Scalp Metastasis of Gastro-Esophageal Junction Adenocarcinoma: A Rare Occurrence
Asitava Deb Roy1, Mingma Sherparpa2, P.R.K Prasad3, Rachna Lamichanet4
1Assistant Professor,Department of Pathology,Sikkim Manipal Institute of Medical Sciences, Gangtok, India.
2Senior Consultant, Department of Neurosurgery,Sikkim Manipal Institute of Medical Sciences, Gangtok, India.
3Assistant Professor,Department of Pathology,Sikkim Manipal Institute of Medical Sciences, Gangtok, India.
4Assistant Professor,Department of Pathology,Sikkim Manipal Institute of Medical Sciences, Gangtok, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Asitava Deb Roy, Department of Pathology, Sikkim Manipal Institute of Medical Sciences, 5th Mile, Tadong, Gangtok-737102, Sikkim,India.
Phone: 9475587658,
E-mail: asitavadr@gmail.com
Cutaneous metastasis is one of the many skin changes which are associated with internal malignancies. Breast, lung, and colon are the most common sources of internal primary malignancies. Gastro-esophageal junction adenocarcinoma is a rare cause of cutaneous metastasis to the scalp. Gastric adenocarcinoma usually metastasizes to the liver, peritoneal cavity and regional lymph nodes more often than to skin. We are presenting a case of cutaneous metastasis on the scalp of a 79-year-old man, who was diagnosed and operated for gastro-oesophageal junction adenocarcinoma one year back.
Cutaneous metastasis, Gastro-esophageal junction adenocarcinoma
Introduction
Among the many skin changes which are associated with internal malignancies, one is the skin involvement which occurs as a result of cutaneous metastasis from an internal tumour. The incidence of cutaneous metastasis from malignant tumours has been estimated to be between 0.7% and 10.8% [1], among which the most common sources of internal primary malignancies are breast, lung, and colon.
Gastro-esophageal junction adenocarcinoma is a rare cause of cutaneous metastasis to the scalp[2]. Gastric adenocarcinoma usually metastasizes to the liver, peritoneal cavity and regional lymph nodes more often than to skin [3].
We are presenting a case of cutaneous metastasis on the scalp of a 79-year-old man who was diagnosed and operated for gastro-oesophageal junction adenocarcinoma one year back.
Case Report
A 79-year-old male patient who underwent a total radical gastrectomy with Roux-en-Y and oesophago-jejunostomy 1 year back for moderately differentiated adenocarcinoma of gastro-oesophageal junction (staged pT3N2M0), was hospitalized again with the chief complaint of a progressively increasing swelling in the right parietal region of scalp, with mild bleeding from the lesion, on and off. The swelling had been present at the time of his previous operation, one year back, but it was very small and hence, it had received no medical attention. Local examination showed a firm, indurated, highly friable mass, (3 × 3) cm, which was not attached to the cranial vault. X-ray was normal, except for increased vascularity of the lesion. CT revealed a hyperdense lesion in the right parietal extracranial space, which did not erode the skull. The lesion was totally excised under local anaesthesia and it was sent for histopathology.
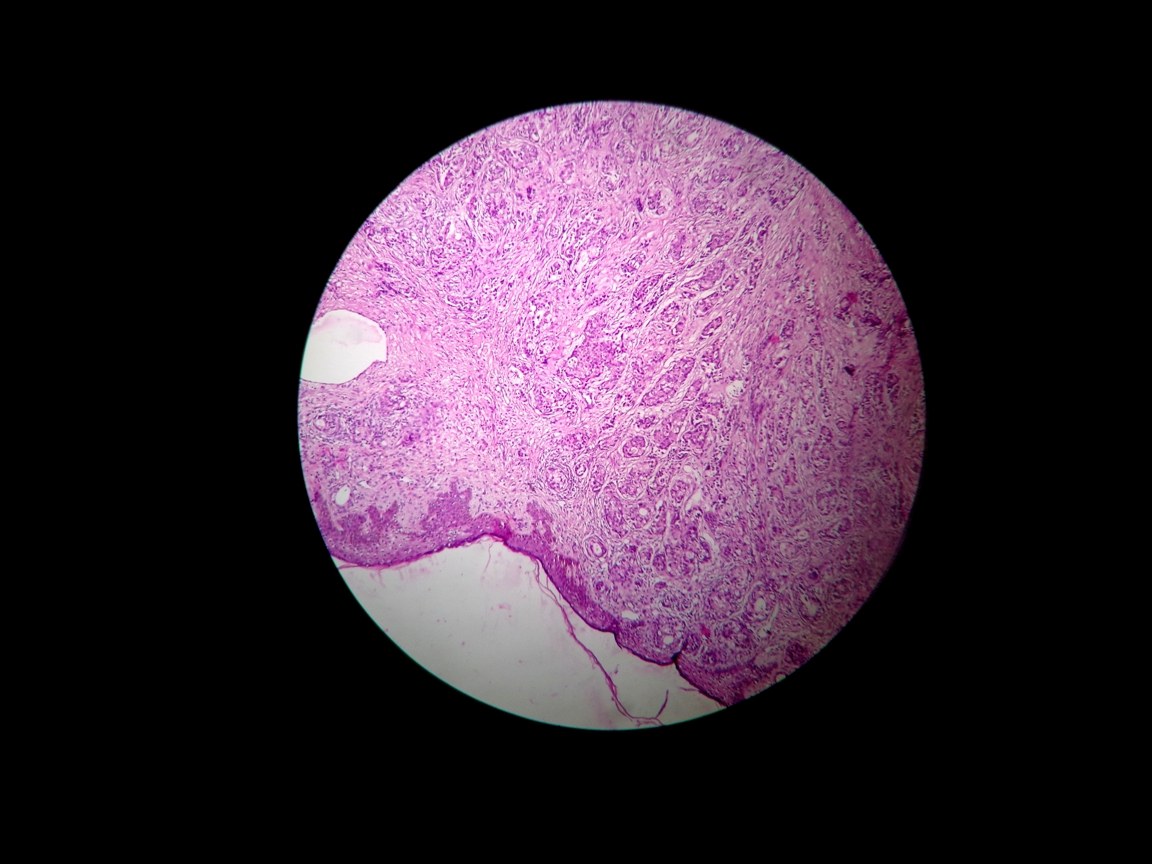
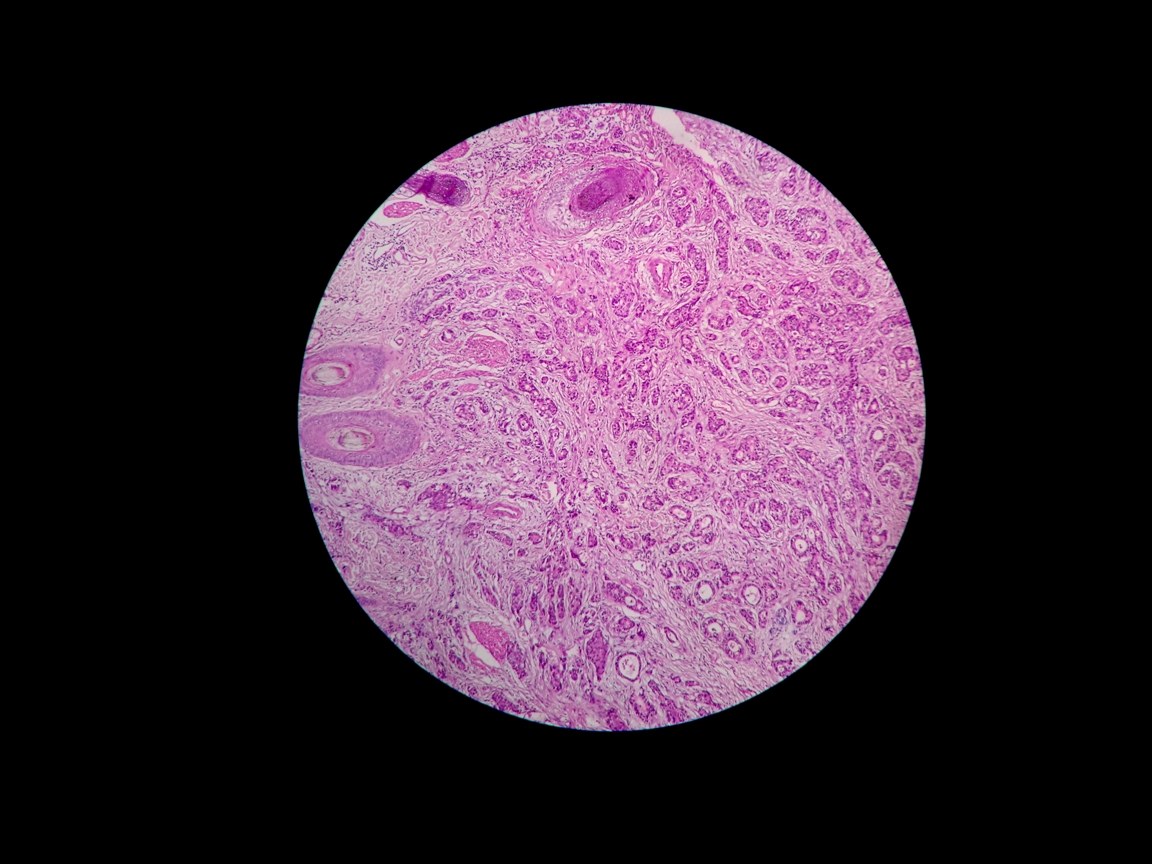
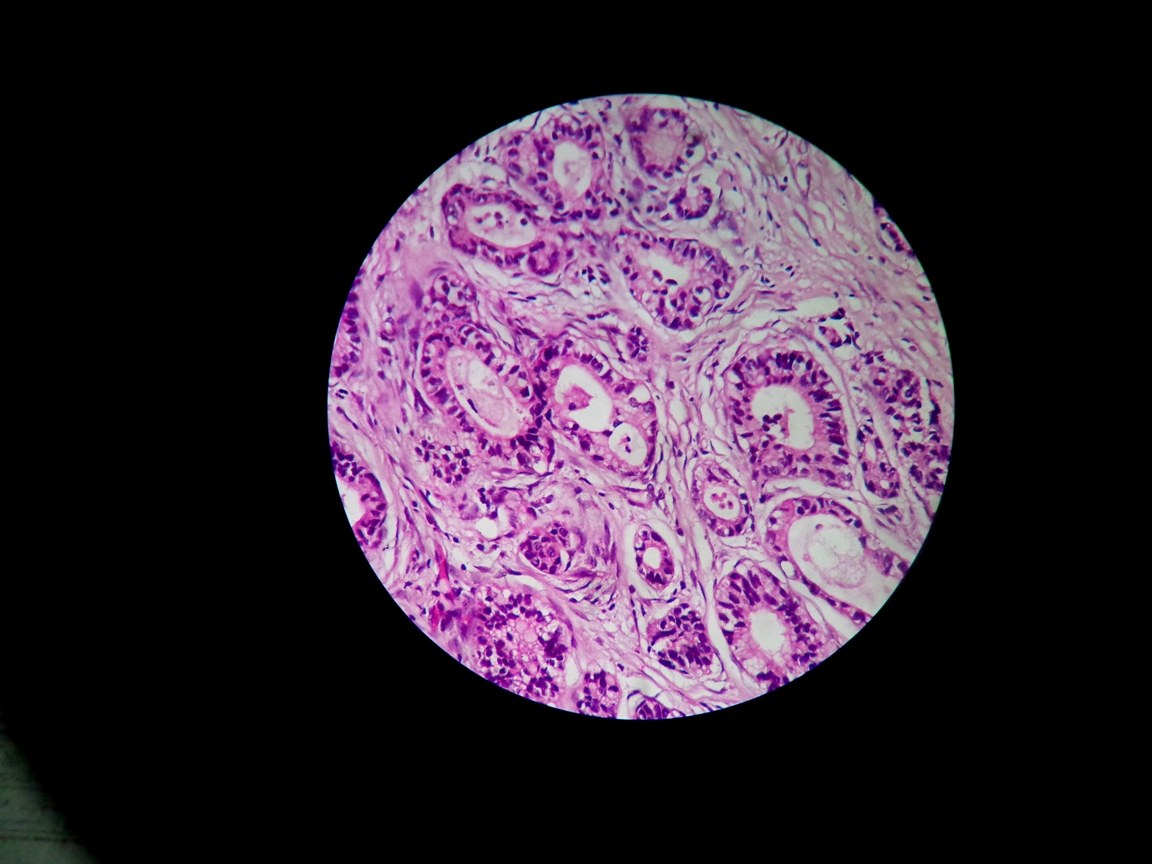
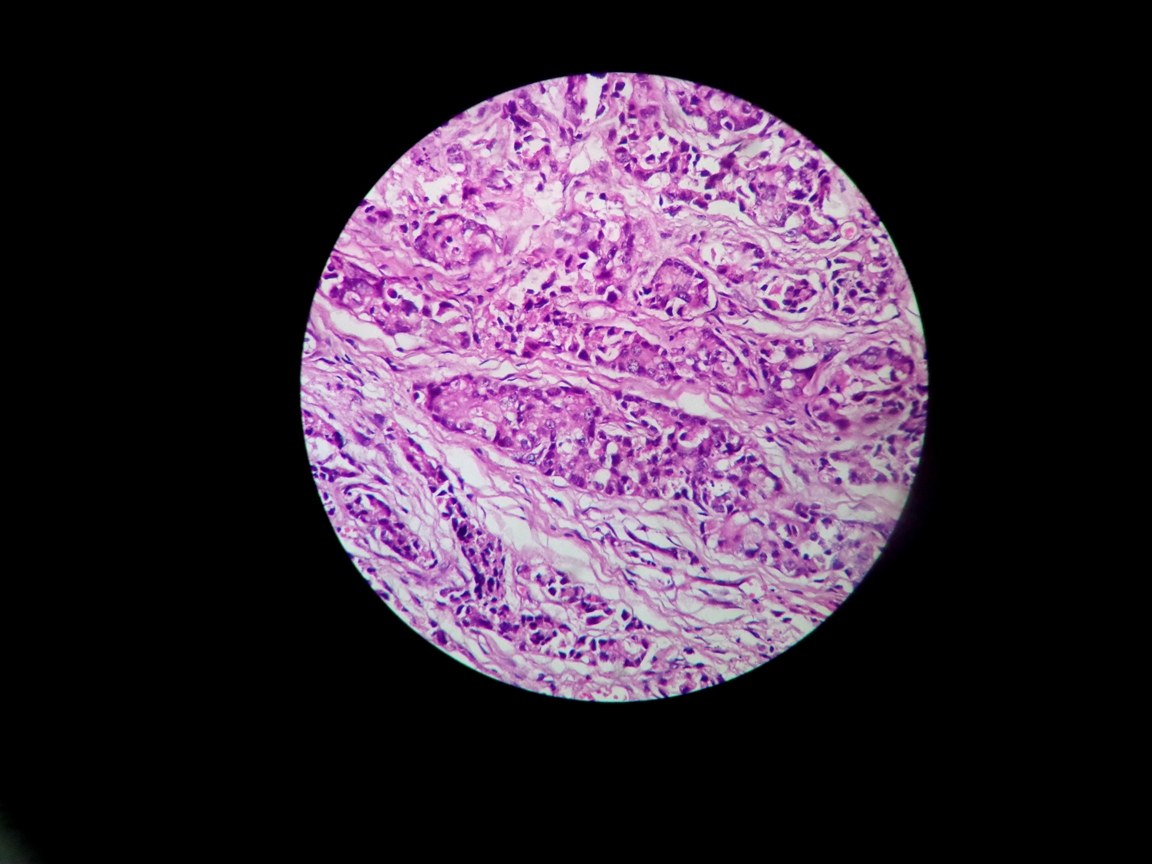
Histopathology revealed infiltrating neoplastic glands in the dermis and subcutaneous tissue [Table/Fig-1,2] which were irregular, but which were somewhat well formed and consisted of columnar cells which had large hyperchromatic and pleomorphic nuclei with inconspicuous nucleoli [Table/Fig-3]. Few solid nests of neoplastic cells were also noted [Table/Fig-4]. The cells were also found to contain mucin at places, which laterally displaced the nucleoli. Periodic Acid Schiff with diastase digestion confirmed the presence of mucin in the cells. The diagnosis of cutaneous metastasis from intestinal type of gastric adenocarcinoma was confirmed. The patient chose a conservative management for the metastatic skin lesion and hence, was discharged after proper palliation.
Histopathology showing dermal infiltration of neoplastic glands (H and E, 40x)
Histopathology showing infiltrating neoplastic glands with adjacent skin adnexal structures (H and E, 100x)
Histopathology showing neoplastic glands lined by tall columnar cells (H and E, 400x)
Histopathology showing nests of neoplastic cells in the dermis (H and E, 400x)
Discussion
Cutaneous metastasis is a relatively uncommon manifestation of visceral malignancies. The overall incidence of cutaneous metastasis from visceral neoplasms is 5.3% and it ranges from 0.7% to 9% [4-5]. The highest incidences of cutaneous metastasis have been seen for lung cancer in males and for breast cancer in females. Cancers of the lung, colon/rectum, kidney, ovary, and bladder all have similar rates for cutaneous metastasis, which range from 3.4% to 4% [5]. Gastric adenocarcinoma is however, a relatively rare cause of cutaneous metastasis, accounting for only 0.8% of the cases [6]. The most common manifestation of such cutaneous metastases from gastric adenocarcinoma has been multiple subcutaneous nodules on the trunk and the typical location has been demonstrated to be the umbilical area (Sister Joseph’s nodule) [7], which is near the primary cancer. Scalp in a rare site for metastasis of gastroesophageal junction adenocarcinoma [8] and this case is being presented because of the unusual location of the cutaneous metastasis.
The most common clinical presentation of cutaneous spread of internal cancer is the developments of nodules, usually firm and painless. However, there are exceptions to this rule, as has been shown in the index case, who developed a bleeding friable swelling. Other clinical presentations include neoplastic alopecia, carcinoma erysipelatoides, erythema annulare like, herpetiform or zosteriform, target like, pyodermatic, and morphea-like lesions[9].
In the Korean-language scientific literature, it has been reported that Kim et al., [10]investigated 4,806 patients with gastric carcinoma, of which only 15 (0.003%) had developed cutaneous metastasis.
Survival after diagnosis of the skin metastases is very short, ranging from 1 to 34 months [11]. Lookingbill et al., found an average survival of 18 months in colorectal cancers with cutaneous metastases. In general, skin metastasis is a poor prognostic sign. Treatment involves radiotherapy or excision and patients may survive up to a year [12].
In conclusion, in patients with internal malignancies, every skin nodules, nonhealing ulcers and persistent indurated erythema must be examined and investigated properly. Recognition of these cutaneous metastases can lead to diagnoses of underlying malignancies, it can help in accurate staging of the disease and enable life-prolonging therapy and in achieving meaningful palliation.
[1]. D Nashan, ML Müller, M Braun-Falco, S Reichenberger, RM Szeimies, L Bruckner Tuderman, Cutaneous metastases of visceral tumours: a reviewJ Cancer Res Clin Oncol 2009 135:1-14. [Google Scholar]
[2]. EP van Vliet, EW Steyerberg, MJ Eijkemans, EJ Kuipers, PD Siersema, Detection of distant metastases in patients with oesophageal or gastric cardia cancer: a diagnostic decision analysisBr J Cancer 2007 97:868-76. [Google Scholar]
[3]. Y Esaki, R Hirayama, K Hirokawa, A comparison of patterns of metastasis in gastric cancer by histologic type and ageCancer 1990 May 1(65(9)):2086-90. [Google Scholar]
[4]. RA Schwartz, Cutaneous metastatic diseaseJ Am Acad Dermatol 1995 33:161-182. [Google Scholar]
[5]. RA Krathen, IF Orengo, T Rosen, Cutaneous metastasis: a meta-analysis of dataSouth Med J 2003 96:164-67. [Google Scholar]
[6]. SC Hu, GS Chen, CS Wu, CY Chai, WT Chen, CC Lan, Rates of cutaneous metastases from different internal malignancies: experience from a Taiwanese medical centerJ Am Acad Dermato.l 2009 60:379-87. [Google Scholar]
[7]. HL Lee, YI Kwon, SY Song, Umbilical metastasis: Sister Mary Joseph’s noduleClin Gastroenterol Hepatol 2011 :9-20. [Google Scholar]
[8]. JY Park, IH Kwon, HS Lee, KH Cho, Four cases of cutaneousmetastasis to the scalp from internal malignanciesKorean J Dermatol 2002 40:666-70. [Google Scholar]
[9]. RP Kaplan, Specific cutaneous manifestations of internal malignancyAdv Dermatol 1986 1:3-43. [Google Scholar]
[10]. MS Kim, SG In, CH Won, SE Chang, MW Lee, JH Choi, A clinicopathological analysis of cutaneous metastasis from gastric cancer in KoreaKorean J Dermatol 2010 28:360-65. [Google Scholar]
[11]. MH Xavier, R Vergueiro Tde, EG Vilar, JM Pinto, MC Issa, GB Pereira, Cutaneous metastasis of gastric adenocarcinoma: an exuberant and unusual clinical presentationDermatol Online J 2008 :14-8. [Google Scholar]
[12]. DP Lookingbill, N Spangler, KF Helm, Cutaneous metastases in patients with metastatic carcinoma: a retrospective study of 4020 patientsJ Am Acad Dermatol 1993 29:228-36. [Google Scholar]