The history of hernia is as old as the history of surgery. Inguinal hernias are the commonest of all hernias, surgery is the definitive treatment and hernia repair is the most commonly performed general surgical procedure in clinical practice. Despite high frequency of this procedure, very few have ideal results and post-operative complications.
Frequent occurrence of hernia in inguinal region, enigmatic quality of the aetiologic background and selection of treatment method make it one of the significant parts of surgery. An unacceptable recurrence rate and prolonged post-operative pain (p in small) and recovery time after tissue repair along with our understanding of the metabolic origin of inguinal hernias led to the concept of tension-free hernioplasty-LMR. Numerous comparative randomized trials have clearly demonstrated the superiority of the tension-tree mesh repair over the traditional tissue approximation method. However, tissue repair methods like Bassini’s have the advantage of being simple and cost effective. As surgeons, as a group, have moved away from ‘technical success’ in the form of low recurrence rates, as an outcome measure and assessed other end points, research has moved from the least recurrence to least complication rate. The present study, a comparative study between MBR and LMR, was deemed appropriate as these are performed more commonly in our hospital, catering the rural population with an aim to prospectively evaluate the outcome of LMR (Tension-Free Hernioplasty) vs. MBR (Anatomical Repair) with reference to duration of surgery, post-operative stay and complications and recurrence rate for the two techniques.
Materials and Methods
All the patients admitted in the surgical wards in all the units of Sri Adichunchanagiri Hospital and Research Center, BG Nagara,India. diagnosed to have inguinal hernia were included in the study without bias on a serial basis. Comparative randomized study consisting of 70 patients with 35 patients in Group LMR and 35 patients in Group MBR undertaken to study the Clinical presentation, Risk factors and Complications of Surgical procedures over a period of 18 months from November 2011 to April 2013. Randomization was done by using the SAS software.
Congenital inguinal hernia, pregnant women with inguinal hernia, patients with recurrent / bilateral / complicated inguinal hernia and patients with coagulopathy and those on anti-coagulant therapy were excluded.
Diagnosis was based on clinical findings. Investigations were done to assess the fitness of patients for surgery. Patients were subjected to either MBR or LMR. All patients were given pre-operative prophylaxis with Inj. Cefotaxime 1gm IV. Only spinal anesthesia was administered to both the groups.
For cohorts, classical incision was used i.e., 2.5 cm above and parallel to the medial three fifths of the inguinal ligament (Right / Left depending on side of hernia).
Modified Bassini’s repair-After making in the groin crease external oblique aponeurosis was identified and divided. Sac was separated from cord structures and was dealt appropriately depending on the type of hernia. Conjoint tendon was sutured unto the inguinal ligament with polypropylene ‘1’ interrupted sutures.
Lichtenstein repair-After dissection of the sac polypropylene mesh was placed on the defect and fixed to the inguinal ligament below and to the conjoint tendon above with ‘1-0’ polypropylene.
Post-operatively, Inj. Diclofenac was given as analgesia for 48 hours to both the groups. Post-operatively Inj. Cefotaxime 1gm IV, BD was given for 48 hours to both the groups and patients were evaluated for Pain, Haematoma, Seroma, Infection, Retention of urine. Patients were discharged when considered fit to go about their normal routine. Sutures were removed on 7th day post-operatively. Patients were followed up once a month for the first 3 months, once every 3 months thereafter in first year and once in six months in the next years, observed for recurrence and overall wellbeing.
Results
Statistical Methods
Descriptive statistical analysis has been carried out in the present study. Results on continuous measurements are presented on Mean ± SD (Min-Max) and results on categorical measurements are presented in Number (%). Student t-test (two tailed, independent) and Chi-square/ Fisher Exact test have been used appropriately. Randomization was done using the SAS software. Statistical software namely SAS 9.2, SPSS 15.0, Stata 10.1, MedCalc 9.0.1, Systat 12.0 and R environment ver. 2.11.1 were used for analysis of the data.
Technique of Repair
Total number of 70 patients were present in study with equal distribution to both groups, i.e., 35 (50%) each [Table/Fig-1].
Groups - Number and percentage of patients
| Group | Number of patients | % |
|---|
| Lichtenstein Mesh Repair (LMR) | 35 | 50.0 |
| Modified Bassini’s Repair (MBR) | 35 | 50.0 |
| Total | 70 | 100.0 |
Type of Hernia
In the present study, all the patients were selected irrespective of type of inguinal hernia, of which 20 (28.6%) cases were of Direct type and 50 (71.4%) cases were of Indirect type with distribution between groups being similar [Table/Fig-2].
| Direct/Indirect | Group LMR (n=35) | Group MBR (n=35) | Total (n=70) |
|---|
| Direct | 9 (25.7%) | 11(31.4%) | 20(28.6%) |
| Indirect | 26 (74.3%) | 24(68.6%) | 50(71.4%) |
| Inference | Distribution of Direct/Indirect is statistically similar between two groups with p=0.792 |
Duration of Surgery
Mean duration of surgery in LMR group was significantly less than the MBR group indicating that patients spent less time on the operating table thus reducing the risk of associated complications including anesthetic ones and residents found LMR more easier to perform requiring relatively lesser learning curve compared to MBR [Table/Fig-3].
| Duration of surgery (in min) | Group LMR (n=35) | Group MBR (n=35) | Total (n=70) |
|---|
| Min-Max | 25-56 | 32-61 | 25-61 |
| Mean ± SD | 41.74±7.29 | 47.11±7.51 | 44.43±7.83 |
| Inference | Duration of surgery is significantly less in LMR group with p=0.003** |
Post-Operative Complications: Comparison
Pain
To quantify pain, numerical rating scale was used. The mean pain scores on the day of surgery (evening), post-operative days 1st, 7th & 30th were considered for comparison between the two groups. Pain on POD 7 was significantly (p-value <0.05) more in the LMR group than the MBR group and one patient was lost for follow-up in the MBR group. However, statistical significance of pain on POD 30 was only suggestive of pain more in LMR group (p-value 0.096) and 2 patients each in both groups were lost for follow up [Table/Fig-4].
| Post-operative pain | Group LMR (n=35) (Mean±SD) | Group MBR (n=35) (Mean±SD) | Total (n=70) | p-value (LMR vs MBR) |
|---|
| POD 0 | 5.29±1.13 | 5.06±1.05 | 5.17±1.09 | 0.384 |
| POD 1 | 3.31±1.35 | 3.26±1.07 | 3.29±1.21 | 0.844 |
| POD 7 | 2.09±1.09 | 1.24±0.96 | 1.67±1.11 | 0.001** |
| POD 30 | 0.45±0.66 | 0.21±0.49 | 0.33±0.58 | 0.096+ |
Haematoma
In our study, 2.9% and 5.7% of patients undergoing LMR and MBR respectively and 4.3% of the 70 patients who underwent either surgeries developed haematoma [Table/Fig-5].
Haematoma incidence according to technique of repair
| Technique of repair | Number of patients in group | Number of patients with Haematoma | % |
|---|
| Lichtenstein’s | 35 | 1 | 2.9 |
| Modified Bassini’s | 35 | 2 | 5.7 |
| Total | 70 | 3 | 4.3 |
| Inference | Incidence of haematoma was 5.7% in MBR group compared to 2.9% in LMR with p=1.000 |
Seroma
In the present study, 22.9% of patients in LMR group and 8.6% in MBR group developed seroma. The p-value was found to be insignificant [Table/Fig-6].
Seroma incidence according to technique of repair
| Technique of repair | Number of patients in group | Number of patients with Seroma | % |
|---|
| Lichtenstein’s | 35 | 8 | 22.9 |
| Modified Bassini’s | 35 | 3 | 8.6 |
| Total | 70 | 11 | 15.7 |
| Inference | Incidence of seroma was 8.6% in MBR group compared to 22.9% in LMR with p=0.188 |
Infection
In the present study, only 2 patients, i.e., 5.7%, who had undergone Lichtenstein’s mesh hernioplasty developed post-operative wound infection. There were none in the MBR group. P-value was insignificant [Table/Fig-7].
Infection incidence according to technique of repair
| Technique of repair | Number of patients in group | Number of patients with Infection | % |
|---|
| Lichtenstein’s | 35 | 2 | 5.7 |
| Modified Bassini’s | 35 | 0 | 0.0 |
| Total | 70 | 2 | 2.9 |
| Inference | Incidence of infection was 0% in MBR group compared to 5.7% in LMR with p=0.493 |
Recurrence
Only two recurrences occurred during the study period and both were in MBR group (5.7%). However, no statistically significant difference was present between the two groups [Table/Fig-8].
Incidence of recurrence according to technique of repair
| Technique of repair | Number of patients in group | Number of patients with recurrence | % |
|---|
| Lichtenstein’s | 35 | 0 | 0.0 |
| Modified Bassini’s | 35 | 2 | 5.7 |
| Total | 70 | 2 | 2.9 |
| Inference | Incidence of recurrence was 5.7% in MBR group compared to 0% in LMR with P=0.493 |
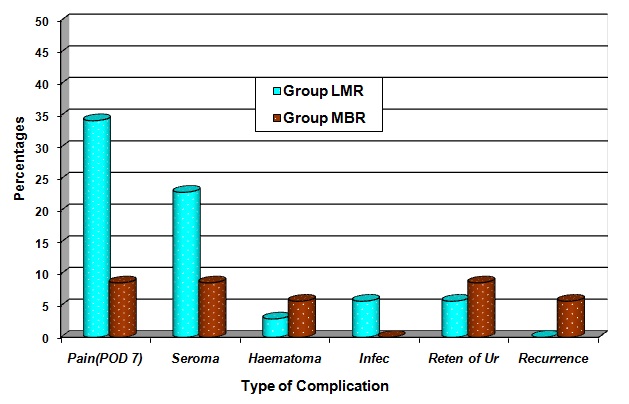
Other Post-operative complications
Retention of urine was seen in 2 (5.7%) and 3 (8.6%) of the patients in LMR and MBR group respectively. No statistical difference between the two groups. There was no incidence of ischemic orchitis, scrotal ecchymosis, osteitis pubis or any other complications other than mentioned above. This may be due to the less number of cases in the study groups [Table/Fig-9, 10].
Incidence according to technique of repair
| Other Post-operative Complications | Group LMR (n=35) | Group MBR (n=35) | Total (n=70) |
|---|
| Retention of Urine | 2 (5.7%) | 3 (8.6%) | 5 (7.1%) |
| Ischemic Orchitis | 0 | 0 | 0 |
| Scrotal Ecchymosis | 0 | 0 | 0 |
| Osteitis Pubis | 0 | 0 | 0 |
Comparison of post-operative complications between repairs
5. Duration of Post-Operative Hospital Stay
Patients who had undergone MBR had on an average stayed for 3.97 days in the hospital as compared to 3.46 days following LMR. Post-operative hospital stay was a tad less in LMR than MBR and the difference between two groups was found statistically similar. Following MBR, 3 cases stayed beyond 7 days accounting for 8.6% of cases, while following LMR, 7 (20%) cases stayed for more than 7 days [Table/Fig-11].
Post-operative hospital stay
| Post-operative stay | Group LMR (n=35) | Group MBR (n=35) | Total (n=70) |
|---|
| 1-2 days | 4(11.4%) | 7(20.0%) | 11(15.7%) |
| 3-4 days | 17(48.6%) | 19(54.3%) | 36(51.4%) |
| 5-7 days | 7(20.0%) | 6(17.1%) | 13(18.6%) |
| >7 days | 7(20.0%) | 3(8.6%) | 10(14.3%) |
| Mean ± SD | 3.46±1.96 | 3.97±1.92 | 3.71±1.94 |
| Inference | Post-operative hospital stay is less in LMR with p=0.271 |
Discussion
The description of the Lichtenstein tension free mesh repair opened a new era in groin hernia repair. The method is very simple, effective and with minimal complications. So, it is currently the preferred method for inguinal hernia repair worldwide. However, Bassini’s repair though done infrequently, has advantages in situations like contaminated field and in low resource settings. Moreover in terms of post-operative complications and overall success of procedure both MBR and LMR are rated equal in many studies.
Type of Hernia-Indirect hernia constituted 76%, in a study by Palanivelu (C. Palanivelu et al.,) [1], 63% in the study of Robb (Robb H Rutledge) [2] and 71.4% in our study. Direct hernia constituted 24% in the Palanivelu study, 37% in Robb’s study and 28.6% in our study. The results of the present study are comparable with the previous studies.
Duration of Surgery-Both the types of repairs were performed by senior residents, with neither having a significant advantage over the other, the length of operation being kept to a minimum. It is important in two respects: the patients, who are on the whole middle aged to elderly, spend less time on the operating table thus reducing the risk of associated complications.
The difference in length of operation as recorded in our study was statistically significant with LMR taking lesser time to perform than MBR (p <0.05), while though the difference was insignificant in the MM Harjai study [3] (p >0.05), LMR took lesser time compared to MBR. Surgeons in training found LMR easier to learn and perform than the MBR.
Post-Operative Pain-The pain scale used in this study was numerical rating scale which is an appropriate tool to use in the clinical assessment of pain. On a scale of ‘0-10’, ‘0’ marked no pain, ‘1-3’ was considered as mild pain, ‘4-7’ as moderate pain and ‘8-10’ as severe pain. Pain was found to be significantly more in LMR group only on POD 7. There was only 1case (LMR group) of severe pain (NRS score – 8) suggesting nerve injury in our study.
During the repair of inguinal hernia using mesh, there is considerably less tissue tension employed to close the abdominal wall defect than in techniques in which sutures are used such as the Bassini’s method. Therefore, it would be expected that there would be less pain involved in mesh repairs because of this reduced tension. There are clinical trials which contradict these claims.
In a previous study by Callesen et al., [4], showed that there was no significant difference in pain following LMR or MBR (36% and 28%). In a similar study done by H Lau and F Lee [5], it was found that age was the only independent predictive factor of pain score. The present study did not take into consideration long term chronic and persisting type of pain during follow-up to assess pain intrinsic to the technique.
Post-operative Complications-There are a number of complications known to arise with some regularity. In present study, most common complication was seroma formation.
Seroma-In the present study, 22.9% of patients who had undergone LMR and 8.6% of patients who had undergone MBR developed seroma. In a study by Faish T et al., [6] 2% of patients who had undergone mesh plug hernioplasty developed seroma. This discrepancy between the two studies may be attributed to the criteria used to define seroma. In our study, all the cases with ooze from the incision site were included. In the other study only those cases which required drainage were included. In MM Harjai study [3], it was 4.08% for LMR and 6.78% for MBR.
Haematoma-In our study, 2.9% and 5.7% of patients undergoing LMR and MBR developed haematoma respectively (statistically insignificant). In study by MM Harjai et al., [3], 1.02% of LMR developed haematoma compared to 4.24% of MBR.
Infection-In the present study, only 5.7% of cases who had undergone LMR developed post-operative wound infection with no incidence in MBR. This is probably due to presence of a foreign body (mesh) which increases the occurrence and subsequent proliferation of pathogens, in case of LMR. In MM Harjai study [3], it was 9.18% in LMR group and 9.32% in MBR group.
Retention of urine-Retention of urine in case of an inguinal hernia repair is usually transient and is mostly due to post-operative neuralgia commonly seen in elderly. In our study, 5.7% of the LMR group and 8.6% of the MBR group developed retention of urine and required catheterization. In MM Harjai study [3], 14.29% of Lichtenstein’s repair group and 19.49% of the modified Bassini’s group had retention of urine.
Testicular Complications-Two complications concerning testis are ischemic orchitis and testicular atrophy, which manifests 24 to 72 hours post-operatively and may last up to 6 weeks. In a survey of 52,582 cases operated for primary inguinal hernias at Shouldice clinic, 19 cases of testicular atrophy were recorded. In our study no such complications were recorded.
Recurrence-The recurrence rate has always been considered an important parameter to assess the effectiveness of any form of hernia repair and is the ultimate test. There are studies plenty, which have determined the recurrence rate for different techniques. Bendavid R [7], after a survey. of literature quoted recurrence and re-recurrence rate in different techniques.
The above table amply demonstrates the superiority of mesh repairs over conventional tissue repairs, in both primary and recurrent inguinal hernias.
In the present study, there was 0% recurrence in LMR group and 5.7% in MBR group but with insignificant p-value (0.493). A 4 year study by Csontos et al., [8] of 714 cases had 16 recurrence (2.04%) following LMR. Many studies have shown conventional tissue repair comparable with that of mesh hernioplasty. This may be due to the bias introduced by the skill of the surgeon. This is not so in mesh hernioplasty which gives consistent good result whether the surgeon is a beginner or an experienced. A study by Amid PK [9] has shown that mesh repair is superior to pure tissue approximation repairs. A study by Nathan JD and Pappas TN [10] concluded that LMR is the most frequently performed inguinal hernia operation with recurrence rate of less than 1%. Mesh repair allows optimal results both for the surgery point (easiness of the technique, repeatability, less invasivity, scanty incidence of recurrence, low frequency of post-operative complications) and in economic terms, allowing an early mobilization.
In the present study, although p-value is insignificant due to the small sample size, and the study period was too small, non-statistically LMR has shown superior results (0% recurrence) to that of MBR (5.7% recurrence). The combined recurrence rate may fall well below 0.1% with specialization and with proper selection of patients and technique tailor made for individual patients.
Hospital stay-In the fast paced life of today, duration of hospital stay may be the determining factor when the rates of other complications are comparable including recurrence. In our present study the mean hospital study in case of MBR was 3.97 days and incase of LMR it was 3.46 days. In MM Harjai study [3], the average hospital stay in the post-operative period for MBR was 5.74 days (range 2-16 days), and 4.97 days (range 2-11 days) for patients undergoing LMR.
Conclusion
The problem in the repair of inguinal hernia is the wide discrepancy between the monotonous excellence achieved in personal series and the uniformly depressing results were obtained by impersonal statistical reviews. But, the question as to which is the best of all available techniques suitable for all kinds of inguinal hernia still remains unanswered. The concept of judging the supremacy of a hernia repair technique over others using recurrence rate as a criterion is questionable.
To conclude, in the light of above results, though the present comparative study does not show any distinct advantages of one repair over the other, LMR gives superior results compared to MBR with regard to technical simplicity, smaller dissection and early ambulation with an acceptable post-operative rehabilitation and relative regards to recurrence. However, because of small sample size and short follow-up period in the current study, a larger study sample and a longer follow up study may be needed before any further conclusions can be made. Surgeons in training found LMR technique easier to master than MBR. But, however, MBR offers advantage of being cost effective and is still being useful for conditions such as strangulated inguinal hernia and in settings which doesn’t allow the use of mesh for repair like in an infected scenario. So individualization of cases with tailor made approach is necessary to circumvent the operative complications in inguinal hernia repair.