Case Report
A 38-year-old male patient reported to the Department of Conservative Dentistry, Goa Dental College and Hospital, Goa, with chief complaint of swelling in the upper front region of jaw, which had occurred 1 year back. Patient gave history of trauma in upper anterior teeth, which had occurred more than 25 years back. Patient had visited a private clinic 1 year prior for a similar complaint. Root canal opening was done with 11 and 21.
Intraoral clinical examination revealed a round to oval swelling which was located over labial mucosa of maxillary anterior region in association with 21,11,12 and 13 [Table/Fig-1]. Swelling was soft, localized, fluctuant, inflamed and nontender. Spontaneous pus discharge was seen from gingival sulcus. Ellis class IV fractures of 11 and 21 with severe discolouration were also seen.
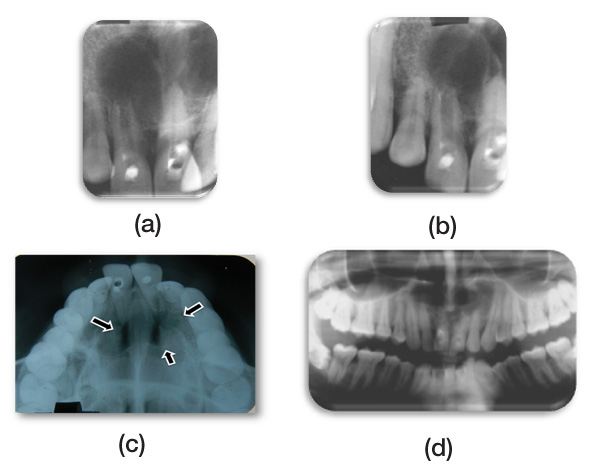
Electric and thermal pulp vitality testing showed negative responses in 21,11,12, and 13, while 22 showed a delayed response. All teeth were non-tender to percussion test. An IOPA [Table/Fig-2a,2b] was taken, which revealed a large unilocular radiolucent lesion which involved periapical regions of 21,11,12 and 13 respectively. Also, incomplete development of root, which led to open apex, was seen with 21. True occlusal X-ray and OPG showed unilocular radiolucency with sclerotic borders and there was no cortical expansion [Table/Fig-2c,d].
Patient was subjected to CT scan for further exploration of the finding, to check for proximity or any involvement of lesion with nasal floor, since lesion was extensive. CT showed that the nasal floor was intact and the radiolucency was seen in relation with 21 in saggital and coronal planes [Table/Fig-3a,c,d]. Based on these, a 3D construction image was plotted [Table/Fig-3b]. The dimension of the lesion was measured by using measurement scale which was around 12 x 2.5 x 2.5 mm. A fine needle aspiration of the swelling was done and it was sent for protein estimation, which was 6.6 g/dl.
From the history, clinical examination and investigation, a provisional diagnosis of infected radicular cyst in 22 was made.
Treatment plan was formulated and after explaining it to the patient, his informed consent was taken. Root canal opening with 11,12,13,21 and 22 was done under rubber dam application. Pus discharge was seen with 21 after access opening. After determination of working length and biomechanical preparation, calcium hydroxide intracanal medicament was used for one week. Then, in next appointment, obturation was completed. Tooth 21 with open apex was managed by using customized Roll cone technique.
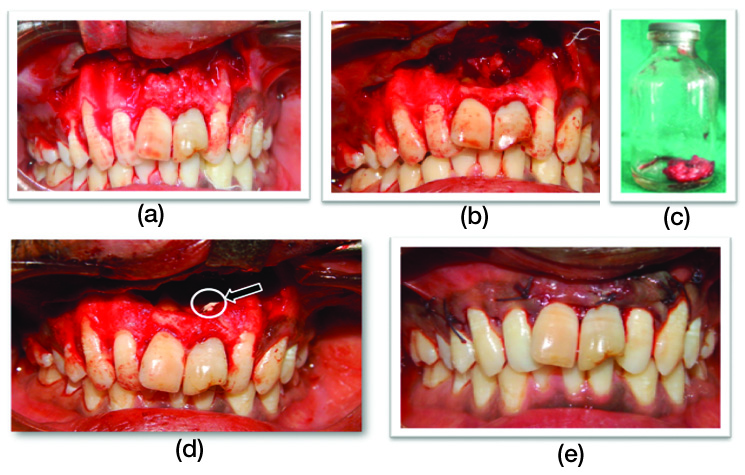
Patient was prepared for surgery in next visit, which included surgical enucleation of cyst, apicoectomy and retrograde filling of involved tooth. After administration of local anaesthesia, crevicular incision was made in labial region 13 to 23. A full thickness mucoperiosteal flap was reflected [Table/Fig-4a] and a large bony defect with open apex of 22 was seen clinically. Complete curettage, along with granulation tissue removal [Table/Fig-4b] and enucleation of cystic lesion was done and it was sent for histopathological evaluation [Table/Fig-4c]. Root end of 22 was resected and retrograde filling was done with MTA [Table/Fig-4e], and flap closure was done with 3-0 silk [Table/Fig-4e].
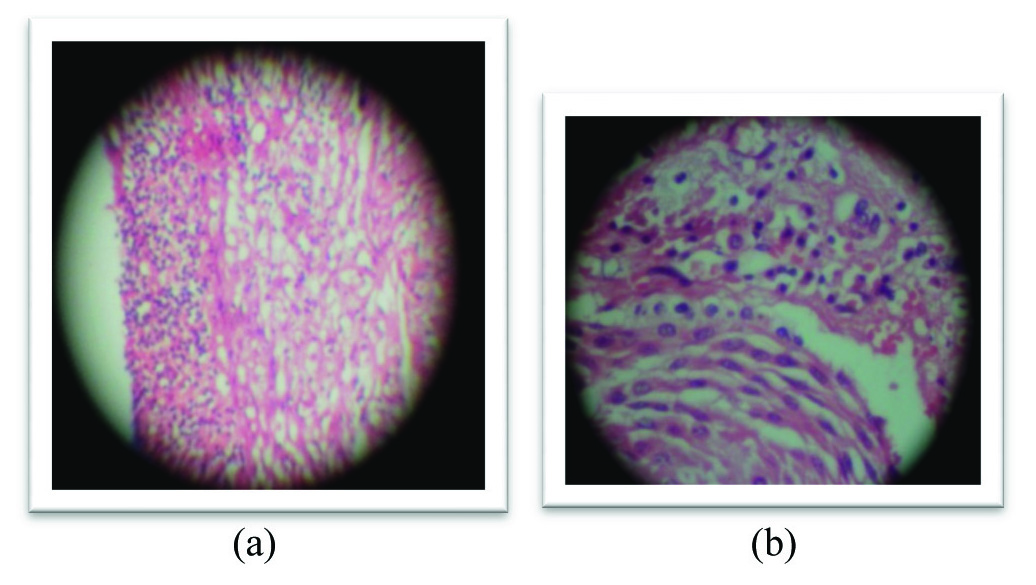
The histopathology report confirmed the provisional diagnosis of an infected radicular cyst [Table/Fig-5].
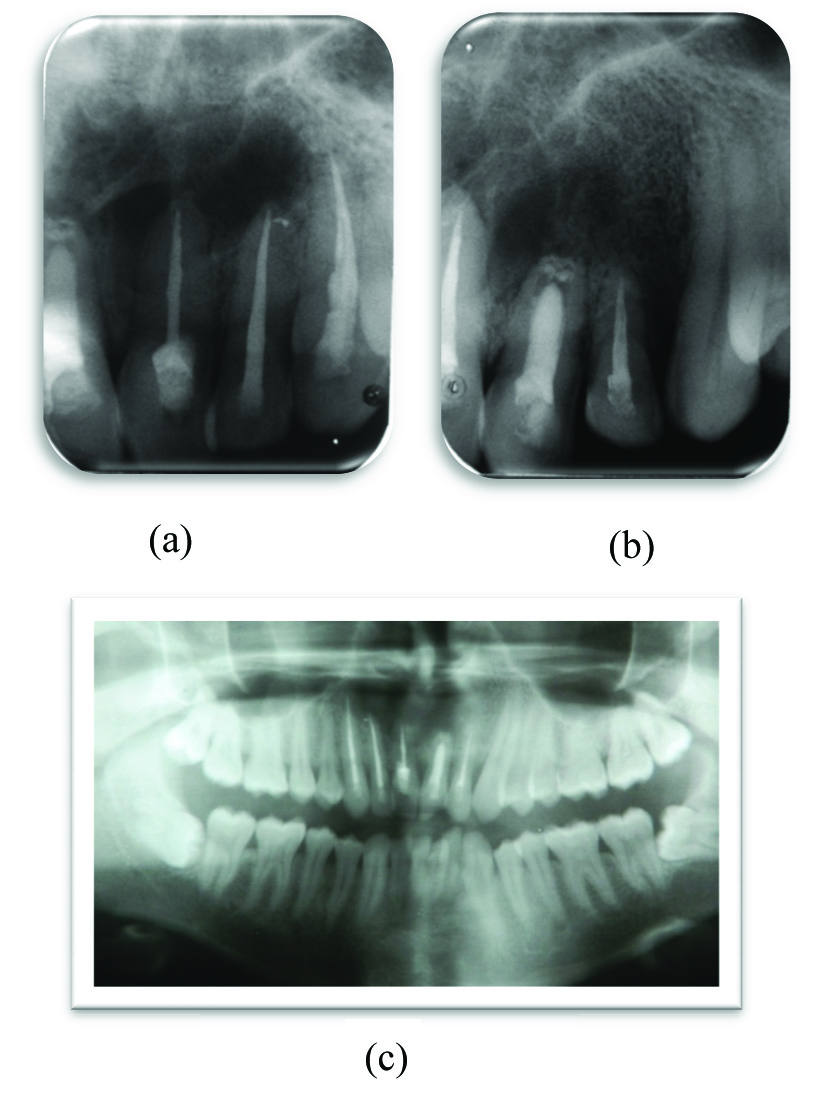
Post-operative instructions were given to the patient and patient was kept on antibiotics and analgesics. Currently, the patient is asymptomatic and he is under follow-up since 1 year [Table/Fig-6]. Follow-up radiograph showed appreciable healing.
Intraoral picture showing extent of lesion

(a) and (b) IOPA xray, (c) True Occlusal radiograph and (d) OPG showing large unilocular radiolucency involving 21, 11, 12 and 13
CT scan images of the lesion (a) showing 21 involvement with lesion in saggital plane (c and d) in transverse plane (b) 3D reconstruction of the images

Surgical pictures (a) full thickness flap eleveated (b) after surgical enucleation of the Cyst (c) enucleated tissue (d) placement of MTA after apicoectomy and (e) after placement of 3-0 Silk sutures
Histopathological picture showing the cystic cavity was lined by non-keratinized stratified squamous epithelium with mixed inflammatory infiltration present(a) at 10x and (b) 40 X magnification
Followup radiographs showing appreciable healing of the lesion (a and b) IOPA’s (c) OPG after 1 year of follow-up
Discussion
The term, ‘cyst’ is derived from the Greek word, ‘Kystis’, meaning, ‘sac or bladder’ [1]. Cyst is defined as a pathological cavity that is usually lined by epithelium and which has a centrifugal, expansive mode of growth [2].
Radicular cysts are the most common cystic lesions which affect the jaw. They are most common of all the jaw cysts and comprise about 52% to 68% of all the cysts which affect the human jaw [3,4]. They arise from epithelial remnants which are stimulated to proliferate, by an inflammatory process which originates from pulpal necrosis of a non-vital tooth. The natural history begins with a non-vital tooth which remains in situ, long enough to develop chronic periapical pathosis [5]. They are most commonly found at the apices of the involved teeth. However, they may also be found on the lateral aspects of the roots in relation to lateral accessory root canals [6]. They are symptomless and are diagnosed during routine radiologic investigations. The treatment for radicular cysts includes conventional nonsurgical root canal therapy when lesion is localized or surgical treatment like enucleation, marsupialization or decompression when lesion is large [7].
Radicular cysts generally originate after trauma or dental caries. Dental caries cause inflammation of the pulp cavity, leading to pulp necrosis [8]. The infection then spreads to the tooth apex of the root, causing periapical periodontitis, which leads to either an acute abscess or a chronic granuloma. Persistent chronic infection can lead to formation of a periapical cyst [9]. In the current case, patient had given a history of trauma previously; it could be the probable aetiology.
Cortical expansion and root resorption of the affected tooth and displacement of the adjacent teeth are common features of radicular cysts [9]. In the current case, there was cortical perforation and adjacent teeth in relation to the cyst were non-vital, which is not common. It has been stated that as the cyst enlarges, adjacent teeth can become non-vital [10].
The use of root canal dressings between sessions in root canal treatment of teeth with chronic periapical lesions is important, for reducing bacteria which are unreachable by instruments or irrigation solutions, such as dentinal tubules and ramifications [11]. Takahashi et al., after analyzing the pH and the concentration of calcium ions in the periapical area, concluded that at least 2 weeks were necessary for calcium hydroxide bactericidal activity[12]. In the current case, calcium hydroxide intracanal medicament was used.
When the canal is wide and walls are parallel, the tapered shape of GP will not fit adequately. In such cases, it is necessary to roll three or more GP cones together on glass slab, in order to make a thick GP cone of even diameter [13]. In the current case, tooth 21 presented with wide canals with open apex. It was successfully managed by roll cone technique obturation.
Due to the large size of the lesion, conservative surgical approach was planned. Conservative approach involves the removal of the infected tissues as compared to procedures like En bloc resection, which involves removal of the normal structure along with diseased tissue. The surgical approach to cystic lesions of the jaws is either marsupialization or enucleation. The treatment of choice is dependent on the size and localization of the lesion, the bone integrity of the cystic wall and its proximity to vital structures [14]. MTA is widely used as a root end filling material [15,16]. MTA has been favoured due to its higher biocompatibility and sealing ability over the currently available root-end filling materials[17]. In the current case, the lesion was enucleated along with curettage, followed by apicocectomy and placement of MTA as root end filling material.
Post-surgical period was uneventful. The histopathological features of the submitted lesion were consistent with the clinical diagnosis of infected radicular cyst. The cystic cavity was lined by nonkeratinized, stratified squamous epithelium with mixed inflammatory infiltration being present [Table/Fig-5a,5b].Intracoronal bleaching, followed by composite restoration, was planned for the patient. But patient was not interested in the restorative phase of the treatment due to economical reasons.
Healing of the periapical area has not yet been completed, due to large area of destruction. Currently, patient is asymptomatic and he has been kept under observation.
Conclusion
The current concept in management of periapical cysts is using nonsurgical means. However, depending on size and extent of lesion, surgical management might be necessary, for achieving success. Current case was managed successfully by performing endodontic therapy with thorough irrigation, cleaning and shaping and obturation of the canal space, followed by surgery.
[1]. PN Nair, New perspectives on radicular cysts:do they heal?Int Endod J 1998 31:155-60. [Google Scholar]
[2]. HF Sailer, Pajarola GFOral Surgery for the General Dentist 1999 New YorkThieme [Google Scholar]
[3]. F Riachi, C Tabarani, Effective management of large radicular cysts using surgical enucleation vs. marsupialisationIAJD 2010 1:44-51. [Google Scholar]
[4]. S Latoo, AA Shah, MS Jan, S Qadir, I Ahmed, AR Purra, Radicular cystJ.K. Science 2009 11:187-9. [Google Scholar]
[5]. G Dimitroulis, J Curtin, Massive residual dental cyst: case reportAust Dent J. 1998 43:234-7. [Google Scholar]
[6]. PN Nair, Non-microbial etiology: periapical cysts sustain post-treatment apical PeriodontitisEndod Topics 2003 6:96-113. [Google Scholar]
[7]. RP Domingos, S Gonçalves Eduardo, S Neto Eduardo, Surgical approaches of extensive periapical cyst. Considerations about surgical techniqueSalusvita Bauru 2004 23:317-28. [Google Scholar]
[8]. LM Lin, GT Huang, PA Rosenberg, Proliferation of epithelial cell rests, formation of apical cysts, and regression of apical cysts after periapical wound healingJ Endod 2007 33:908-16. [Google Scholar]
[9]. AL Weber, T Kaneda, SJ Scrivani, Jaw Aziz S, tumors and nontumorous lesions. In: Som PM, Curtin HD, edsHead and neck imaging 2003 4th EditionMosbySt. Louis, MO:930-934. [Google Scholar]
[10]. L Andersson, KE Kahnberg, MA Pogrel, Oral and Maxillofacial Surgery 2010 WileyBlackwell [Google Scholar]
[11]. MR Leonardo, FF Silveira, LA Silva, M Tanomaru Filho, LS Utrilla, Calcium hydroxide root canal dressing histopathological evaluation of periapical repair at different time periodsBraz Dent J. 2002 13:17-22. [Google Scholar]
[12]. Y Takahashi, T Yoshida, S Takashima, The regulation of intracellular calcium ion and pH in young and old fibroblast cellsJ Gerontol 1992 47:B65-70. [Google Scholar]
[13]. Louis Grossman, Endodontic Practice 1988 11th EditionLea and Febiger EditorLea and Febiger Editor:194 [Google Scholar]
[14]. L Bodner, Cystic lesions of the jaws in childrenInt J Pediatr Otorhinolaryngol. 2002 62:25-9. [Google Scholar]
[15]. KT Koh, Mineral trioxide aggregate (MTA) as a root end filling material in apical surgery: a case reportSingapore Dent J. 2000 23:72-8. [Google Scholar]
[16]. S Shahi, Comparison of the sealing ability of mineral trioxide aggregate and Portland cement used as root-end filling materialsJ Oral Sci 2011 53:517-22. [Google Scholar]
[17]. I Islam, HK Chng, AU Yap, Comparison of the physical and mechanical properties of MTA and Portland cementJ Endod 2006 32:193-7. [Google Scholar]