Abdominal Cocoon: An Unusual Presentation of Small Bowel Obstruction
R.G. Naniwadekar1, S.R. Kulkarni2, P. Bane3, S. Agrarwal4, A. Garje5
1Consultant, Department of General Surgery,Krishna Institute of Medical Sciences and Research Centre, Maharashtra, India.
2Consultant, Department of General Surgery,Krishna Institute of Medical Sciences and Research Centre, Maharashtra, India.
3Resident, Department of General Surgery,Krishna Institute of Medical Sciences and Research Centre, Maharashtra, India.
4Resident, Department of General Surgery,Krishna Institute of Medical Sciences and Research Centre, Maharashtra, India.
5Resident, Department of General Surgery,Krishna Institute of Medical Sciences and Research Centre, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR:Dr. R.G. Naniwadekar, Surgery Office, Ward 10, Krishna Institute of Medical Sciences, Karad, Maharashtra, India.
Phone: 0091-9960209192,
E-mail:drrgnaniwadekar@gmail.com
Abdominal cocoon is a rare condition. It presents as a thick whitish membrane which covers bowel loops. Because of this presentation, it is also called as sclerosing encapsulating peritonitis. It is usually diagnosed intra operatively. Treatment of this condition involves resection of the membrane and release of adhesions. Pre-operatively, patient is investigated for recurrent episodes of small bowel obstructions. However, preoperative diagnosis does not change the treatment and management. Investigations done preoperatively help in expediting the treatment with planned laparotomy
Sclerosing encapsulating peritonitis, Exploratory laparotomy, Bowel obstruction
Case Report
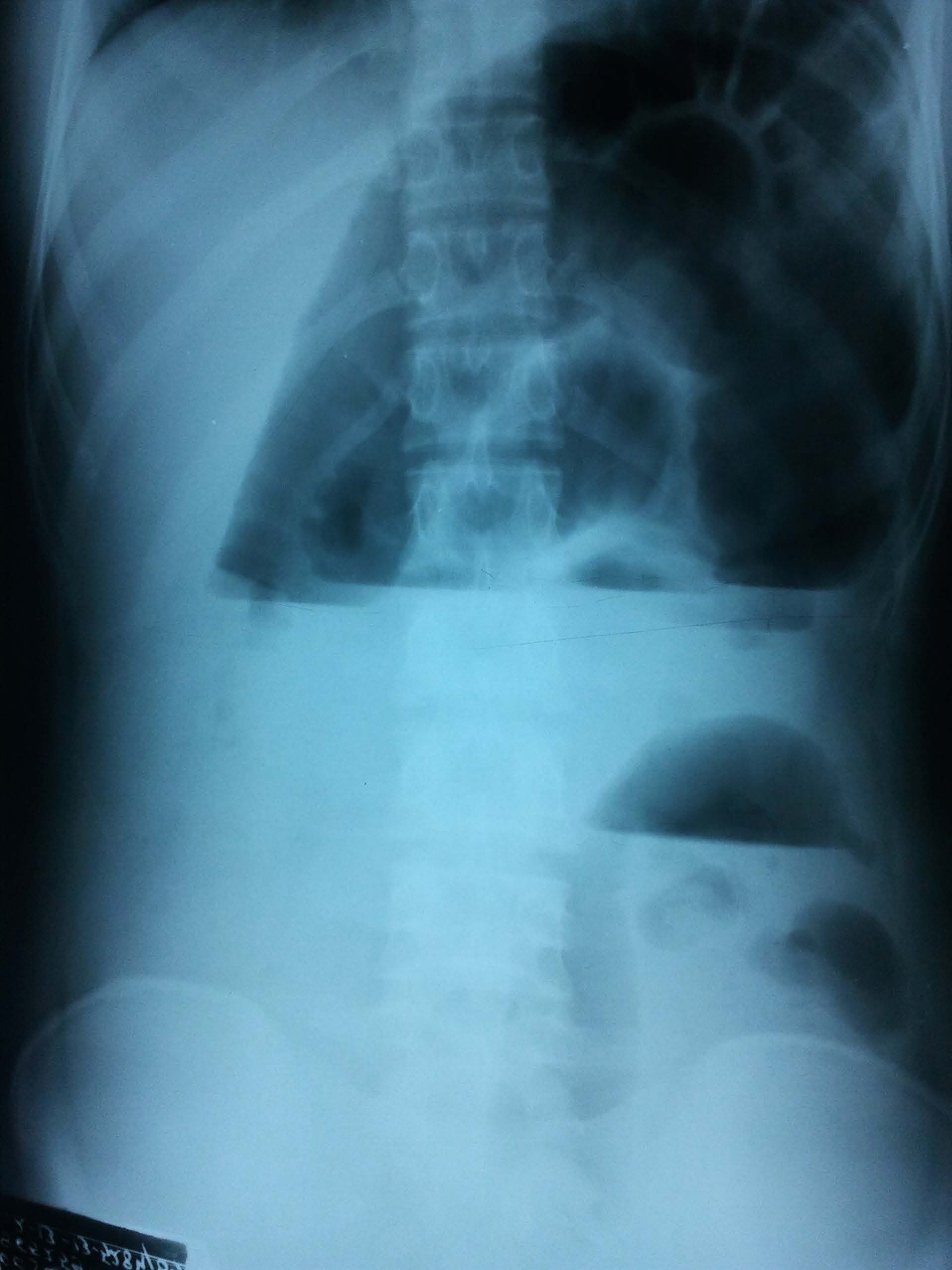
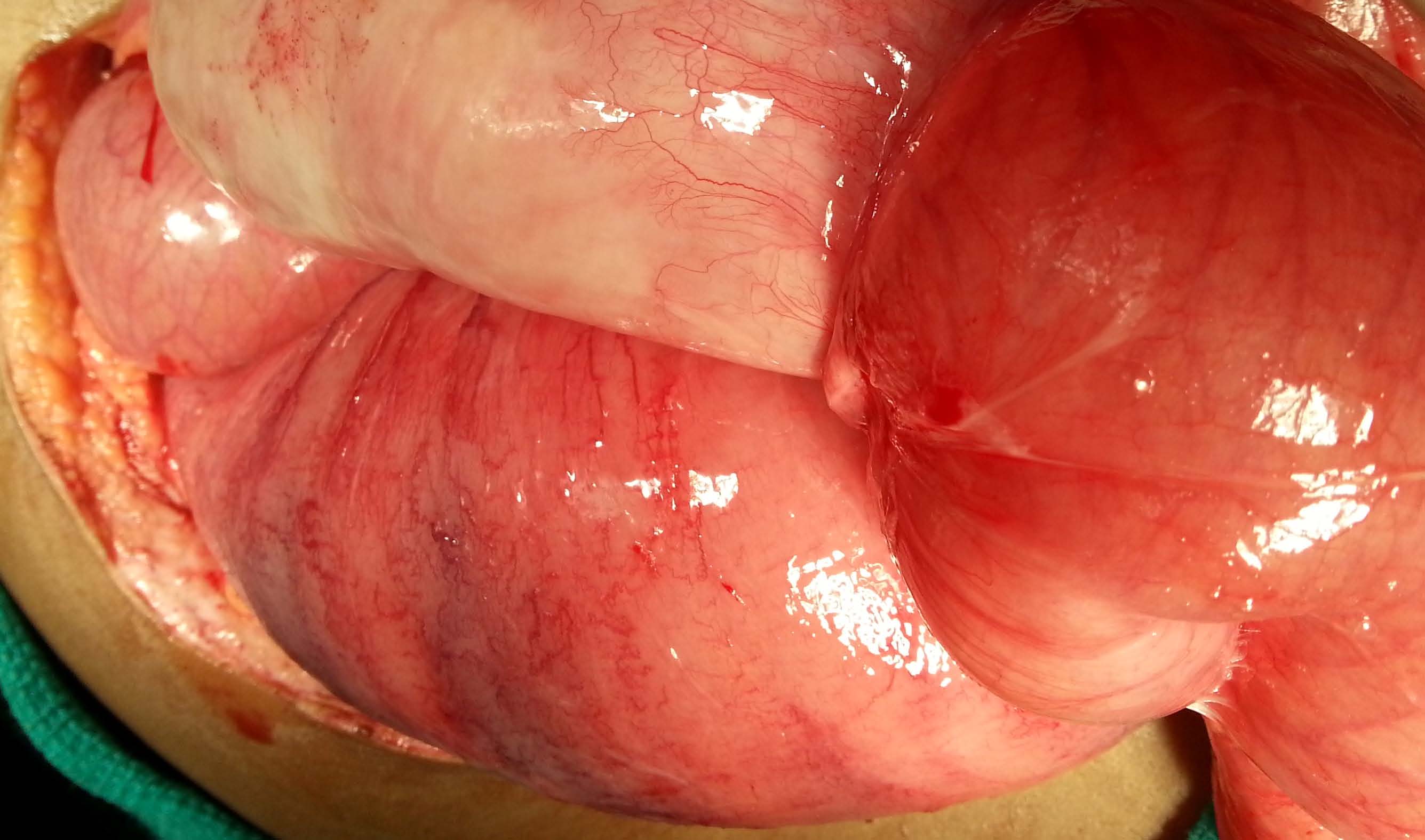
A 17-year-female presented with episode of abdominal pain and asymmetrical distension, which was associated with vomiting and constipation, which she had for 4 days. She had two similar episodes which had been treated conservatively. Her abdominal radiograph showed dilated bowel loops which were concentrated in centre and left of the abdomen, with ileal loops being bunched in the lower abdomen and pelvic cavity [Table/Fig-1]. Ultrasound showed dilated bowel loops with reduced peristaltic activity. She was investigated with ultrasound and upper GI scopy during previous episodes, which were normal. Exploratory laparotomy was done at this time, because signs of obstruction were not relieved. Intraoperative findings showed whitish thick membrane, encapsulating bowel loops [Table/Fig-2]. Thick membrane was resected. There were further adhesions between loops of small bowel, which were further released. Patient recovered completely and she comes for regular follow up.
Intra operative finding of abdominal cocoon
Discussion
Abdominal cocoon is a rare condition. It is commonly seen in young and adolescent populations. It is more common in females than in males [1]. Few cases of young males have been diagnosed with abdominal cocoon. It could be primary or secondary. Primary condition is idiopathic, secondary condition is commonly seen in peritoneal dialysis patients [2]. This is a rare condition in which small bowel loops are encased in thick fibrotic membrane with adhesions.
Pre-operatively, patient should be investigated for recurrent episodes of small bowel obstructions [3]. Upper GI scopy is suggested, but it may not show any positive finding. Ultra-sound of abdomen shows dilated bowel loops with soft-tissue density. Dilated loops are arranged in concentric fashion, in centre of abdomen or on the left side of the abdomen, with reduced peristalsis. Plane X-ray of abdomen shows dilated bowel loops in the centre of abdomen. Barium meal follow through shows changes of concertina pattern or cauliflower sign and delayed transit time of contrast medium. CT scan may help in making a definitive diagnosis. This rare condition is difficult to diagnose pre-operatively [4]. Pre-operative diagnosis does not change the treatment and management. Investigations done preoperatively, help in expediting the treatment with planned laparotomy.
Treatment of abdominal cocoon involves resection of membrane and release of adhesion [5]. Intraoperative findings show coils of intestine covered with thick fibrous membrane and adhesions between the coils. Resection of encapsulating membrane will return bowel loops to peritoneal cavity. Breaking of adhesions needs to be done carefully, to prevent damage to serosal surface and perforation [6]. Resection of bowel is not done, unless loops are strangulated. In our case, encapsulating membrane was excised and adhesions were released. Resection of bowel was not required, because bowel loops were not strangulated.
Conclusion
Pre-operative diagnosis of abdominal cocoon is difficult. Every attempt should be made, to reduce morbidity caused by emergency laparotomy. This rare condition is intraoperative diagnosis. Treatment involves resection of the membrane and release of adhesion. Condition heals completely if careful resection of membrane and release of adhesion are done.
[1]. G Gurleyik, S Emir, A Saglam, The abdominal cocoon: a rare cause of intestinal obstructionActa Chir Belg 2010 110(3):396-98. [Google Scholar]
[2]. MM Da Luz, SM Barral, CM Barral, S Bechara Cde, A Lacerda-Filho, Idiopathic encapsulating peritonitis: report of two casesSurg Today 2011 41(12):1644-48. [Google Scholar]
[3]. J Hur, KW Kim, MS Park, JS Yu, Abdominal cocoon: preoperative diagnostic clues from radiologic imaging with pathologic correlationAJR Am J Roentgenol 2004 182:639-141. [Google Scholar]
[4]. Tannoury Jenny N, Abboud Bassam N, Idiopathic sclerosing encapsulating peritonitis: Abdominal cocoonWorld J Gastroenterol 2012 18(17):1999-2007. [Google Scholar]
[5]. R Kaur, D Chauhan, U Dalal, U Khurana, Abdominal cocoon with small bowel obstruction: two case reportsAbdom Imaging 2012 37(2):275-78. [Google Scholar]
[6]. KK Ba, H Besim, A rare cause of intestinal obstruction: abdominal cocoonAm Surg. 2011 77(2):E24-E26. [Google Scholar]