Primary Cavernous Haemangioma of the Thyroid - A Case Report
Anuja Dasgupta1, S Teerthanath2, Meera Jayakumar3, Kiran HS4, Mary Raju5
1Postgraduate, Department of Pathology,KS Hegde Medical Academy, Mangalore, India.
2Professor, Department of Pathology,KS Hegde Medical Academy, Mangalore, India.
3Postgraduate, Department of Pathology,KS Hegde Medical Academy, Mangalore, India.
4Postgraduate, Department of Pathology,KS Hegde Medical Academy, Mangalore, India.
5Postgraduate, Department of Pathology,KS Hegde Medical Academy, Mangalore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anuja Dasgupta, Postgraduate, Department of Pathology, KS. Hegde Medical Academy, Mangalore-575018, India.
Phone: 9902336642,
E-mail: for_frendz@hotmail.com
Primary thyroid haemangioma is extremely rare, with only countable cases having been previously reported. We are reporting a case of 38-year-old male with history of diffuse thyroid swelling in front of the neck, which was firm to hard in consistency. Ultrasonography (USG) displayed an enlarged left thyroid with anechoic / isoechoic nodule and foci of coarse calcification. Preoperative clinical diagnosis of solitary thyroid nodule was made. Fine Needle Aspiration Cytology (FNAC) was inconclusive, due to bloody aspirate. Left hemi-thyroidectomy was performed. Haemangioma was diagnosed, based on histopathological examination findings. Surgical excision would be the treatment of choice, which provides a good prognosis.
Benign vascular neoplasm, Hemi-thyroidectomy
Case Report
A 38-year-old male presented with history of swelling in front of the neck of one year’s duration, which had slowly increased to the present size of 4 x 5 cm. He had no other symptoms which suggested functional thyroid disease. There was no history of pain over the swelling, change in voice or dyspnoea. There was no past history of trauma, previous fine-needle aspiration biopsy, or other surgical procedures. Patient was moderately built and nourished. Clinical examination of the neck revealed a mobile, diffuse thyroid swelling which measured about 4 x 5 cm, and was firm to hard in consistency. The patient was euthyroid and he showed no signs of hyper or hypothyroidism. Thyroid profile was within normal limits. Haematological and biochemical investigations were also within normal limits.
USG of neck revealed an enlarged thyroid. The left lobe of the thyroid measured 6 x 3.5 x 5 cm, with a well-defined anechoic / isoechoic nodule, with foci of coarse calcification. The right lobe of thyroid measured 4.1 x 1.6 cm and isthmus was 2 mm. The common carotid artery was displaced posteriorly. FNAC of the mass was inconclusive, as the aspirate was bloody. Pre-operative clinical diagnosis of solitary thyroid nodule was made.
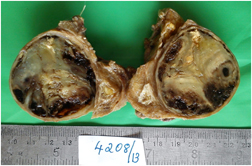
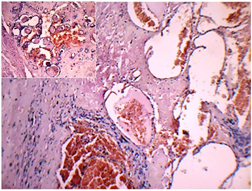
A left hemi-thyroidectomy was performed, and specimen was sent for histopathological evaluation. The specimen which was received was grey brown, globular, soft tissue mass and measured 6 x 5 x 3 cm. Cut-section revealed a well-encapsulated circumscribed lesion which measured 4.5 x 4 cm, and consisted of dark brown haemorrhagic areas, with irregular areas of fibrosis, myxoid change, foci of calcification and bone formation [Table/Fig-1]. The surrounding thyroid appeared normal. Microscopic examination revealed thyroid with a well encapsulated lesion, composed of large cavernous vascular spaces, with areas of haemorrhage, fibrosis, hyalinization, calcifications and bone formation [Table/Fig-2]. The surrounding thyroid tissue appeared normal. The final histological diagnosis of cavernous haemangioma of thyroid was made.
Gross Well-encapsulated circumscribed lesion, consisting of dark brown hemorrhagic areas, with irregular areas of fibrosis, myxoid change, foci of calcification and bone formation.
Cavernous spaces with blood and areas of fibrosis. Inset: Thyroid follicles admixed with vascular spaces (H&E X100)
Demographic and clinical characteristics of patients with primary thyroid hemangioma F, Female; M, Male; US, United States
| Patient | Country | Age (year) | Sex | Location | Size (cm) | Authors, year published |
| 1 | US | 56 | M | Left | 7.5 x 3 x 2 | Pickleman, [5] |
| 2 | India | 53 | M | Right | 6 x 3.5 | Pendse, [6] |
| 3 | India | 53 | M | Right | 4 x 4 | Kumar, [7] |
| 4 | Spain | 48 | F | Left | 5 x 4 | Rios, [8] |
| 5 | Spain | 63 | F | Left | 5 x 4 | Rios, [8] |
| 6 | Japan | 21 | M | Right | 5.5 x 3 x 2 | Kano, [9] |
| 7 | Korea | 66 | M | Left | 17 x 16.5 | Lee, [10] |
| 8 | Turkey | 64 | M | Right | 7 x 6 x 6 | H. Ciralik, [4] |
| 9 | India | 25 | M | Left | 4.9 x 4.4 | Datta R, [1] |
| 10 | Japan | 71 | F | Left | 5.2 x 4.8 x 3.5 | Akihiro Sakai, [2] |
| 11 | Greece | 78 | M | Right | 4 x 4 | Michalopoulos, [11] |
| 12 | Brazil | 80 | F | Left | 22 x 21 x 17 | Maciel LM, [3] |
| 13 | Switzerland | 84 | F | Left | | Gutzeit A, [12] |
| 14 (our case) | India | 38 | M | Left | 6 x 5 x 3 | 2 |
Discussion
Haemangiomas are common benign vascular tumours which are seen in childhood[1]. Majority of the cases (65%) develop in head and neck region [2]. Primary thyroid haemangiomas are extremely rare and are considered to be a developmental anomaly which result from the inability of the angioblastic mesenchyma in forming canals [1-3]. They usually follow trauma or fine-needle aspiration biopsy, and arise from vascular proliferations that follow the organization of a haematoma [3]. They clinically present as asymptomatic cervical tumours, are occasionally fast-growing, especially if intra tumoural bleeding is present [1]. These tumours have diameters of 20 and 40 mm [4]. Making a diagnosis before surgery is difficult. Haemangioms should be considered in the diagnosis of any pulsatile mass which involves the thyroid gland [2].
Only 13 cases of primary thyroid haemangiomas have been published in the literature, which have been mentioned below. The location of the tumour predominantly in left lobe of thyroid, with a slightly higher predilection in males and the size of the lesion, were consistent with findings of various reported cases [Table/Fig-3].
Haemangiomas, on USG, show hypoechoic areas with calcifications within the thyroid gland, without specific, distinct characteristics [3]. The clinical finding of the hard nature of mass with associated calcifications, often points to a malignancy. Coarse calcifications, when they are present, are suggested as a reliable sign of the presence of a haemangioma [3].They may be hard in consistency, due to the presence of phleboliths within the tumour. Though they are unusual, it is often the only reliable sign of a rare haemangioma in the thyroid [1]. Shpitzer et al., have suggested MRI, single photon emission computed tomography (SPECT), digital subtraction angiography (DSA) and red blood cell (RBC) scans for the pre-operative diagnosis of haemangiomas [13]. The presence of heterogenous signal intensity and serpentine pattern on MRI is considered to be highly suggestive of cavernous haemangioma [1]. Pickleman et al., performed angiography to identify the feeding blood vessel which was distributed from the inferior thyroid artery, and they diagnosed haemangiomas before surgery [5]. A Tc-99m erythrocyte blood-pool imaging has been suggested, to confirm diagnosis of haemangiomas [1]. FNAC is essential for the diagnosis of thyroid tumours in most of the cases. However, the specimens of haemangioma will contain only blood components as a feature. Therefore, they will be inconclusive to opine [2].
Surgical treatment is indicated when there is a suspicion of malignancy or when there is presence of compressive symptoms. Hemi-thyroidectomy or total thyroidectomy could be the treatment of choice [4].
To conclude, primary haemangioma of thyroid is rare, which predominantly affects the left lobe, which has an average size of 4 to 5 cm, and a predilection in males. Pre-operative diagnosis is difficult, as there are no specific pathognomic findings on radiological investigations or FNAC. A differential diagnosis can be considered when the abundant blood flow is aspirated. Surgery is the treatment of choice and it provides a good prognosis. A definitive diagnosis can only be achieved by doing postoperative pathological examination.
[1]. R Datta, MD Venkatesh, A Nilakantan, B Joseph, Primary cavernous hemangioma of thyroid glandJ Postgrad Med 2008 54:147-48. [Google Scholar]
[2]. Sakai Akihiro, Sugitani Iwao, Yamamoto Noriko, Kawabata Kazuyoshi, Hemangioma of the ThyroidClinical Medicine: Ear Nose and Throat 2009 :7-12. [Google Scholar]
[3]. LM Maciel, PM Gomes, PK Magalhães, FV Mello Filho, LC Conti-Freitas, A giant primary hemangioma of the thyroid glandJ Clin Endocrinol Metab 2011 96:1623-24. [Google Scholar]
[4]. H Ciralik, R Citil, E Bulbuloglu, S Bakaris, A patient with a neck massNeth J Med 2008 66(1):38-39. [Google Scholar]
[5]. JR Pickleman, JF Lee, FH Straus, E Paloyan, Thyroid hemangiomaAm J Surg 1975 129:331-33. [Google Scholar]
[6]. AK Pendse, KK Porwal, Solitary primary hemangioma of thy thyroidJ Indian Med Assoc 1998 :96-190. [Google Scholar]
[7]. R Kumar, R Gupta, A Khullar, S Ramirez, B Dasan, A Malhotra, Thyroid hemangioma: a case report with a review of the literatureClin Nucl Med 2000 25:769-71. [Google Scholar]
[8]. A Ríos, JM Rodríguez, E Martínez, P Parrilla, Cavernous hemangioma of the thyroidThyroid 2001 11:279-80. [Google Scholar]
[9]. M Kano, K Kameyama, Y Hosoda, K Sugino, K Ito, A cavernous haemangioma of the thyroid glandJ Laryngol Otol 2005 119:828-30. [Google Scholar]
[10]. J Lee, JS Yun, KH Nam, WY Chung, CS Park, Huge cavernous hemangioma of the thyroid glandThyroid 2007 17:375-76. [Google Scholar]
[11]. NV Michalopoulos, H Markogiannakis, PB Kekis, E Lagoudianakis, A Manouras, Primary cavernous hemangioma of the thyroid glandSouth Med J. 2012 103:674-75. [Google Scholar]
[12]. A Gutzeit, G Stuckmann, I Tosoni, D Erdin, CA Binkert, A cavernous hemangioma of the thyroid gland: First documentation by ultrasound of a rare pathologyJ Clin Ultrasound 2011 39:172-04. [Google Scholar]
[13]. T Shpitzer, AM Noyek, I Witterick, T Kassel, M Ichise, P Gullane, Noncutaneous cavernous hemangiomas of the head and neckAm J Otolaryngol 1997 18:367-74. [Google Scholar]