Background: The thoracolumbar junction is the most common area of injury to the axial skeleton. Forces along the long stiff kyphotic thoracic spine switch abruptly into the mobile lordotic lumbar spine at the thoracolumbar junction. Goals of treatment are to obtain a painless, balanced, stable spine with optimum neurological function and maximum spine mobility. The present prospective study has evaluated the effectiveness of pedicle screw instrumentation in various fractures around the TL spine to overcome the complications encountered in the conservative line of management of these fractures.
Materials & Methods: Thirty cases of fractures around the TL spine were operated with posterior pedicle screw fixation one or two level above and below the fracture. The cases were followed up for a mean of 9.5 months with radiological and neurological evaluation.
Results: The average age groups of the patients studied were 21 to 53 years majority were males, fall from height being the predominant mode of injury involving the T12 and L1 vertebral body. The unstable burst fractures the most common type of fracture, radiological parameters sagittal angle and index were recorded pre and post-operatively. The neurological grading was done using the ASIA score. Follow-up was done for a minimum of 5 months where sagittal angle reduction achieved was 10.75 at final follow-up from 23.5 pre-operative. The sagittal index achieved at final follow-up was 72% compared to the pre-operative mean of 53%. The neurological improvement was regarded to be fair enough for the type of injury sustained and fixation achieved.
Conclusion: We found that the application of posterior instrumentation using pedicle screw and rod resulted in a reasonable correction of the deformity with a significant reduction in recumbency-associated complications; the limiting factor being the small study group and short follow-up period.
Thoracolumbars, pedicle screw and rod instrumentation
Introduction
The thoracolumbar junction is the most common area of injury to the axial skeleton. Forces along the long stiff kyphotic thoracic spine switch abruptly into the mobile lordotic lumbar spine at the thoracolumbar junction. Biomechanically, this transition zone is susceptible to injury and is the most commonly injured portion of the spine, motor vehicle accidents are the leading cause of injury followed by falls and sports related injuries [1].
Males are at four times higher risk than females. Other organ system injury is encountered in up to 50% of thoracolumbar trauma patients [2]. Injuries such as those causing thoracic level paraplegia, have a mortality rate of 7% [3].
The goals of treatment are to obtain a painless, balanced, stable spine with optimum neurological function and maximum spine mobility. Significant controversy exists about the best method of treatment to achieve these goals.
Stability of the spine determines the method of treatment. Mc Afee et al., classification gives us the complete picture over the stability of spine, He proposed that the mechanism of failure of middle column, by axial compression, axial distraction or translation could be determined which would influence the stability.
Wedge Compression Fractures – Cause isolated failure of anterior column results from forward flexion, rarely associated with neurological deficits.
Stable Burst Fractures – Only anterior and middle.
Unstable Burst Fractures – Anterior and middle column fail in compression, the posterior column is also disrupted due to compression, lateral flexion or rotation.
Chance Fractures – Horizontal avulsion fractures of the vertebral body caused by flexion around as axis anterior to the anterior longitudinal ligament.
Flexion Distraction Injuries – Anterior column fails on compression, middle and posterior column in tension, flexion axis is posterior to the anterior longitudinal ligament.
Translation Injuries – All three columns have failed in shear, there ismalignment of the neural canal in the transverse plane.
All unstable fractures needs surgical intervention.
The advantages of surgical treatment with pedicle screw and rod fixation systems in spine injuries are shorter hospital stay, more complete rehabilitation, fewer complications of prolonged immobilization and reduced morbidity and mortality. Hence there is a need for study to delineate the benefits of this procedure on the functional outcome of the patients.
Aims and Objectives
1. To evaluate the restoration of the alignment of the spine and spinal canal.
2. To aid in early mobilization.
3. To evaluate the improvement of neurological level according to ASIA scale.
Materials and Methods
The study was conducted between March 2011 to September 2012, 30 patients in our institute were operated for unstable thoraco lumbar fractures with pedicle screw fixation and posterior decompression and were followed up for 5 to 18 months (mean -9.5 months). Exclusion criterion was those who had stable thoracolumbar fractures, medically unfit and not willing for surgery. After a detailed examination consisting of a detailed history pertaining to mode of injury and time of injury was taken, clinical examination which included general examination for head, cervical spine, chest, abdominal injury was completed.
Then after the patient was stabilized, examination of the spine with neurological evaluation for motor power, sensory, reflexes examination of the spine with neurological evaluation for motor power, sensory, reflexes and bowel-bladder was done to evaluate the level of spine injury and extent of cord damage following the American Spinal Injury Association of neurological evaluation.
A radiograph of the injured spine in two views was done to classify the fracture type using the MacAfee’s system of classification [4]. In cases with associated injuries additional radiographs were included to rule out fractures.
Patients with neurological involvement caused by the fracture, all neurologically stable or unstable patients with instability criteria of kyphotic deformity (sagittal angle) more than 200, loss of vertebral body height (sagittal index) of more than 50% were considered to have an indication for surgical stabilization of the spine.
Patients were operated between 1 to 23 days of injury surgical interval with a mean of 5.5 days.
Surgery delayed in few cases due to delay in reporting to hospital. MRI scan was taken routienly in all cases and status of spinal cord was corresponding with the ASIA scale, three cases had almost complete injury of spinal cord. For all cases posterior approach was used. Primarily stabilization was done using pedicle screw-rod system under C arm guidance and followed by decompression of the cord with laminectomy of the injured segment and if required adjacent segments. Bone grafts were placed at posterolateral aspect in all the cases taken from the cut removed spinous proceses. The mean surgical interval was 3 hours, ranging from 2 to 4 hours.
Post-operative: patients were administered intravenous antibiotics for 3-5 days, and then oral preparations were continued for another five days. They were allowed to lie on both right and left lateral positions in the immediate post-operative period. Drainage tubes were removed within 48 hours of surgery. Check radiographs were taken for evaluation of fracture reduction; implant position, kyphotic angle and correction of vertebral height. All patients were started on a rehabilitation program with the passive mobilization of lower limb joints and to teach the patient attender regarding bed care and strengthening of muscles. Thoraco-lumbo-sacral orthosis were prepared for adequate bracing. Patients were made to sit on the third - fifth day with his braces on. Suture removal performed at 12th day. Bladder training was begun on the 7th day if patients obtained control, catheter was removed and discharged, if not patients were taught self catheterization. Bowel evacuation was taught by tickling the perianal region or by digital evacuation.
Rehabilitations were started immedietly after surgey.
Post-operative follow-up done every month for first six months, then after once in three months for first year, then after once in six months with clinical evaluation and radiological assessment. At every follow-up symptomatic history pertaining to pain relief, his level of activities and bowel-bladder function is taken. Clinical examination for deformity and neurological grading using the ASIA criteria is done. Radiographs are taken for evaluation of the fixation, sagittal angle and index calculation. The cases with incomplete injuries/paraplegia were strictly restricted of activities for 4 weeks and all patients advised to continue TLSO brace for over 10 weeks. Patients with complete injuries/paraplegia were confined to bed to prevent early re-collapse and mobilized depending on the radiographic evidence of fracture consolidation. They were mobilized using wheelchair mobilization.
Results
The study included 30 cases of which 24 (80%)were males and 6 (20%) females. The mean age of the study population was 33.5 years. The most common mode of injury in the study group was fall from a height in 23 cases (76.6 %) followed by road traffic accidents in 7 cases (23.4%). In our study we observed that 21 cases (70%) the site of injury was at L-1 level, 6 cases (20%) were at L-2 level 3 cases with fracture at T-12 ( 10%) [Table/Fig-1]. The most common type of fracture observed in the study was unstable burst fracture with 25 cases (83.3%) followed by 4 cases (13.3 %) with flexion distraction injury [Table/Fig-2]. The radiological evaluation of sagittal angle and sagittal index was done pre-operatively, post- operatively and at final follow-up. Pre-operative sagittal angle was 23.5 0 post operative sagittal angle was 10.75 0 and at the final follow-up the loss of angle was 4.80. Pre-operative sagittal index was 0.53, post operative 0.75 and at final follow up was 0.72. Neurological evaluation was done according to American Spinal Injury Association scale in the pre-operative period and at all follow-ups [Table/Fig-3,4,5]. Twenty-six cases (86.7%) were improved, in that 17 (56.6%) cases showed one grade improvement, 8 (26.6%) showed two grade improvement and one (3.33%) improved three grade. 4 cases (13.33%) fail to recover any grade [Table/Fig-3].
| Level | No. of Cases | Percentage |
|---|
| T 12 | 3 | 10% |
| L 1 | 21 | 70% |
| L 2 | 6 | 20% |
| TOTAL | 30 | 100% |
| Type | No. of Cases | Percentage |
|---|
| Unstable Burst Fracture | 25 | 83.33% |
| Flexion Distraction Injury | 4 | 13.33% |
| Translation Injury | 1 | 3.33% |
Neurological evaluation/assesment
| Nuerological Examination | Follow Up |
|---|
| Pre-operative | A | B | C | D | E |
| A | 5 | 4 | 1 | | | |
| B | 3 | | | 1 | 1 | 1 |
| C | 21 | | | | 14 | 7 |
| D | 1 | | | | | 1 |
| E | 0 | | | | | |
Pre-operative MRI scan – T 12 burst fracture

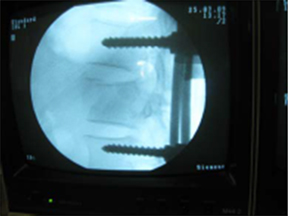
Mean duration of injury- surgery interval was 5.1 days. The common complication associated in the study was bed sores and urinary tract infections accounting for 4 cases (13.3%) each followed by implant failure which was seen in 3 cases (10 %), in that 2 cases had screw broken one case at third month due to improper use of the brace, for that revision done with additional segment fixation with bone grafting. One more screw broken at seventh month due to fall, treated conservatively. One case had connecting rod slippage with pedicle screw noticed at 16 month, for that nothing has been done [Table/Fig-6,7,8].



Discussion
The finding of the present study of mean age being 33.5 years is consistent with studies by Roy Camille et al., [5] who reported a mean age of 30. The predominance of fall from height as the mode of injury ( 76.6 %) is comparable to the findings of study by Dipankar and Patro [6] which reported 64.7%. Level of fracture in this study were around T12 and L1 constitute 80% comparable with the study by Dipankar and Patro which is 82%. Fifty-eight unstable burst fracture being the commonest type in 83.3% (23 cases) comparable with Gertzbein study with 68% [6,7]. Radiological evaluation of the cases in this study for sagittal angle was pre-operatively 23.50, post-operatively 10.750 and at final follow up the loss of angle was 4.8 comparable with the similary study by Mohammad F Butt et al., reported sagittal angle pre-operatively 21.40, post operative 12.8 and loss of angle at final follow-up 3.40 [8].
Nuerological evaluation done using American Spinal Injury Association scale in that out of 30 patients 26 (86.7%) were improved, in that 17 (56.6%) cases showed one grade improvement, 8 (26.6%) showed two grade improvement and one (3.33%) improved three grade. Four cases (13.33%) fail to recover any grade.
Over all complications occurred in 11 (36.6%) cases in that 4 cases had bed sore, 4 cases had urinary tract infection and 3 cases had implant failure in the form of breakage are comparable with Mohammad M Butt et al., [8] study recorded 50% complications.
Management of spinal injury is usually considered an extremely difficult and demanding job when considered in respect of infrastructural support in the hospitals of developing countries. However we find that the results of this study is comparable with similar other studies in most aspects although we have used locally manufactured implants which is much cheaper than the standard latest implants and this is particularly significant when considering the socio-economic structure of our country.
Conclusion
Fracture and fracture dislocations of the thoracolumbar spine are the most commonly occurring types of osseous spine injury. In the developed countries road traffic accidents causing the major percentage and fall from height being the commonest mode of injury in the developing countries. The main aim of the treatment resides in early stabilization, direct or indirect decompression of the neural elements and early mobilization of the patient to prevent complications. This also avoids the burden on the family of the patients and the care givers and reduces the hospital stay compared with that of conservative means of treatment.
Unstable burst fractures were the most common fracture type encountered in the study which leads to deformity and neurological compromise. The radiological and neurological evaluations were the parameters taken into account to assess the instability and indication for surgery and recovery. There was marked improvement in the radiological parameters comparable to other studies done in both Western and Asian countries. The neurological improvement was observed to be fair enough in cases of incomplete neurological injury.
Short segment fixation using the posterior approach with pedicle screw-rod fixation devices with or without bone grafting achieves good stabilization and fair enough neurological recovery in patients with unstable thoracolumbar fractures. The limiting factors being a small study group and shorter follow-up period.
[1]. Price C, Makintubee S, Herdon W, Istre GR, Epidemiology of traumatic spinal cord injury and acute hospitalization and rehabilitation changes for spinal cord injuries in OklahomaAMJ Epidemiol 1994 139:37-47. [Google Scholar]
[2]. Colter JM, Vernace Jr, Michalski JA, The use of Harrington rods in thoracolumbar fracturesOrthop Clin North Am 1986 17:87-103. [Google Scholar]
[3]. Shikala J, Yamamuro T, Iida H, Shimiruk Yoshikawa J, Surgical treatment for paraplegia resulting from vertebral fractures in senile osteoporosisSpine 1990 15:485-89. [Google Scholar]
[4]. McAfee PC, Yuan H, Fredrickson BE, Lubicky JP, The value of computed tomography in thoracolumbar fracturesJ Bone Joint Surg (Am) 1983 65(4):461-73. [Google Scholar]
[5]. Roy Comille, Saillant G, Mazel C, Internal fixation of the lumbar spine with pedicle screw platingClin Orthop 1986 203:7-17. [Google Scholar]
[6]. Dipankar Sen, Patro DK, Management of unstable spine fracture with segmental instrumentation: Result at 5 years follow upIndian Journal of Orthopaedics 2005 39:232-36. [Google Scholar]
[7]. Gertzbein SD, Brown CMC, Marks P, Martin C, Fazl M, Schwartz M, Jacobs RR, The neurological outcome following surgery for spinal fracturesSpine 1988 13:641-44. [Google Scholar]
[8]. Butt Mohammad F, Farooq Munir, Mir Bashir, Dhar Ahmad Shabir, Management of unstable thorocolumbar injury by posterior short segment spinal fixationInt Orthop 2007 31(2):259-64. [Google Scholar]