Synchronous Multicentric Giant Cell Tumour (GCT)-A Rare Case Report
Anshu Shekhar1, Gururaj Murgod2, Suresh Korlhalli3
1Assistant Professor, Department of Orthopaedics,Sri Dharmasthala Manjunatheshwara College of Medical Sciences and Hospital, Karnataka, India.
2Assistant Professor, Department of Orthopaedics,K.I.M.S., Hubli, Karnataka, India.
3Professor and HOD, Department of Orthopaedics,K.I.M.S., Hubli, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anshu Shekhar, Assistant Professor, Department of Orthopaedics, S.D.M. College of Medical Sciences and Hospital, Sattur, Dharwad-580009, Karnataka, India.
Phone: +91 808 814 2231,
E-mail:dr.anshushekhar@gmail.com
Giant Cell Tumours (GCT) of bone account for 5% of all primary bone tumours. Multicentric variety is a rare variant of this condition, accounting for less than 1% of all cases and can occur as synchronous or metachronous lesions. We report a 22-year-old male patient with 18 months history of painful progressive swellings around the right knee. Radiographs revealed expansile lytic lesions in the distal femur, proximal tibia and fibula and core needle biopsy was typical of GCT. Biochemical parameters were normal and radiological investigations did not reveal any metastasis. The patient was treated by above knee amputation due to the extensive nature of the tumours. The excised tissue from all sites had features of giant cell tumor with no atypia or malignant cells seen. The patient is free from recurrence or metastasis at three years follow up.
Neoplasms, Synchronous multiple primary, Amputation
Case Report
A 22-year-old male presented with one-and-half year history of painful, progressively increasing swelling around the right knee joint, which was insidious in onset. The swelling first appeared in the proximal tibia for which he took self medication for pain relief. After eight months he noticed another swelling in the distal femur which was progressing at a faster rate and was more painful. Subsequently, he developed a wound over the tibial swelling following a trivial fall, which progressively increased in size. There was no history of fever, cough, hemoptysis or weight loss.
Physical examination revealed 15 x 8 cm circumferential swelling in proximal tibia with dilated veins and an exophytic growth anteriorly. The swelling was tender, hard in consistency, rough irregular surface with well defined borders. A 7x6 cm ulcer as present at the apex of this swelling anteriorly with everted edges, indurated base and covered with slough. Another well defined swelling of 18 x 10 cm was present circumferentially at the distal end of femur with local warmth, tenderness, hard in consistency, irregular rough surface and deep to the quadriceps muscle [Table/Fig-1]. He had a fixed flexion deformity of 30 degrees at the knee with flexion up to 80 degrees possible. Wasting of thigh and calf muscles was evident. Two inguinal lymph nodes were palpable and tender but mobile. There was no distal neurovascular deficit.
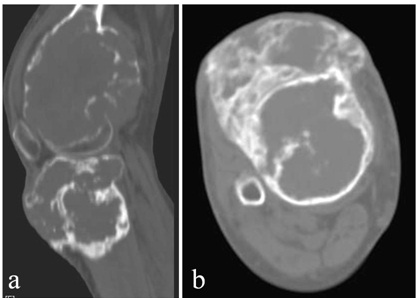
Radiograph of the right knee showed large expansile, osteolytic lesions with soap bubble appearance, no periosteal reaction and no matrix calcification in the distal femur, proximal tibia and proximal fibula with cortical breach at all sites. The lesion in the tibia was primarily metaphyseal [Table/Fig-2]. Computed Tomography (CT) scan showed cortical breach in the tumours and the exophytic extent of tibial tumour [Table/Fig-3]. Magnetic Resonance Imaging (MRI) of the lesion was hypointense on T1 weighted images and revealed the popliteal artery and tibial and common peroneal nerves to be pushed by the mass but not encased by it. CT scan of the chest and abdomen was done to look for any metastatic deposits but was normal. Fine needle aspiration cytology of inguinal nodes was suggestive of reactive lymphadenitis. Whole body Technetium 99m scan did not reveal any other site of involvement. Serum calcium, phosphorus, alkaline phosphatase and parathyroid hormone levels were normal. Core needle biopsy from femur and tibial lesions was performed which showed scattered osteoclastic giant cells and clusters of stromal cells suggestive of GCT.
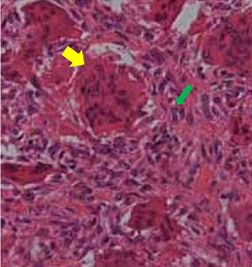
The patient subsequently underwent transfemoral amputation as the tumor was too extensive for curettage and resection with endoprosthetic reconstruction carried high risk of infection due to the presence of an ulcer [Table/Fig-4]. Histopathology examination of the tumours revealed features typical of GCT and no evidence of malignancy was seen [Table/Fig-5]. Bone margin was negative for tumour cells. The patient has no recurrence, new lesions or lung metastasis after three years.
Clinical photograph of the tumours around the right knee with ulcer over the tibia and flexion deformity of the knee

Radiograph of the tumours showing an epiphyseal lytic lesion in the femur, primarily metaphyseal lesion in the tibia, destruction of fibula head with decreased knee joint space and subluxation of the joint

CT scan revealed multiple cortical breaches in femur and tibia in the saggital section (a). Axial section of the tibial tumour showing its exophytic component (b)
Clinical photograph of the patient after he underwent transfemoral amputation

Multinucleated giant cells (yellow arrow) and oval stromal cells (green arrow) typical of giant cell tumours seen on hematoxylin-eosin stain
Discussion
In 1912, Joseph Bloodgood was the first to refer to this lesion of the bone as GCT. This tumour must be considered a clinicalradiologic- pathologic entity [1]. GCT of the bone are unpredictable lesions that account for 4-5% of primary bone tumours in the West but Multicentric Giant Cell Tumour (MGCT) nevertheless is a rare entity, with the reported incidence in the literature being less than 1% of all GCTs. Around 101 cases of MGCT have so far been reported in literature, with the vast majority being single case reports [2]. Multicentricity is defined when more than single lesion is encountered in a patient. Usually two or three tumours are seen initially but ten lesions in a patient have been detected [3]. Hoch et al., further classified multicentricity as being synchronous when multiple tumours are discovered initially or diagnosed within a period of six months, or metachronous when the second tumour appears six months or more after the diagnosis of the first [4]. Various pathogenic mechanisms of multicentricity have been suggested including contiguous spread, iatrogenic tumour cell seeding, benign metastasis, malignant transformation and de novo multifocal formation [2]. It is also believed that lesions in MCGCT arise independently, like other polyostotic bone diseases rather than being multiple sites of metastases from a single tumour, as no destructive pattern of metastatic disease is seen at any site. A germ-line genetic abnormality that predisposes patients to develop multiple tumours has also been postulated but no familial cases have been reported so far [4].
MCGCTs occur at an earlier age than solitary tumours, the average age being 22.5 years and are more common in the immature skeleton [2]. However, they have a slight female preponderance like solitary GCTs [2,5]. Although multicentric lesions are commonest around the knee followed by proximal humerus and distal radius like solitary GCTs, they are more prevalent in short bones of the hand and feet [2]. MCGCTs are more frequently found to arise from metaphysis or meta-diaphysis, with a reported incidence of 10-14%, as against 5% for solitary lesions which are classically epiphyseal in location [2,6]. Our patient fits in the typical age for MCGCT and had three synchronous lesions in the right femur, tibia and fibula.
Diagnosis of GCT is critically dependant on correlating clinical data, radiologic analysis and pathologic evaluation [6]. MCGCTs should be distinguished from other multifocal lesions; such as brown tumours of hyperparathyroidism, multifocal giant-cell reparative granuloma, Paget’s disease, fibrous dysplasia, fibrosarcoma, metastasis, osteosarcoma, multiple myeloma, multifocal osteomyelitis and rarely osseous hydatid disease [7].
Radiographically, MCGCTs are indistinguishable from solitary GCTs [2]. The lesions in our patient were Campanacci Grade III [5]. MRI scan is currently the best imaging modality since it allows accurate tumour delineation, extra-osseous extent and articular surface involvement. CT is a reasonable alternative to define intraosseous extension [7]. The histological characteristics of MCGCT do not differ from that of solitary tumours although some cases may contain fibroblastic and fibrohistiocytic areas which are probably features of degeneration or involution [4]. More importantly, the histologic appearances are of no significant value in predicting the behaviour of the lesion and MCGCTs demonstrate aggressive behavior similar to that of primary GCT [4,5]. Pulmonary metastasis is reported at 5-10% in patients with multicentric GCTs as against 1-2% in patients with solitary GCTs [7].
The current modalities of treatment of GCT are intralesional extended curettage and reconstructing the defect, wide resection and reconstruction and rarely, amputation [8]. The factor that definitely influences outcome is the surgical margin [5]. In our case, the patient had a tumour big enough to preclude the option of curettage. The presence of non healing ulcer made resection with endoprosthesis implantation fraught with the risk of infection and hence was ruled out. We thus performed a transfemoral amputation after discussing with the patient.
Since MCGCT occurs in less than 1% of GCT, screening of all patients for multicentricity may not be cost-effective. Half-yearly screening by either bone scan or skeletal survey is recommended for GCTs at unusual sites or those diagnosed with multicentric involvement for at least five years and less frequently thereafter [2].
Thus, our patient had three synchronous tumours with typical radiographic, histologic and clinical features of GCT. Clinicalradiologic- pathologic correlation is critical to differentiate this rare but distinct tumour from a host of polyostotic osseous lesions with similar presentation. Management principles are the same as for solitary GCTs. Regular follow-up is critical to detect new lesions and metastasis.
[1]. EF McCarthy, Giant-cell tumor of bone: An historical perspectiveClin Orthop Relat Res. 1980 153:14-25. [Google Scholar]
[2]. Dhillon Mandeep S, Prasad Prabhudev, Multicentric giant cell tumour of boneActa Orthop Belg 2007 73(3):289-99. [Google Scholar]
[3]. IK Park, IH Jeon, Multicentric giant cell tumour of bone: Ten lesions at presentationSkeletal Radiol 2003 32:526-29. [Google Scholar]
[4]. B Hoch, C Inwards, M Sundaram, AE Rosenberg, Multicentric giant cell tumor of bone: clinicopathologic analysis of thirty casesJ Bone Joint Surg 2006 88:1998-2008. [Google Scholar]
[5]. M Campanacci, N Baldini, S Boriani, A Sudanese, Giant cell tumour of boneJ Bone Joint Surg 1987 69:106-14. [Google Scholar]
[6]. FH Sim, DC Dahlin, JW Beabout, Multicentric Giant cell tumour of boneJ Bone Joint Surg. 1977 59(A):1052-60. [Google Scholar]
[7]. Wirbel Reiner, Blumler Frank, Lommel Dirk, Syre Guido, Krenn Veit, Multicentric Giant Cell Tumor of Bone: Synchronous and Metachronous Presentation. Case Reports inOrthopedics 2013 Article ID 756723, 5 pages. doi:10.1155/2013/756723. [Google Scholar]
[8]. Puri Ajay, Agarwal Manish, Treatment of giant cell tumor of bone: Current conceptsIndian Journal of Orthopaedics 2007 41:101-08. [Google Scholar]