Women with previous cesarean sections constitute a highrisk group in obstetrics, with associated medical and legal implications. Vaginal birth after cesarean (VBAC) or trial of scar (TOS) represents a significant change in modern obstetric practice. However, the concern that a scarred uterus might end up in rupturing the uterus, leading to severe maternal and perinatal morbidity, still prevents a large number of obstetricians and pregnant women worldwide, from adopting a TOS after previous one cesarean section. In UAE, where having a big family is the social norm, TOS after a prior cesarean is more of a necessity than choice. Hence, it is not unusual to find more women attempting VBAC in this part of the world. This was the reason for choosing this particular study in the selected population.
Both, attempting a vaginal birth and opting for an elective repeat cesarean section (ERCS) are associated with different risks for the mother and newborn; and, deciding a delivery plan involves a difficult weighing of those cases [1]. For years, researchers have maintained an interest in the effective prediction or identification of factors, which can influence the outcome of a TOS. The ability to predict the outcome of an attempted trial of vaginal delivery plays an important role in initial counseling of pregnant women with previous one cesarean delivery. The study objectives were set in this context. The main aims of our study were to determine the outcome of pregnancy in women with prior cesarean section in relation to vaginal delivery, maternal and perinatal complications, and to identify the factors, which can influence the outcome of TOS.
Materials and Methods
This study was conducted in Mafraq Hospital, a tertiary care referral Centre in Abu Dhabi, UAE. Approval was obtained from the Ethics Committee, and a retrospective analysis of medical records of 151 women with previous one cesarean section who delivered during the time period (January–August 2011) was carried out. The exclusion criteria included women with previous classical cesarean section and those with extreme prematurity (less than 32 weeks).
We followed our Department protocols for managing high-risk pregnancies with previous cesarean sections. Women with previous uterine surgery involving the cavity, scar rupture or extension, those with inter-delivery interval of less than 18 months, and those with unknown scar type were booked for ERCS. The mode of delivery was planned during the antenatal visit to the clinic, usually by about 36 weeks after proper counseling. For un-booked patients, the decision was made when they reported to the labour ward. For those who planned for TOS, spontaneous onset of labour was awaited till 41 weeks and three days. Induction of labour was carried out by artificial rupture of membranes (ARM) and oxytocin or cervical balloon for indicated, suitable women. However, prostaglandins were not used for cervical ripening.
The raw data collected was analyzed using the SPSS software version 20. Maternal outcome was measured in terms of type of delivery (VBAC, ERCS, or Failed VBAC), occurrence of scar dehiscence (complete or partial), visceral injury, post-partum hemorrhage with the need for blood transfusion, uterine rupture, adherent placenta, hysterectomy, and maternal death.
Perinatal outcomes measures included Apgar levels, neonatal ICU admissions, and neonatal death.
Descriptive statistics were used to analyze the continuous and categorical data and presented in the form of mean, standard deviation and percentage, while proportions were analyzed using chi-square test. A p-value ≤0.05 was considered statistically significant.
Results
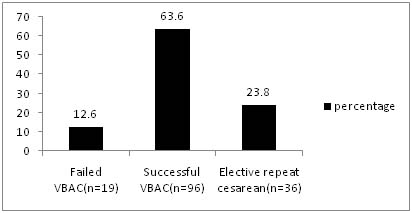
A total of 151 women with history of previous one caesarean delivery, were included in the study.Age of the patient population ranged from 21 to 42 years with a mean of 30.26 years, mode of 33 years and standard deviation of 5.60. Of the 151 women, 36 (23.8%) had ERCS, 96 (63.6%) had VBAC and 19 (12.6%) had failed TOS. In other words, 115 women had TOS with 83.4% VBAC rate and 16% failed trial [Table/Fig-1]. Among 96 successful vaginal deliveries, 89 women had spontaneous vaginal delivery while seven had assisted delivery with ventouse. Here, ventouse delivery was mainly used to cut short the second stage of labour, and that occurred in 5 cases (71.43%). The most common reason for ERCS was non-availability of previous operative notes [Table/Fig-2]. The other common indications included malpresentations, patient request and suspected cephalopelvic disproportion (CPD). About 5.6% women had history of posterior colpoperineorrhaphy, which prevented them from attempting a TOS for fear of disruption of vaginal repair site in the event of a vaginal delivery.
Mode of delivery in women with previous one cesarean (n=151). VBAC- Vaginal birth after cesarean delivery
Indications for elective repeat cesarean section (n=36)
| Number (n) | Percentage(%) |
|---|
| Operative notes not available | 17 | 47.22 |
| Big baby | 3 | 8.33 |
| Malpresentations | 5 | 13.88 |
| Patient request | 3 | 8.33 |
| Previous uterine incision extension | 2 | 5.56 |
| Previous rupture uterus | 1 | 2.78 |
| History of posterior repair | 2 | 5.56 |
| Short inter delivery interval | 1 | 2.78 |
| Twin pregnancy | 1 | 2.78 |
| IUGR | 1 | 2.78 |
| Total | 36 | 100 |
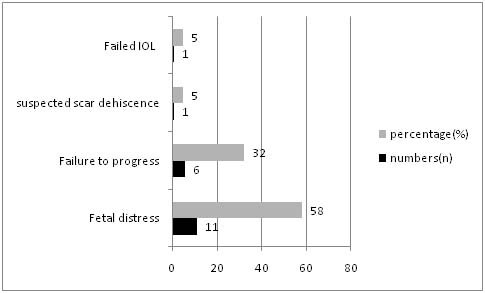
Out of 115 women, 19 who underwent TOS ended up in emergency cesarean deliveries. Fetal distress was the main reason in 11 women (58%) while the second common cause was failure to progress (32%) [Table/Fig-3].
Causes of failed trial of scar (n=19)
No significant association was observed between the indication for previous cesarean and the outcome of TOS [Table/Fig-4]. Similarly, body mass index (BMI) was also found to have no significant effect on the mode of delivery.
Indication of previous cesarean and mode of delivery in index pregnancy. χ2value-10.786, df-6, p-value 0.095
| Pregnancy outcome | Total |
|---|
| No Trial of scar | Successful VBAC | Failed VBAC |
|---|
| Previous Cesarean indication | Fetal distress | n | 8 | 33 | 8 | 49 |
| % | 16.33% | 67.34% | 16.33% | 100.0% |
| Failure to progress | n | 15 | 18 | 6 | 39 |
| % | 38.46% | 46.15% | 15.38% | 100.0% |
| Ante partum hemorrhage | n | 4 | 7 | 1 | 12 |
| % | 33.33% | 58.33% | 8.33% | 100.0% |
| Malpresen-tations | n | 9 | 38 | 4 | 51 |
| % | 17.65% | 74.51% | 7.84% | 100.0% |
| Total | n | 36 | 96 | 19 | 151 |
| % | 23.84% | 63.58% | 12.58% | 100.0% |
There was significant association between previous vaginal delivery and outcome of TOS [Table/Fig-5]. VBAC rate was 76.8% among those women with previous vaginal delivery compared to 41% in those who did not have a prior vaginal delivery (χ2 =20.143; p = 0.000). Among women with previous vaginal delivery, those with prior VBAC had 87.5% successful VBAC rate compared to 46% in those without a previous VBAC (χ2 =27.958; p = 0.000) [Table/Fig-6].
Effect of previous vaginal delivery on mode of delivery in women with a prior cesarean section(n=151). χ2value- 20.143, df-2, p-value- 0.000. VBAC-Vaginal birth after cesarean delivery
| Pregnancy Outcome | Total |
|---|
| No Trial of scar | Successful VBAC | Failed VBAC |
|---|
| Previous Vaginal Delivery | No | n | 23 | 23 | 10 | 56 |
| % | 41.07% | 41.07% | 17.86% | 100.0% |
| Yes | n | 13 | 73 | 9 | 95 |
| % | 13.68% | 76.84% | 9.47% | 100.0% |
| Total | n | 36 | 96 | 19 | 151 |
| % | 23.84% | 63.58% | 12.58% | 100.0% |
Previous VBAC and delivery outcome in index pregnancy. (χ2value-27.958, df- 2, p-value-0. 000) VBAC-Vaginal birth after cesarean delivery
| Pregnancy Outcome | Total |
|---|
| No Trial of scar | Successful VBAC | Failed VBAC |
|---|
| Previous Vaginal Delivery | No | n | 32 | 40 | 15 | 87 |
| % | 36.78% | 45.98% | 17.24% | 100.0% |
| Yes | n | 4 | 56 | 4 | 64 |
| % | 6.25% | 87.50% | 6.25% | 100.0% |
| Total | n | 36 | 96 | 19 | 151 |
| % | 23.84% | 63.58% | 12.58% | 100.0% |
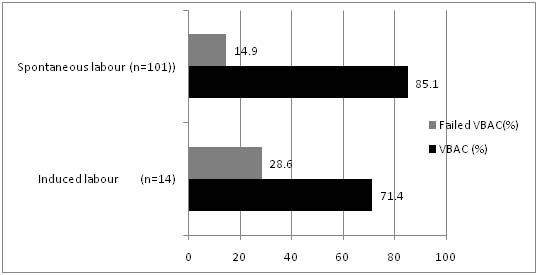
Women with spontaneous onset of labour had greater chances of VBAC (85.1%) compared to induced women (71.4%) (χ2 = 153.203; p = 0.000) [Table/Fig-7]. The chief methods of induction used were oxytocin, cervical ripening balloon, and artificial rupture of membranes.
Mode of onset of labour and delivery outcome in women who underwent trial of scar (n=115) (χ2 =153.203, df-2 p=0.000) VBAC- Vaginal birth after cesarean delivery
Average-sized babies (2.5–4.0 kg) had a successful vaginal delivery rate of 66.2%. Small for gestation babies (<2.5 kg) had a lower rate of VBAC (50%) while babies larger than 4 kg had an even lower success rate (20%). This was statistically significant (χ2 =15.275; p = 0.004) [Table/Fig-8].
Baby weights versus mode of delivery in index pregnancy. (χ2value- 15.275, df-4, p-value-0.004)
VBAC-Vaginal birth after cesarean delivery; LSCS-Lower segment cesarean section
| Mode of delivery | Total |
|---|
| NO trial of scar (Elective LSCS) | Successful VBAC | Failed VBAC |
|---|
| Baby Weight (Grams) (Grouped) | < 2500 | n | 5 | 5 | 0 | 10 |
| % | 50.0% | 50.0% | 0% | 100.0% |
| 2500 - 3999 | n | 30 | 90 | 16 | 136 |
| % | 22.06% | 66.18% | 11.76% | 100.0% |
| >4000 | n | 1 | 1 | 3 | 5 |
| % | 20.0% | 20.0% | 60.0% | 100.0% |
| Total | n | 36 | 96 | 19 | 151 |
| % | 23.84% | 63.58% | 12.58% | 100.0% |
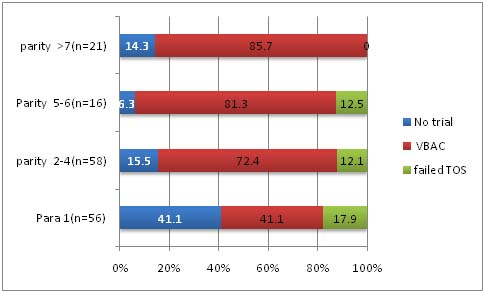
Increasing parity was noted to be associated with an increase in VBAC rate [Table/Fig-9]. This again emphasizes the fact that increases in the number of vaginal deliveries increases the chances of having a successful TOS.
Effect of parity on mode of delivery in women with a prior cesareansection. (n=151)( χ2 = 23.011, p=0.001); VBAC-Vaginal birth after cesarean delivery; TOS-Trial of scar
On analyzing maternal morbidity outcomes [Table/Fig-10]. it was noted that there were two cases of scar dehiscence one of which was in the trial group and the other in a woman who underwent elective cesarean delivery. The former who presented in spontaneous labour had emergency cesarean delivery for suspected scar dehiscence and the diagnosis was confirmed intra-op. The latter was an incidental finding during the surgery while the patient remained asymptomatic. Both women were primiparous with no history of prior vaginal delivery.
Maternal morbidity in women with previous one cesarean delivery
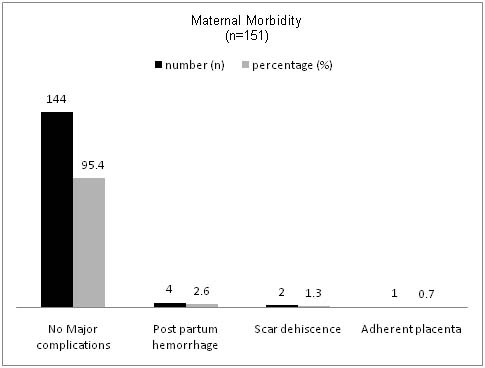
There were four cases of minor postpartum hemorrhage, not requiring blood transfusion in the vaginal delivery group. There were no cases of uterine rupture or third degree perineal tear in the study group.
No significant perinatal morbidity was reported other than the three cases of NICU admissions for transient tachypnea of the newborn (TTN).
Discussion
Good candidates for planned TOS are those women in whom the balance of risks (low as possible) and chances of success (as high as possible) are acceptable to the patient and healthcare provider [2]. In this study also we found that womens’ wishes and the presence of conditions favorable for vaginal delivery influenced the selection of patients for TOS. The women who had high risk for complications like those with prior uterine surgery, short inter-delivery interval and those with unknown scar type were posted for elective lower segment cesarean section (LSCS) as per our Department protocol. Women who were less likely to have serious complications like scar rupture were offered TOS.
The most common indication for the ERCS in our study was unknown scar type in accordance with our Department protocol. This was relevant in the context of extremely mobile patient population belonging to various Asian countries, when, sometimes, it was almost impossible to get documents related to their previous surgery.This is also a major limitation of our study as the number of women taking part in the VBAC Trial was limited by the strict criteria. A case series, from a large tertiary care facility has reported rates of VBAC success and uterine rupture in patients with unknown types of cesarean scar, similar to those from other contemporaneous studies of women with documented previous low transverse uterine incisions [3].They concluded that although obtaining an old record is useful, its absence probably should not interdict a trial of labour in a patient who desires to attempt vaginal delivery.
Additionally, in one study evaluating risk factors for uterine rupture, no significant association was found with the presence of an unknown scar [4].
This study was conducted in Mafraq Hospital, a tertiary care referral Centre in Abu Dhabi, UAE. The annual number of deliveries here is approximately 2,500. The Labour ward is fully equipped with facilities for continuous fetal monitoring, 1:1 nursing care, 24/7 availability of senior obstetricians, neonatologists, anesthetists, and blood banking facilities. Of the 115 women, who attempted TOS, 96 (83.47%) had successful VBAC. This rate is slightly more than that reported in the literature. Most published series of women attempting TOS have demonstrated a probability of VBAC of 60–80% [5–9]. The higher rates in our study could be attributed to the larger number of women with higher parity (2–4) in the study population. There is consistent evidence to show that a prior vaginal delivery and, particularly, a prior VBAC are associated with a higher rate of successful trial of labour (TOL) compared with patients with no prior vaginal delivery [5,10,11]. Our results correlate well with the study by Landon et al., [5] who concluded that previous vaginal delivery including previous VBAC is the greatest predictor for successful TOL. They also reported a reduced success rate for women with induced labour, which is again in agreement with our results. However, their finding that BMI >30 and previous cesarean for dystocia were associated with lower success rates could not be demonstrated in this study. We could not find any significant relation between the indication for previous cesarean and pregnancy outcome.
Elkousy et al., [12] and Flamm et al., [13] have stated that there are reduced chances of successful vaginal delivery with neonatal baby weights more than 4 kg. Our study also highlights the better chances of VBAC for average-sized babies (66.2%) compared to babies weighing more than 4 kg (20%). In addition, we also found that small for gestational age babies had a lower success rate (50%), which is statistically significant.
Most of the large studies in literature on VBAC trial have shown a higher incidence of maternal and perinatal morbidity associated with TOS and failed trial [5, 6, 14]. However, our study did not reveal any significant increased maternal or perinatal morbidity associated with TOS other than a 0.86% incidence of scar dehiscence in the trial group, which is the same as that reported worldwide.
The limitations of our study are:
1. This being a retrospective study, the level of evidence gathered is inferior to that from a randomized control trial.
2. Large number of women of higher parity would probably have a favorable effect on overall outcome.
3. Scarcity of occurrence of adverse events like scar dehiscence could be responsible for their statistical insignificance.
4. Strict hospital protocol regarding selection of women for TOL reduced the number of women in the trial group.
Conclusion
In conclusion, in carefully selected cases, TOS after previous one cesarean is safe and often successful. A prior vaginal delivery, particularly a prior VBAC are associated with a higher rate of success compared to patients with no prior vaginal delivery. Spontaneous onset of labour, average-sized babies and increasing parity are other factors having a positive impact on the successful outcome of TOS. Indication for previous cesarean and BMI were found to have no significant association with the outcome.