically excising the lesion, under Local Anaesthesia

Surgically excisised lesion
Surgically excisised lesion,histopathologically showing cystic lumen lined by parakeratinised stratified squamous epithelium with mucinophages and inflammatory infiltrate
Recurrence of the lesion after 4 weeks

Complete ressolution of the lesion after 18 months of recurrence

Discussion
The solitary, smooth, nodular submucosal lesions of the tongue can be clinically differentiated as schwannoma, neurofibroma, rhabdomyoma, lymphangioma,fibroma, lipoma, leiomyomas, inflammatory lesions such as fibro epithelial polyp and benign salivary gland tumors and mucocele. Three main groups of minor salivary glands are found in different locations of the human tongue. They are glands of Von Ebner, glands of Weber and the glands of Blandin and Nuhn. The glands of Blandin and Nuhn are mixed mucous and serous salivary glands that are embedded within the musculature of the anterior tongue ventrum [1].
The glands of Blandin and Nuhn are not lobulated or encapsulated. Each gland is approximately 8mm wide and 12 to 25 mm deep and consists of several small independent glands, composed of mucus tubules with seromucus demilunes and occasional seromucus acini. They drain by means of 5 or 6 small ducts that open near the lingual frenum.These glands extend laterally and posteriorly from the midline, forming a mass resembling a horseshoe with its opening pointing towards the root of the tongue [1].
Mucocele is a common benign lesion of the oral mucosa etymologically meaning a cavity filled with mucus (muco meaning mucus and coele meaning cavity), which is the secretory product of salivary glands. It is originated from the rupture of a salivary duct and extravazation of the mucin into the surrounding soft tissues [2].
Mucoceles on the tongue are rare and occur almost exclusively on the ventral surface where the glands of Blandin and Nuhn are located. If the mucocele is located directly under the mucosa(superficial mucocele), in the upper submucosa (classic mucocele) or in the lower corium (deep mucocele). The clinical presentation of these lesions depends upon their depth within the soft tissue and the degree of keratinization of the overlying mucosa superficial lesions present as raised soft tissue swelling that is translucent and having bluish color, while the deeper lesions are more nodular, lack the vesicular appearance and having normal mucosal color [2].
Sugerman et al., stated that the mucoceles of the Blandin and Nuhn glands are uncommon and clinically similar to the vascular lesions, pyogenic granulomas, polyp, and squamous papiloma,
Palpation can be helpful for a correct differential diagnosis. Lipomas and tumors of minor salivary glands present no fluctuation while cysts, mucoceles, abscess and hemangiomas do [2-3]. They are often found in young people, frequently associated with areas that are subject to traumas. The site with the higher incidence is the lower lip however, it can be found in any region where there are small salivary glands such as the tongue, buccal mucosa, upper lip, and palate [1-3] Mucoceles of the glands of Blandin and Nuhn have been considered to be uncommon [1,3,4].
According to Jinbu et al., and Mandel et al., Blandin and Nuhn mucoceles comprise 9.9% of all oral mucoceles studied by them [4-5]. Out of the 400 cases of mucocele reviewed by Harrison only nine cases were in the tongue [6].
In the Minnesota Oral Disease Prevalence Study, Blandin and Nuhn mucoceles had a lower prevalence than mucoceles at other locations, or 0.1 cases per 1000 persons with increased predilection for females. This type of mucocele represents an estimated 2-10% of all mucoceles [7]. Moraes et al., showed that, in their 6-year-period study, out of 312 cases of mucoceles 48 cases (15.4%) were diagnosed as mucocele of the glands of Blandin and Nuhn, the tongue being the second most frequent site of mucocele occurrence [8].
Occurrence of mucoceles on the dorsal surface of the tongue is not yet reported. Regarding superficial mucoceles, trauma does not always appear to play an important role in the pathogenesis. In many cases, mucosal inflammation that involves the minor gland duct results in blockage, dilatation, and rupture of the duct with subepithelial spillage of fluid. Changes in minor salivary gland function and composition of the saliva may contribute to their development. In some cases, an immunological reaction may be the cause
Histologically, mucoceles are classified as retention and extravasation types. Mucocele involving the glands of Blandin and Nuhn are often histologically diagnosed as being extravasation type and likely to occur in young patients. Mucoceles can easily traumatize and become a strong source of irritation and annoyance to the patient. Traumatic injury to a duct or ducts with partition of this structure is the most likely etiologic factor leading to the development of these lesions. These lesions are often asymptomatic, however, as they grow in size, they can cause discomfort, external swelling, and interfere with speech and mastication. Thus surgical excision is the treatment of choice. Usually, the surgical excision includes the servicing mucous glands with evacuation of its contents. According to surgerman et al., and Baurmash, the technique for managing moderate to large Blandin and Nuhn mucoceles is to completely unroof the lesion along its entire periphery to visualize and remove all of the glands present. Healing without complication or recurrence should follow [1,2,9].
In small mucocele cases, they are completely excised with primary closure and healing is rapid and uneventful. On the other hand, larger lesions may also be managed by marsupialization, [2] cryosurgery, [10], laser ablation, [11] and micro-marsupialization, [2].
Alternatives to surgery include steroid application such as corticosteroid clobetasol propionate 0.05%, [12] which we have used in our case and a method where the cystic cavity is filled with rubber impression material presurgically, to improve the visual access for surgical excision can be tried out [13].
Based on our experience, we recommend that mucoceles affecting the glands of Blandin and Nuhn should be removed up to the muscle plan, including the small glands found in the surgical field, to avoid recurrence. The glands of Blandin and Nuhn are not encapsulated and are directly overlapped to the muscle tissues; their manipulation tends to be different from the other oral mucoceles, besides they cannot be removed in toto like other mucoceles. When only marsupialization is performed, the lesion has every chance of recurrence as soon as the draining site is repaired [14].
Conclusion
This case report stresses the importance of both clinical and histopathological aspects in the diagnosis of Blandin and Nuhn Mucocele so that it may not be misdiagnosed.Different non-surgical methods of resolution can be tried out as treatment modalities. As clinicians, we should be prepared to encounter, different variants of mucoceles, whose occurrence is rare at various sites in the oral cavity.
[1]. PB Sugerman, MW Savage, WG Young, Mucocele of the anterior lingual salivary glands (glands of Blandin and Nuhn): report of 5 casesOral Surg Oral Med Oral Pathol Oral Radiol Endod 2000 90:478-82. [Google Scholar]
[2]. HD Baurmash, Mucoceles and ranulasJ Oral Maxillofac. Surg 2003 61:369-78. [Google Scholar]
[3]. ID Poker, C Hopper, Salivary extravasation cyst of the tongueBr J Oral Maxillofac Surg 1990 28:176-77. [Google Scholar]
[4]. Y Jinbu, M Kusama, H Itoh, K Matsumoto, J Wang, T Noguchi, T. Mucocele of the glands of Blandin and Nuhn: clinical and histopathologic analysis of 26 casesOral Surg Oral Med Oral Pathol Oral Radiol Endod 2000 95:476-70. [Google Scholar]
[5]. L Chander, A Kaynar, Mucocele of the gland of Blandin and NuhnN Y State Dent J 1992 58:40-41. [Google Scholar]
[6]. JD Harrison, Salivary mucocelesOral Surg Oral Med Oral Pathol 1975 39:268-78. [Google Scholar]
[7]. JE Bouquot, KKH Gundlach, Odd tongues: the prevalence of common tongue lesions in 23,616 white Americans over 35 years of ageQuint Intern 1987 17:719-30. [Google Scholar]
[8]. P De Camargo Moraes, M Bönecker, C Furuse, LA Thomaz, RG Teixeira, VC de Araújo, Mucocele of the gland of Blandin and Nuhn: histological and clinical findingsClin Oral Invest 2009 13:351-53. [Google Scholar]
[9]. HD Baurmash, Marsupialization for treatment of oral ranula: a second look at the procedureJ Oral Maxillofac Surg 1992 50:1274-79. [Google Scholar]
[10]. J Twetman, S Isaksson, Cryosurgical treatment of mucocele in childrenAm J Dent 1990 3:175-76. [Google Scholar]
[11]. WK Kopp, H St-Hilaire, Mucosal preservation in the treatment of mucocele with CO2 laserJ Oral Maxillofac. Surg 2004 62:1559-61. [Google Scholar]
[12]. JW Wilcox, JE History, Non-surgical resolution of mucocelesJ Oral Surg 1978 36:478 [Google Scholar]
[13]. AJ Rai, AM Hegde, YR Shetty, Management of Blandin and Nuhn mucocele’a case reportJ Clin Pediatr Dent 2008 32:147-49. [Google Scholar]
[14]. Adachi Patricia , Maria Ana, Soubhia Pires , Horikawa Fernando K., Shinohara Elio Hitoshi , Textbook of Medical MycologyJ Oral Maxillofac. Surg 2011 15:11-13. [Google Scholar]