Case Report
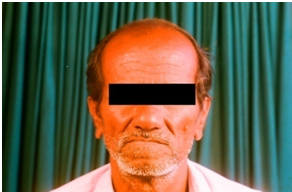
A 60-year-old male presented with a complaint of a slow growing, solitary, midline swelling in the region of chin, which had a duration of 5 years. There was a history of removal of lower front teeth, followed by trauma to the chin and discolouration of the lower front teeth. A single, oval, sub mental lymph node was palpable and it was nontender, firm in consistency and freely movable. Extra oral examination revealed obliteration of the mentolabial sulcus and slight fullness of the chin region [Table/Fig-1]. It had extended superiorly from vermillion border of the upper lip, inferiorly obliterated the mentolabial sulcus and mediolaterally 2 cm from the midline, i.e., upto the corner of the mouth. Skin over the swelling and skin surrounding the swelling appeared to be normal, with no local rise in temperature. The swelling was non-tender and no visible or palpable pulsations were encountered. Intraoral examination revealed a solitary, well-defined roughly oval swelling of size 5×4 cm in the anterior region of the mandible extending from the mesial aspect of 33 to the mesial aspect of 44, inferiorly obliterating the vestibule and superiorly upto the level of occlusion above the alveolar crest [Table/Fig-2]. The mucosa over the swelling and which surrounded the swelling appeared to be normal, with smooth surface texture. The swelling was non-tender, non-pulsatile and it showed cystic consistency. Teeth 31, 32, 41,42 and 43 were missing [Table/Fig-3]. Bilateral Angle’s class I molar relationship was observed and 44 appeared to be displaced mesioligullay. Although stains and calculi were present, there was no evidence of active periodontitis. 2 ml of straw coloured serosanguinous fluid was obtained upon aspiration and it showed the presence of cholesterol crystals. Radiograph of the mandibular anterior region showed a mixed radiolucent radiopaque lesion in the region of missing 31,32,41,42 and 43, extended from the mesial aspect of 33 to the mesial aspect of 44 [Table/Fig-4]. The lesion consisted of an oval radiolucency that was surrounded by a thin cortical line near the inferior aspect of the lesion with two discrete areas of calcifications within the radiolucency [Table/Fig-5]. The radiodensity of the calcifications was not similar to that of either enamel or dentin. Routine laboratory findings were within normal limits. Based on the above said findings, a provisional diagnosis of residual cyst with calcifications and differential diagnoses of other mixed radiolucent radiopaque lesions like traumatic bone cyst, focal cement-osseous dysplasia and periapical cement-osseous dysplasia (PCOD) were considered. Although, the common presentation patterns of these lesions, like location, site, gender, age distributions and radiographic appearances were specific, a histopathologic examination was done to establish a definitive diagnosis.
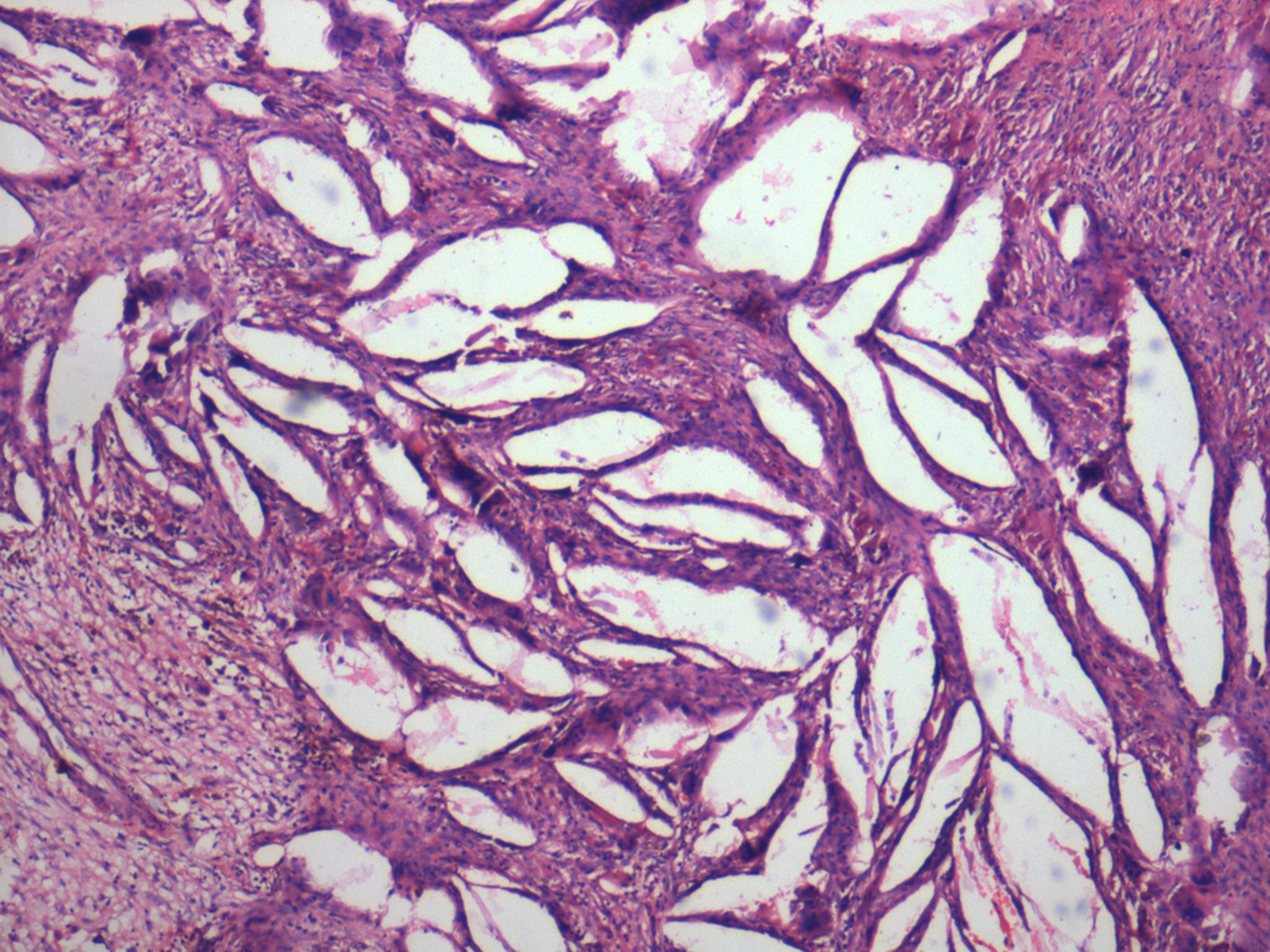
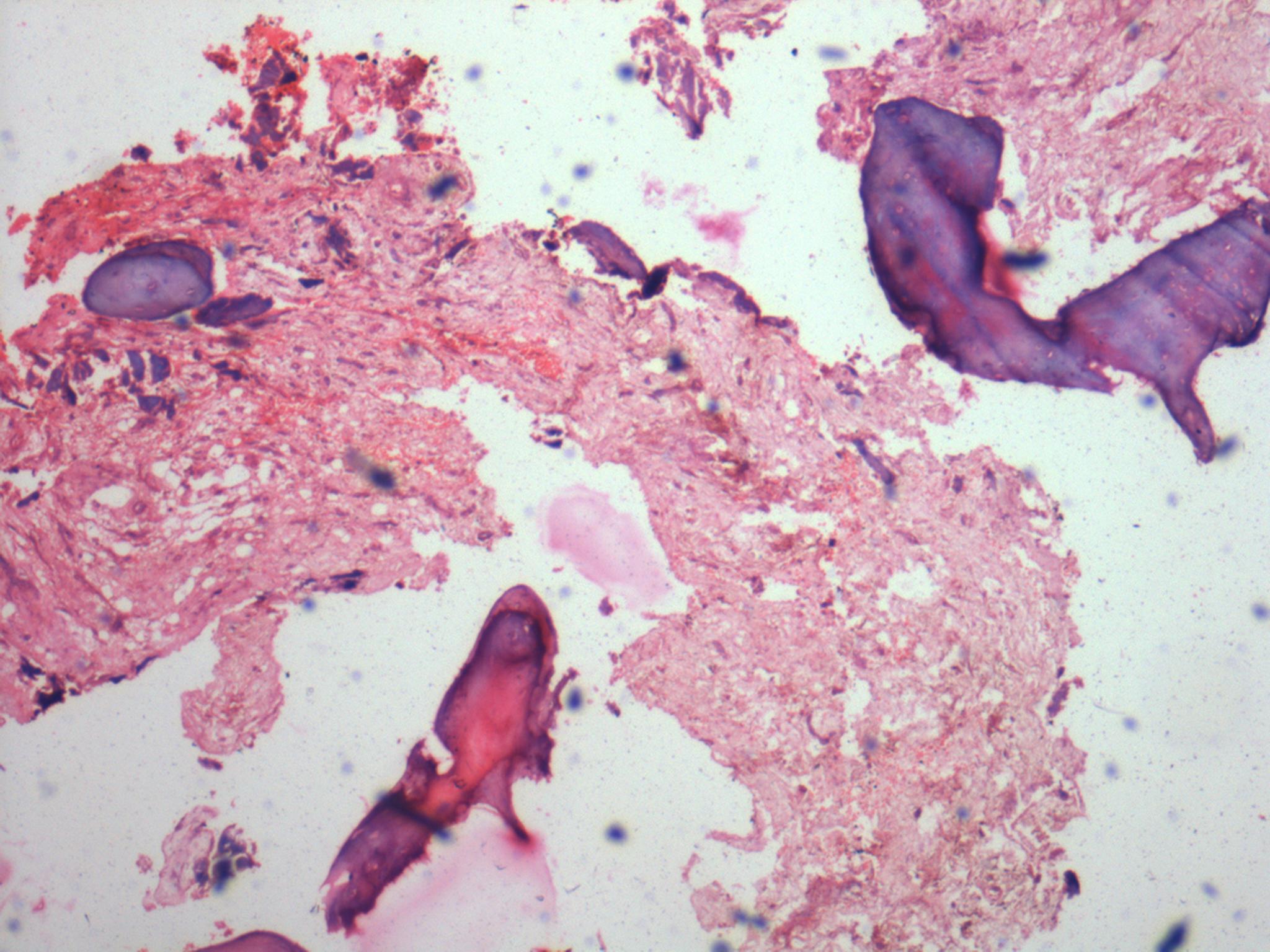
Patient was referred to the Department of Oral and Maxillofacial Surgery, where an incisional biopsy was performed after obtaining the informed consent of the patient. The histopathological examination revealed the presence of stratified squamous epithelial lining in an arcading pattern [Table/Fig-6]. The connective tissue wall showed inflammatory infiltrate with numerous cholesterol clefts [Table/Fig-7] and foci of dystrophic calcifications [Table/Fig-8].
The cyst was enucleated by using an intraoral approach under general anaesthesia. After enucleation and proper haemostasis, the surgical site was closed by using 3/0 vicryl. Histopathological examination of the excised specimen confirmed the diagnosis of residual dental cyst with dystrophic calcifications. No signs of recurrence was recorded over a period of 4 years.
Photograph showing the obliteration of mentolabial sulcus and slight fullness of the chin region
Photograph showing the extensions of the swelling

Photograph showing the intraoral aspect of the swelling and missing 31,32,41,42 and 43

IOPA of the mandibular anterior region depicting the mixed radiolucent radiopaque lesion and missing 31,32, 41, 42 and 43.
Radiograph depicting an oval radiolucent lesion with two discrete areas of calcifications within the radiolucency
Photomicrograph showing the stratified squamous epithelium lining arranged in arcading pattern
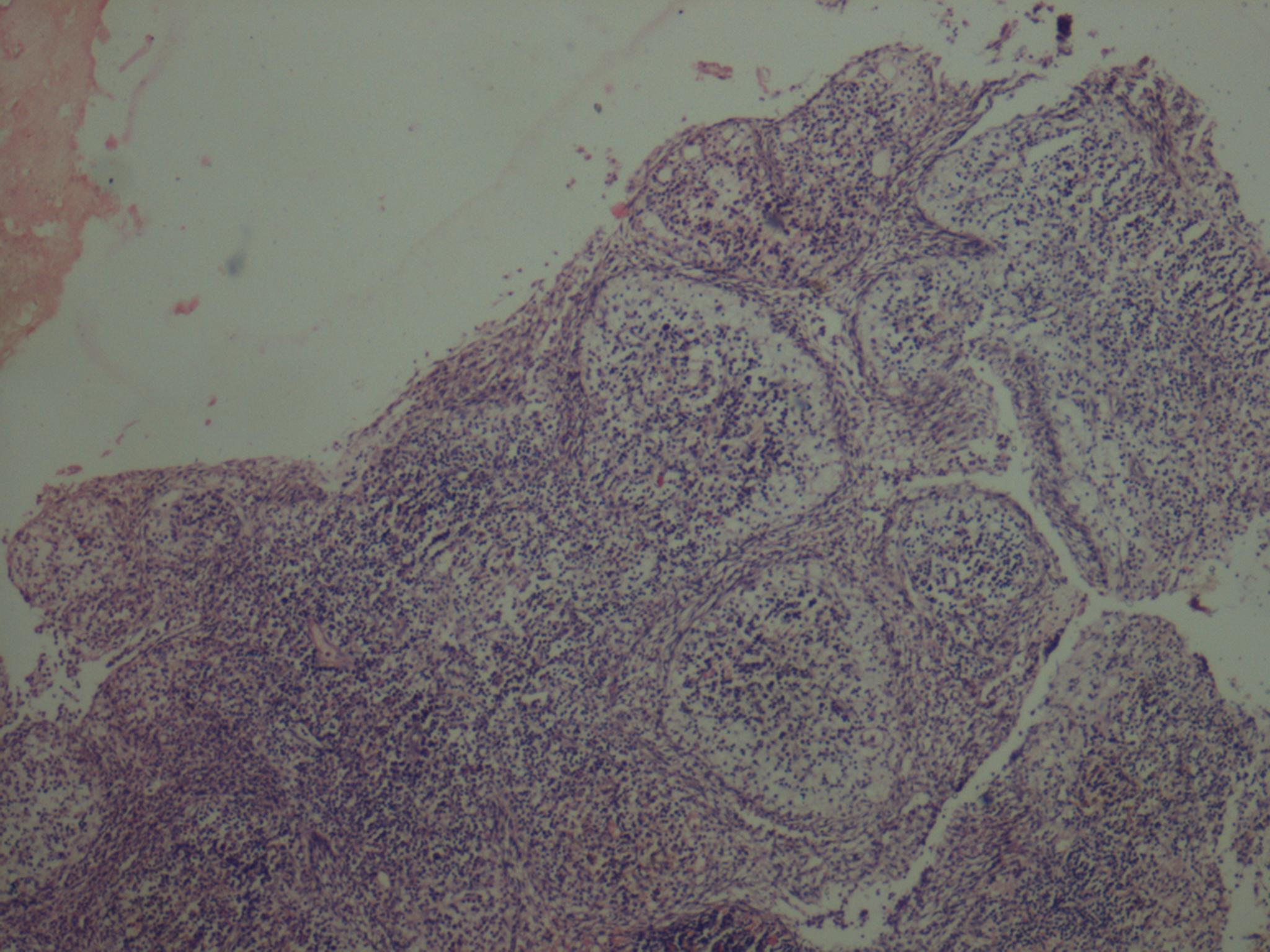
Photomicrograph depicting the inflammatory infiltrate with cholesterol clefts
Photomicrograph revealing foci of dystrophic calcifications
Discussion
Residual cysts are inflammatory cysts that are usually peri apical in position and persist after the removal of associated tooth. They represent approximately 10% of all odontogenic cysts and are usually asymptomatic [1,2]. Intrinsic calcifications present in the odontogenic cysts were first reported by Lovestadt and Bruce [3] and later by Browne et al., [4]. Calcifications in the residual cysts are quiet rare. However, Shafer et al., stated that the term, ‘residual cyst’ could be used for any cyst of the jaw, that remained following surgery.
According to previous reports [3-6] majority of the residual cysts are asymptomatic, they occur in the alveolar process and body of the jaw bones in edentulous areas, but may also be found in the lower ramus in patients who are over the age of twenty years, with the average age at the time of presentation being 52 years. Males are affected slightly more commonly than females, with a ratio of 3:2 and maxilla is more commonly involved than the mandible.
The case study reported here had presented with a slowly growing, painless swelling which had involved the anterior region of the mandible, who had a past history of extraction of the mandibular anteriors owing to the discolouration (non-vital), followed by trauma. The presence of cystic consistency (yielding with pressure) drove the authors to aspirate the lesion, that yielded a serosanguinous fluid with cholesterol crystals, without any evidence of blood and pus. Although a differential diagnosis of traumatic bone cyst could be considered at this stage, the same could be ruled out, as traumatic bone cysts usually occurr in patients under 25 years of age. Also, mandibular premolar and molar regions are frequently involved and aspiration is usually fruitless [7].
Radiographically, residual cyst appears as well-defined radiolucency, with a distinct sclerotic margin in edentulous area. The sclerotic margin may be fine, thin and it may be thicker and diffusely sclerotic. Occasionally, in cases of longstanding lesions and in lesions with chronic inflammation, calcified masses are seen, their appearances may vary from barely perceptible, fine grains of radiopacities, to large, irregular particles that rarely cross diameter of 0.5 cm [8]. The present case also showed similar radiographic appearance.
Dystrophic calcification refers to the precipitation of calcium salts at primary sites of chronic inflammation or in dead and dying tissues. This process is usually associated with a high local concentration of phosphatase, an increase in local alkalinity and anoxic conditions within the inactive or devitalized tissues [9]. A chronic, long standing cyst is a common location of dystrophic calcification, as was seen in our case. Dystrophic calcifications usually do not produce any signs or symptoms.
The case study reported here, showed the presence of cholesterol crystals in the cystic fluid, which was similar to that seen in previous reports. High et al., [9], in a histological and radiographic study done on age changes in the residual cysts, stated that there was a slow increase in the mineralized deposits within the cyst lumen, with time. This becomes prominent histochemically in those cysts that are more than 8-years-old and radiographically 6 years later. They also reported the presence of cholesterol crystals in residual cystic contents. The major sources of cholesterol could be attributed to disintegrating red blood cells which were in a form which readily got crystallized in the tissues, serum which had got accumulated in the tissues because of the relative inaccessibility of normal lymphatic drainage, degeneration and disintegration of lymphocytes, plasma cells, macrophages and circulating plasma lipids. Once cholesterol crystals get deposited in the fibrous capsules of the cysts, they behave as foreign bodies and excite a foreign body giant cell reaction. These crystals get dissolved out and clefts get surrounded by multinucleated giant cells. The cholesterol masses are extruded from the fibrous wall towards the path of least resistance, i.e., into the cyst cavity, as the external surface of the cyst may consist of dense fibrous tissue, bone and mucosa.
Although, traumatic bone cysts and odontogenic keratocysts are considered under differential diagnosis, when the residual cyst shows calcifications, like in our present case, one should differentiate the same from other localized mixed radiopaque-radiolucent lesions like odontomas, fractured root tips with secondary infections, intermediate stages of periapical cemento osseous dysplasia, adenomatoid odontogenic tumour and calcifying epithelial odontogenic tumour.
Odontomas are hamartomas composed of calcified structures of the enamel and dentine, as either amorphous conglomerations (complex odontomas) or rudimentary tooth like structures (compound odontomas), with radiodensities which are somewhat greater than that of the bone and usually not exceeding the diameters of the teeth present in the affected region. Odontomas are usually discovered either incidentally in young adults during routine radiographic examinations and during investigations of missing and displaced teeth [10]. Fractured root tips with secondary infections could be identified by the shape of root, along with the presence of root canal and lamina dura [11]. Periapical cemento osseous dysplasia (PCOD) predominantly involves the periapical region of the mandibular vital anterior teeth, with a marked female predilection between the ages of 30 and 50 years. Moreover, it is an asymptomatic condition that is discovered during routine radiographic examinations. When PCOD is observed in edentulous areas, the lesions tend to present as circular or ovoid radiolucencies with the central crescent shaped radiopaque mass [12].
Focal cemento osseous dysplasia is similar to PCOD, but it occurs commonly in the mandibular premolar region and appears as a localized, small radiolucency with central calcification [13] Adenomatoid odontogenic tumour is a slow growing tumour of the odontogenic epithelium, commonly seen in the maxillary anterior region, and is associated with an impacted tooth, especially canine tooth, with female predilection. Radiographically, the mixed radiolucent radiopaque stage appears as pericoronal cyst like radiolucency, with sharply defined radiopaque foci within the radiolucency [14].
The calcifying odontogenic cyst is a rare, slow growing, odontogenic, asymptomatic, solid and cystic lesion that occurs with equal frequency in the maxilla and mandible and with no gender predilection. Maxillary incisor-canine region is the most common site of involvement, whereas a considerable number of lesions are seen in the molar and premolar regions of the mandible. Although their radiographic appearance is like that of a cystlike radiolucency containing quite distinct radiopaque foci, half of the cases are associated with impacted teeth and root resorption [15].
Cacifying epithelial odontogenic tumour is a rare, benign, odontogenic neoplasm which affects the middle aged group, with equal gender predilection and mandible is commonly affected than the maxilla. Prevalence in the molar region is three times of that in the bicuspid region. Mixed radiolucent radiopaque stage appears as diffuse or well circumscribed radiolucency, along with combined pattern of radiolucency and radiopacity with many small, irregular bony trabeculae traversing the radiolucent area in many directions, producing a multilocular honey comb pattern. The scattered flecks of calcifications seen throughout the radiolucency, has given rise to the descriptive term of a ‘driven snow’ appearance. However, all these lesions are distinct histopathologically and aspiration is generally negative.
Residual cysts are slowly resolving lesions, but those that persist or increase in size are subjected to mechanisms which prolong the process. Due to the apparent thinness, the squamous epithelium lining the cyst can act as a semipermeable membrane and also continue to shed some cellular material into the lumen. Both these mechanisms could delay resolution [16].
Hstopathologic examination of the present case showed stratified squamous epithelium arranged in arcading pattern, lining the cystic space, in addition to slit like spaces which contained cholesterol clefts. The connective tissue wall showed foci of calcifications, similar to those reported earlier [5]. van der Waal et al., [17] reported the development of squamous cell carcinoma from three cases of residual cysts, in addition to the reported literature on the development of squamous cell carcinoma and mucoepidermoid carcinoma from the linings of other odontogenic cysts. The present case did not show any evidence of malignancy.
The treatment of choice for residual cysts is surgical enucleation, along with removal of the lining of the cyst. The rate of recurrence is low. However, a regular follow up is needed, to rule out malignant transformation and recurrence. In the present case, surgical enucleation was In the present case, surgical enucleation was done under general anaesthesia through intraoral approach and no signs of recurrence were observed for a period of 4 years.
Conclusion
Though not common, residual cysts with calcifications should be considered in the differential diagnosis of the swellings of the jaw bones which present as mixed radiolucent radiopaque lesions. A proper clinical, radiological, histopathological evaluation including aspiration must be done, to establish a definitive diagnosis and treatment should be planned accordingly for residual cysts. A regular follow-up protocol should be established after giving appropriate treatment, to rule out any recurrence and malignant transformation
[1]. DM Main, Epithelial jaw cysts: A clinicopathological reappraisalBr J Oral Maxillofac Surg 1990 8:114-25. [Google Scholar]
[2]. HC Killey, LW Kay, GR Seward, Benign cystic lesions of the jaws, their diagnosis and treatment 1977 3rd EditionEdinburghChurchill Livingstone:169 [Google Scholar]
[3]. SA Lovestadt, KW Bruce, Cysts of the incisive canal with concrementsJ Oral Surg 1954 12:48 [Google Scholar]
[4]. RM Browne, Sn Rowles, AJ Smith, Mineralized deposits in odontogenic cystsIRCS Med Sci. 1983 12:642 [Google Scholar]
[5]. C Krithika, S Kota, KS Gopal, H Koteeswaran, Mixed periapical lesion: Differential diagnosis of a caseJ Dentomaxillofac Radiol. 2011 40(3):191-94. [Google Scholar]
[6]. RL Cabrini, RE Barros, H Albano, Cysts of the jaws: A statistical analysis J Oral Surg 2003 28:485-89. [Google Scholar]
[7]. P Donkor, A Punnina Moorthy, Biochemical analysis of simple bone cyst fluid: report of a caseInt J Oral Maxillofac Surg 1994 23:291-97. [Google Scholar]
[8]. SC White, MJ Pharoah, Oral radiology – principles and interpretation (5th edn). St Louis: Mosby 2006 :597-98. [Google Scholar]
[9]. AS High, PN Hirschmann, Age changes in residual radicular cystsJ Oral Pathol 1986 15:524-28. [Google Scholar]
[10]. E Stavrou, KI Tosios, I Stavrou, Globular Opacity around the apex of an impacted third molarOral Surg Oral Med Oral Pathol Oral Radiol Oral Endod 2007 103:594-98. [Google Scholar]
[11]. BW Neville, DD Damm, CM Allen, JE Bouquo, Text Book of Oral and Maxillofacial Pathology, Chapter 14-Bone Pathology 2002 2nd Edition:553-571. [Google Scholar]
[12]. RP Langlais, OE Langland, CJ Nortje, Y Li, H Li, Diagnostic Imaging of the Jaws, Chapter 9-Circumscribed Radiolucencies - 2nd Edition:254-255. [Google Scholar]
[13]. DJ Summerlin, H Tomich, Focal cemento osseous dysplasia: a clinicopathologic study of 221 casesOral Surg 1994 78:611-20. [Google Scholar]
[14]. HP Philipsen, PA Reichart, K Zhang, al et, Adenomatoid odontogenic tumor: biologic profile based on 499 casesJ Oral Pathol Med. 1991 20:149-58. [Google Scholar]
[15]. T Nagao, T Nakajima, M Fukushima, al et, Calcifying epithelial odontogenic cyst: a survey of 23 cases in the Japanese literatureJ Maxillofac Surg 1983 11:174-79. [Google Scholar]
[16]. F Oehlers, Periapical lesions and residual dental cystsBr J Oral Maxillofac Surg. 1970 8:103-13. [Google Scholar]
[17]. IU Van der Waal, R Rauhamaa, WAM van der K Wast, GB Snow, Squamous cell carcinoma arising in the lining of odontogenic cysts: Report of 5 casesInt J Oral Surg 1985 14:145-52. [Google Scholar]