Primary Midgut Carcinoid, a Rare Cause of Paraneoplastic Limbic Encephalitis: A Case Report
Gautham Krishnamurthy1, K Chandramouleeswari2, Jagadeesh Chandra Bose3, Rajendran4
1Postgraduate Student, Department of Surgery,Stanley Medical College, Chennai, India.
2Professor, Department of Pathology,Stanley Medical College, Chennai, India.
3Professor and HOD, Department of Surgical Oncology,Stanley Medical College, Chennai, India.
4Postgraduate Student, Department of Surgery,Stanley Medical College, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. K. Chandramouleeswari, Professor, Department of Pathology, Stanley Medical College, Chennai, India.
Phone: 9444620097,
E-mail: chandrakathir@yahoo.com
A 60-year-old male presented with an unexplained seizure whose aetiology could not be demonstrated. After 8 weeks, patient on evaluation for abdominal pain was detected to have primary midgut carcinoid with nodal and hepatic metastasis. Patient underwent cytoreductive surgery and metastatectomy with successful outcome. The case is being presented for its rarity and the need to recognize the paraneoplastic neurological manifestations of these rare neuroendocrine tumors.
Neuroendocrine tumor, Paraneoplastic limbic encephalitis
Introduction
Carcinoid tumor, part of the neuroendocrine tumor family, is a rare tumor type predominantly affecting gastrointestinal and respiratory tract. Patients present with local complications or symptoms arising from metastasis, even fewer present with paraneoplastic syndrome as the primary manifestation. The present case described is of midgut carcinoid, presented initially with symptoms of possible paraneoplastic limbic encephalitis following which tumor was detected and treated accordingly.
Case Report
A 60-year-old male presented with an unexplained episode of seizure for which he was started on anti-epileptics after relevant investigations. Six months later, he came back with upper abdominal pain and constipation for 8 weeks. His relatives reported significant history of behavioural change since 8 months duration. Abdominal examination revealed a 3x3 cm ill-defined, firm and immobile mass in the peri-umbilical region. Computed tomography of the abdomen showed a well-defined, contrast enhancing lesion with a thin linear calcification at the root of mesentery and a narrowed segment of Small intestine measuring 3 cm in length with proximal small bowel dilatation. There were multiple para-aortic and aorto-caval nodes. Three small enhancing lesions involving both lobes of liver were identified.
Image guided core needle biopsy of mesenteric nodal mass was performed and histopathological examination revealed well differentiated neuroendocrine tumor. Serum chromogranin A done subsequently was 155 IU/L.
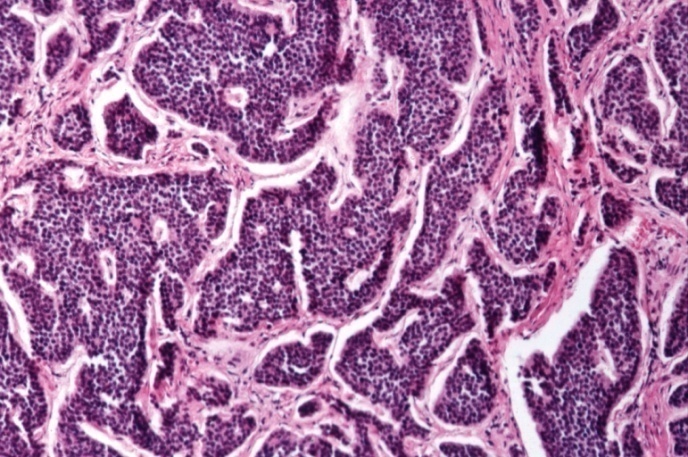
Intraoperative findings confirmed imaging findings of 3x2.5 cm tumor encircling the small intestine, multiple mesenteric nodes present in close proximity to the superior mesenteric artery and three metastatic liver nodules. Cytoreductive surgery was performed with removal of the tumor along with mesenteric nodal mass and hepatic metastasis [Table/Fig-1]. Histopathological examination of the resected specimen confirmed well-differentiated neuroendocrine carcinoma with infiltration into the serosa forming nodules[Table/Fig-2]. The resected mesenteric nodes and nodules from the liver were positive for metastatic deposit. Post operative period was uneventful.
Resected small intestine with tumour and attached mesentery with nodule measuring 23 cm. The lumen of the small intestine shows an ulceroinfiltrative tumour measuring 2.5x2x1.5 cm encircling the lumen. (Solid Arrow)

(10x view:) Showing islands and nests of tumor cells infiltrating the stroma
Discussion
Oberndorfer, described an intestinal tumor distinct from adenocarcinoma and biologically less aggressive [1-2]. Gosset and Mason hypothesized the origin of these tumors from the enterochromaffin cells of the gastrointestinal tract. Confirmation of this fact has now led to these tumors being classified as neuroendocrine tumors [2]. With development of molecular techniques and better understanding of the tumor biology, various classifications have been described and reported. Williams and Sandler’s classification is based on their embryological origin of these tumors: foregut, midgut and hindgut [3]. Tumors arising from different segments of the embryologic gut varied in their histologic, immunohistochemical, and bioactive amine production.
Nearly three-fourths of carcinoid tumors were from the gastrointestinal tract and rest from the bronchopulmonary tract. The incidence of the gastrointestinal disease is estimated around 2.5 to 5 per 100,000 with a surge in the recent past. Within the GI tract, small bowel carcinoids accounted for 42%, rectal 27%, and stomach 9% [4].
Small bowel carcinoids have a predisposition for the submucosa of the terminal ileum. Seventy percent of patients present with regional nodal metatstasis while 50% with hepatic metastasis. Desmoplastic reaction around the mesenteric nodal metastases causes contraction of the mesentery and kinking of the bowel. When the mesenteric vessels are included in this reaction, chronic ischemic changes of the antimesenteric border of the bowel occurs. Thus, patients often present with nonspecific abdominal pain and a history consistent with intermittent ischemia [5]. Due to the indolent behaviour of these tumors, patients usually have symptoms for a mean period of 5 years before the diagnosis is made and 43% present as advanced or metastatic disease at the time of presentation [5-6].
Carcinoid syndrome occurs in 20% to 30% of patients with small bowel carcinoids. The syndrome is characterised by flushing and diarrhoea, and, less frequently with heart failure and bronchoconstriction. It is caused by production of excessive bioactive amines. Due to the liver’s ability to deactivate serotonin, carcinoid syndrome typically occurs when liver metastases are present though not necessary [7].
Surgery plays an important role in the management of patients withsmall bowel carcinoids even in the presence of metastatic disease. Resection of the primary tumor and mesenteric nodal disease is effective in relieving symptoms of gastrointestinal obstruction and ischemic symptoms associated with these tumors. Resection of mesenteric nodal disease has also been associated with a survival benefit. Resection or ablation of hepatic metastases has been associated with improvement of symptoms of carcinoid syndrome in 67% to 96% of patients by reducing the release of serotonin and other hormones into the systemic circulation [8].
Paraneoplastic syndromes are those associated with certain tumors characterised by production of specific substances by the tumor cells and cause signs and symptoms distant to the site of tumor and may be humoral or neuronal. The manifestation of the primary and the paraneoplastic syndrome can have a variable temporal relation. Paraneoplastic limbic encephalitis has been rarely reported in neuroendocrine tumors, with few reported in bronchial carcinoids [9]. Production of auto-antibodies against the brain parenchyma is considered to cause specific neurological manifestations like personality changes and seizures.
A diagnostic criteria proposed by Gutelkin is used in the diagnosis of paraneoplastic limbic encephalitis [9]. They are (i) a clinical picture of short-term memory, loss, seizures, or psychiatric symptoms suggesting involvement of the limbic system; (ii) an interval of < 4 years between the onset of neurological symptoms and the cancer diagnosis; (iii) exclusion of other cancer-related complications (metastasis, infection, metabolic and nutritional deficits, cerebrovascular disorder or side-effects of therapy) that may cause symptoms of limbic dysfunction; and (iv) at least one of the following: CSF with inflammatory changes (pleocytosis, oligoclonal IgG bands); MRI showing unilateral or bilateral temporal lobe abnormalities; and EEG showing slow- or sharp-wave activity in one or both temporal lobes. Employing the above mentioned criteria, paraneoplastic limbic encephalitis secondary to midgut carcinoid was considered as a possible explanation for seizure and behavioural changes in our case. Here, patient fulfilled the first three criteria and the last criteria could not be investigated as he underwent debulking of cancer which is considered to be the effective modality of treatment for paraneoplastic syndromes.
Conclusion
Paraneoplastic limbic encephalitis is a rare presentation in neuroendocrine tumors. There are only few cases reported in tumors of midgut origin. Though various diagnostic tools are available, knowledge of this entity and high index of clinical suspicion is mandatory for diagnosis and effective patient management. Given the rarity, documentation of this disorder and compilation of statistics is essential in creating awareness and forming guidelines for identification and treatment of paraneoplastic limbic encephalitis.
[1]. IM Modlin, MD Shapiro, M Kidd, G Eick, Siegfried oberndorfer and the evolution of carcinoid diseaseArchives of Surgery 2007 142(2):187-97. [Google Scholar]
[2]. G Kloppel, Oberndorfer and his successors: from carcinoid to neuroendocrine carcinomaEndocrine pathology 2007 18(3):141-4. [Google Scholar]
[3]. SM Williams ED, The classification of carcinoid tumoursLancet 1963 1:238-9. [Google Scholar]
[4]. IM Modlin, KD Lye, M Kidd, A 5-decade analysis of 13,715 carcinoid tumorsCancer 2003 97(4):934-59. [Google Scholar]
[5]. CG Moertel, WG Sauer, MB Dockerty, AH Baggenstoss, Life history of the carcinoid tumor of the small intestineCancer 1961 14:901-12. [Google Scholar]
[6]. S Mocellin, D Nitti, carcinoid Gastrointestinal, epidemiological and survival evidence from a large population-based study (n = 25 531). Annals of oncology; Official Journal of the European Society for Medical Oncology/ESMO 2013 24(13):3040-4. [Google Scholar]
[7]. J Datta, NB Merchant, Terminal ileal carcinoid tumor without hepatic or extrahepatic metastasis causing carcinoid syndromeThe American Surgeon 2013 79(4):439-41. [Google Scholar]
[8]. P Hellman, T Lundstrom, U Ohrvall, B Eriksson, B Skogseid, K Oberg, Effect of surgery on the outcome of midgut carcinoid disease with lymph node and liver metastasesWorld Journal of Surgery 2002 26(8):991-7. [Google Scholar]
[9]. SH Gultekin, MR Rosenfeld, R Voltz, J Eichen, JB Posner, J Dalmau, Paraneoplastic limbic encephalitis: neurological symptoms, immunological findings and tumour association in 50 patientsBrain; a journal of neurology 2000 123:1481-94. [Google Scholar]