Spinal anaesthesia is one of the most suitable modality of anaesthesia for lower abdominal surgeries. The advantages of subarachnoid block are limited by its short duration of action and side effects such as hypotension and bradycardia resulting due to sympathetic blockade. In recent years, the supplementation of local anaesthetics with adjuvants is widely in practice, to reduce the dose of local anaesthetic, minimize side effects and prolong the duration of anaesthesia [1,2].
Opioids are the time honoured drugs which have been used for this purpose. Morphine was the first opioid used intrathecally in 1979, followed by other opioids [3–5]. Buprenorphine is a centrally acting lipid soluble analogue of alkaloid thebaine. It exhibits analgesic property both at spinal and supraspinal levels [6]. It has been used for various surgeries at different doses for the past few decades. It has consistently proven to prolong the duration of anaesthesia [1,2,7]. At higher doses, it causes pruritus, drowsiness, nausea and vomiting [8].
There are no studies in the literature comparing the benefits and side effects of the drugs buprenorphine and dexmedetomidine as adjuncts to bupivacaine for lower abdominal surgeries. Hence, we undertook this study to investigate and compare buprenorphine and dexmedetomidine as an adjuvant to hyperbaric bupivacaine for efficacy, hemodynamic stability, post-operative analgesia and side effects.
Materials and Methods
This prospective randomized double blind study was conducted in a Medical College Hospital following approval of ethics committee. Informed written consent was obtained from 60 patients posted for elective lower abdominal surgery requiring subarachnoid block. Inclusion criteria were age 18-60 years of either sex belonging to American Society of Anaesthesiologists Physical Status I and II. Patients with bleeding disorders, on anticoagulant therapy, cardiac disease, heart blocks, dysarrythmias, β-blockers and α-antagonists were excluded from the study. They were randomized by computer generated random number sequence and sealed envelope technique into two groups: Group B and Group D of 30 each.
Group B received 60µg of buprenorphine with 3cc (15mg) of 0.5 % heavy bupivacaine
Group D received 5µg of dexmedetomidine with 3cc (15mg) of 0.5 % heavy bupivacaine.
The drug solution was prepared by an anaesthesiologist not involved in the study.
All patients were kept nil per oral for 8 hours and premedicated with tablet diazepam 0.1mg/kg orally on the night before the surgery and in the morning. Injection atropine 0.6mg was administered Intramuscular (IM) to all patients 30 minutes before procedure. On arrival to the operation room (OR), intravenous access was started and patients preloaded with 10ml/kg of crystalloid over 15 minutes. Patient monitoring included Non Invasive Blood Pressure (NIBP), pulse oximetry and three lead electrocardiogram (ECG). The baseline systolic and diastolic blood pressures (SBP, DBP), heart rate (HR) and oxygen saturation (SpO2) were recorded.
Under strict aseptic precautions subarachnoid block was performed by 23G/25G Quincke Babcock spinal needle in the L3-L4 interspace in lateral position. The loaded drug was injected over 10-15 seconds following free flow of Cerebrospinal Fluid (CSF). The time at which injection was completed was considered zero time of the study and all measurements were recorded from this point. Following subarachnoid block, patients were made to lie supine. Sensory testing was done by pin prick method using 25G hypodermic needle and time taken to reach T8 level noted down. Motor block was assessed using Modified Bromage Scale (Bromage 0 – patient is able to move hip, knee and ankle; Bromage 1 – not able to move hip but able to move knee and ankle; Bromage 2 – not able to move hip and knee, but able to move ankle; Bromage – 3 not able to move hip, knee and ankle). The time taken to reach modified Bromage 3 was recorded. Sedation was assessed by Ramsay sedation scale on arrival to OR, 10 minutes post spinal anesthesia and post operatively. (Ramsay Sedation Scale: 1. Anxious, agitated; 2. Co-operative, oriented and tranquil; 3. Responding to commands; 4. Brisk response to glabellar tap; 5. Sluggish response to glabellar tap; 6. No response).
In cases with failure of subarachnoid block and conversion to general anaesthesia we planned to exclude such patients from the study. Haemodynamic variables were recorded at 1 minute, 3, 5, 7 and 10 minutes after the administration of subarachnoid block and every 5 minutes thereafter up to 45 minutes after the block. Hypotension was defined as fall in SBP 30% from baseline and was treated with intravenous fluids and injection Mephentermine in 3mg aliquots. Bradycardia was defined as HR <50 beats per minute and treated with intravenous atropine 0.6 mg. Patients did not receive any additional analgesic in intraoperative period while anxious patients received intravenous midazolam 1mg. The incidence of any adverse effects such as hypotension, bradycardia, shivering, nausea, vomiting, pruritis, respiratory depression and ECG changes were noted.
Post-operatively the haemodynmic variables and oxygen saturation was recorded in the post anaesthesia care unit until complete recovery of the patients from anaesthesia. Duration of analgesia was taken from the time of intrathecal drug administration to the first supplementation of rescue analgesic when patient complained of pain. Injection Tramadol 1mg/kg intravenous was administered as a rescue analgesic. All patients were followed up for 1 week post surgery for headache, dysesthesia in thighs, buttocks or lower limbs.
Statistical Analysis
Statistical analysis was done by using Statistical Package for Social Science (SPSS 16.0 Evaluation version). Data expressed as mean and standard deviation. Chi-square test or Fisher’s test was used wherever appropriate. P-value < 0.05 was considered significant.
Results
The groups were comparable in terms of age, sex, weight, height, co-morbidities, type and duration of the surgery [Table/Fig-1]. The characteristics of subarachnoid block between the two groups are shown in [Table/Fig-2]. Group D had prolonged sensory and motor blockade with higher sedation scale.
| Variable | Group B (n=30) | Group D (n=30) | p-value |
|---|
| Age (years)* | 42.60±9.81 | 46.60±12.26 | 0.22 |
| Sex (M:F) | 10:20 | 11:19 | 0.79 |
| Duration of surgery (minutes)* | 91.67±25.20 | 95.43±38.10 | 0.06 |
| Type of surgery | Total abdominal hysterectomy | 16 | 13 | 0.25 |
| Inguinal hernioplasty | 14 | 17 |
| Height (centimetres)* | 157.46±7.48 | 161.06±7.38 | 0.66 |
| Weight (kilograms)* | 70.38±7.34 | 62.9±11.63 | 0.11 |
| Comorbidities | Diabetes Mellitus | 4 | 8 | 0.07 |
| Hypertension | 4 | 0 |
| Bronchial Asthma | 0 | 1 |
| Nil | 22 | 21 |
* Mean ± Standard deviation
| Parameters | Group B (n=30) | Group D (n=30) | p-value |
|---|
| Onset of sensory block (minutes)* | 3.26±0.9 | 3.52±0.9 | 0.76 |
| Onset of motor block (minutes)* | 3.30±0.97 | 3.90±0.89 | 0.97 |
| Time for Modified Bromage 0 (minutes)* | 205.17±63.0 | 413.4±27.38 | 0.002 |
| Duration of analgesia (minutes)* | 289.66±64.94 | 493.56±385.95 | 0.015 |
| Time for sensory regression to S1 (minutes)* | 225.9±64.94 | 451.4±270.19 | 0.002 |
| Degree of sedation | Sedation scale <3 | 28 | 8 | 0.001 |
| Sedation scale >3 | 2 | 22 |
| Requirement of additional sedation | 11 | 9 | 0.25 |
* Mean ± Standard deviation
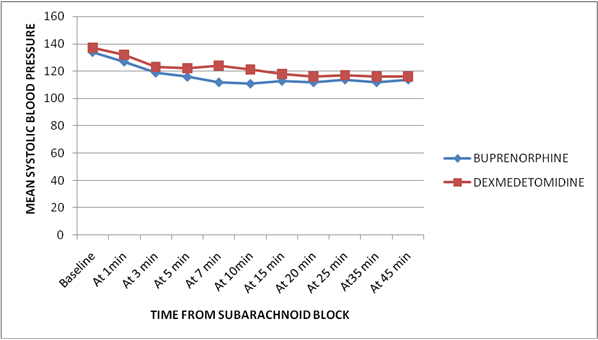
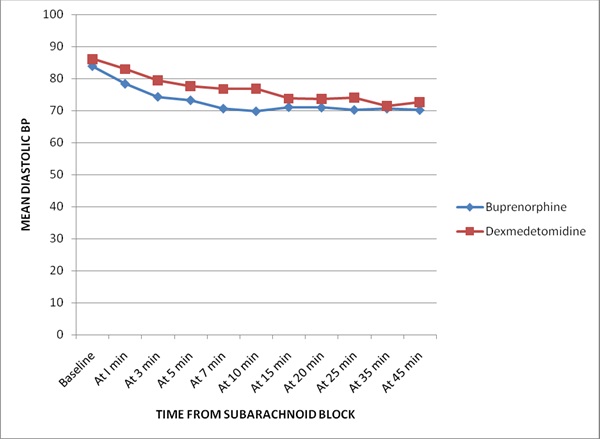
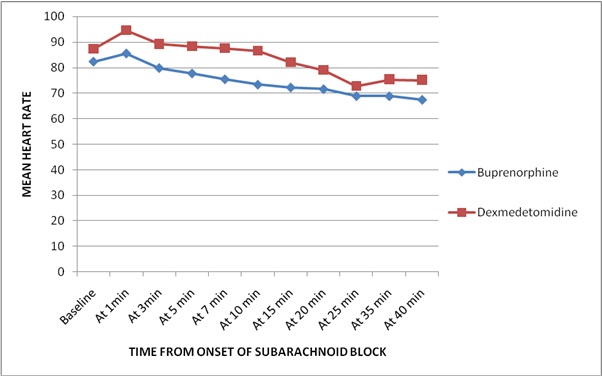
Side-effects and interventions required are shown in [Table/Fig-3]. No adverse effects like pruritis, ECG changes or respiratory depression were encountered in either of the two groups. There was no difference in SBP and DBP change over time between the 2 groups [Table/Fig-4&5]. The mean HR decreased over time in both the groups. It was lower in Group B when compared to Group D but the difference was statistically insignificant [Table/Fig-6].
Side effects and interventions
| Group B (n=30) | Group D (n=30) | p-value |
|---|
| Nausea/Vomiting | 4 | 2 | 0.39 |
| Shivering | 2 | 5 | 0.12 |
| Mephenteramine required | 12 | 17 | 0.19 |
| Atropine required | 4 | 2 | 0.389 |
| Intravenous fluids | <1.5 litres | 7 | 2 | 0.023 |
| >1.5 litres | 23 | 28 |
* Mean ± Standard deviation
Mean systolic blood pressure
Mean diastolic blood pressure
Discussion
A revolution has occurred in the management of post-operative pain since the understanding of its neurobiology and pharmacology of the available drugs for the control of pain.
Buprenorphine is a centrally acting partial opioid agonist with both spinal and supraspinal component of analgesia [6]. Recently it has been found that buprenorphine has a local anaesthetic action, this mechanism may be responsible for prolonging the anaesthesia associated with buprenorphine [12]. It is highly lipid soluble and diffuses quickly into neural tissue, decreasing the chances of rostral spread leading to lesser side effects in the post-operative period [8].
Dexmedetomidine is a highly specific α-2 adrenergic agonist [2]. It prolongs sensory block by acting on presynaptic C fibres and decreasing the neurotransmitter release. It acts on postsynaptic dorsal neurons causing their hyperpolarisation. It prolongs motor block by binding to motor neurons in the spinal cord [13,14]. Celik et al., found that intrathecal Dexmedetomidine causes neuroprotective effect similar to methyprednisolone in rats following spinal cord injury [15].
The onset of sensory and motor block in our study was comparable with the studies done by Shukla et al., [16] and Shaikh and Kiran [1] for dexmedetomidine and buprenorphine respectively.
HR was decreased in both the groups following subarachnoid block. Although all our patients had received IM atropine prior to spinal anaesthesia, 6 patients (4 in Group B and 2 in Group D) had bradycardia, which needed intervention. Dexmedetomidine causes bradycardia but the effect is more prominent when administered intravenously and with a higher dose [17]. More number of patients required Intravenous mephentermine and greater intravenous fluids in dexmedetomidiene group, which was comparable with the more ephedrine requirement in previous studies on intrathecal dexmedetomidine [2].
Intravenous dexmedetomidine has anti shivering effect [18]. However, we encountered more incidence of shivering in dexmedetomidine group which implies that intrathecal dexmedetomidine has no effect on shivering. Although the incidence of nausea and vomiting was more in the buprenorphine group it was not significantly different between the two groups. Similar observation were done by Sapkal et al., while comparing clonidine 60µg with buprenorphine 60µg where incidence of nausea and vomiting was higher in buprenorphine compared to clonidine [19].
The duration of analgesia in the dexmedetomidine group in the present study was 493 minutes. This is in agreement with studies done by Shah et al., [13] where 5µg dexmedetomidine had a duration of analgesia 474 minutes. Similarly in the study done by Gupta et al., [9], duration of analgesia was significantly prolonged with the addition of 5µg dexmedetomidine to 478 minutes. Study done by Eid et al., [20] showed that duration of analgesia with dexmedetomidine is proportional to its dose. A meta-analysis of use of dexmedetomidine in regional anaesthesia states that the sensory duration, motor blockade and request for rescue analgesia is prolonged in dexmedetomidine group [21]. Buprenorphine group in our study had duration of analgesia as 300 minutes which is less than that stated by Shaikh and Kiran [1] and Capogna et al., [8] where the duration of analgesia was 475 minutes and 430 minute respectively in the buprenorphine group. This could be because Capogna studied elderly patients and the study of Safiya had included procedure of lower limb only.
The duration of motor block in our study was 440 minutes in the dexmedtomidine group which is in agreement with the studies done by Gupta et al., [9] where duration of motor block was 421 minutes. This is significantly prolonged in comparison to duration of motor block in the buprenorphine group 212 minutes. The sedation scale was higher in the patients belonging to dexmedetomidine group as compared to buprenorphine, so the need for further intraoperative sedation was less in dexmedetomidine group. This action of dexmedetomidine can be attributed to its action on the α-2 receptors in locus ceruleus.
We had to administer general anaesthesia following subarachnoid block for 5 patients who received dexmedetomidine and one patient who got buprenorphine due to failure of the spinal anaesthesia. These patients were excluded from the study. In our follow up of the patients post-surgery for one week, we did not encounter any incidence of headache; dysesthesia is buttocks, thighs or lower limbs.
Limitations
The limitations of our study were that we had not done a power calculation to derive at sample size.
Absence of a control group to compare the effect of drugs separately is lacking in our study.
The mean age group in our study was 42-47 years; the effect of intrathecal dexmedetomidine on older patients could not be assessed in the present study.
Recommendations
Future studies are needed to elucidate the cause of failure of subarachnoid block, the incidence of which was more in dexmedetomidine group as compared to buprenorphine group.
A dose finding study of intrathecal dexmedetomidine is lacking.
Studies concerning use of intrathecal dexmedetomidine in elderly patients with comorbidities needs to be investigated.
Conclusion
From present study it can be concluded that, the onset of sensory and motor blockade in both dexmedetomidine and buprenorphine were comparable. The duration of motor and sensory block in dexmedetomidine group was 413 minutes and 451 minutes which was significantly different from 205 minutes and 226 minutes of buprenorphine group. Similarly duration of analgesia was 493 minutes in dexmedetomidine group as compared to 289 minutes of buprenorphine group. Hence we concluded that intrathecal dexmedetomidine 5µg when compared to intrathecal buprenorphine 60µg causes prolonged duration of sensory and motor block. The requirement of additional sedation and rescue analgesia is less in dexmedetomidine group and the haemodynamics are similar in both the groups without causing any significant side effects.
* Mean ± Standard deviation
* Mean ± Standard deviation
* Mean ± Standard deviation