Background: Diabetic patients with concomitant dyslipidemia are often soft targets for cardiovascular disease and deaths. An early intervention to normalize circulating lipids has been shown to reduce cardiovascular morbidity and mortality. Glycosylated hemoglobin (HbA1c) is routinely used as a marker to indicate long-term glycemic control.
Aim: Our aim was to test whether HbA1c can serve as a marker of circulating lipids among Type 2 diabetic patients.
Methods: The sera of 130 Type 2 diabetic patients was analyzed for fasting blood sugar (FBS), HbA1c and lipid profile consisting of total cholesterol (TC), triglycerides (TG), High-density Lipoprotein (HDL) cholesterol and LDL cholesterol. We divided the subjects based on their glycemic index into three groups; HbA1c< 6% as good, HbA1c>6% - <9% as poor and HbA1c>9% as worst glycemic control. One–way analysis of variance (ANOVA) and post-hoc Dunnett’s multiple comparison tests was used to examine the significance levels for various biochemical parameters in age-categorized groups.
Results: The mean ± SD levels of HbA1c was significantly higher in females (8.598 ± 2.284 %) compared to males (7.323±2.18 %). Older patients had HbA1c, FBS and lipid profile levels similar to younger ones. HbA1c showed direct and significant correlations with cholesterol, TG and LDL. Univariate analysis showed that HbA1c was a good predictor of circulating lipid levels.
Conclusion: The study indicates the usefulness of HbA1c as a marker for lipid profile for screening of diabetic patients at high risk of developing cardiovascular diseases.
Coronary artery disease, Dyslipidemia, Glycemic control
Introduction
Population surveys conducted over two decades in India reported a 9-fold increase of coronary artery disease (CAD) in urban centres. This increase is mainly associated with increase in the prevalence of lipid and glucose abnormalities [1]. Indians are known to have relatively lower levels of lipids and lipoproteins, raised TG and low HDL Cholesterol and presence of metabolic syndrome explaining more than half of the excess burden of CAD [2]. Diabetes mellitus is emerging as a global endemic both in developing and developed countries. It is characterized by metabolic abnormalities and long-term micro and macro vascular complications. There is a high risk of CAD in people with type 2 diabetes. Individuals with coexisting diabetes and metabolic syndrome have a high prevalence of CAD [3].
HbA1c is commonly used as a marker of long term glycemic status. Elevated HbA1c has also been regarded as an independent risk factor for CAD in subjects with or without diabetes. Thus elevated HbA1c has been proposed as an independent risk factor for both diabetics and CAD patients [4]. Significantly increased levels of cholesterol and lipids are seen in type 2 diabetic patients with CAD as compared to diabetic patients without CAD [5]. It has been observed that there is a direct correlation between HbA1c and the severity of CAD in diabetic patients [6]. The American Diabetes Association (ADA) estimated that the risk of diabetes related mortality increased 25% for each 1% increase in HbA1c. It has also been estimated that each percentage point increase in HbA1c corresponds to a 35% increase in the risk of macrovascular complication and an 18% increase in risk of myocardial infarction [7].
A strong correlation has been shown between lipid profile and CAD. The Framingham study has demonstrated a linear increase in CAD risk with increment of TC level from 180 mg upward. The study established that individuals with HDL cholesterol less than 35 mg/dl have 8 times increase in CAD incidence than those with HDL cholesterol more than 65 mg/dl [8]. The Lipid Research clinics Coronary Primary Prevention Trial concluded that a 1% fall in the TC reduced the CAD risk by 2% [9]. Helsinki heart study concluded that a mean 12% rise in HDL cholesterol and an 11% fall in LDL cholesterol were both correlated with a 34% decline in CAD [10].
Very few studies have shown a positive correlation between glycemic control and lipid profile. Dyslipidemia, frequently occurring in type 2 diabetes patients, might play a critical role in accelerated macrovascular atherosclerotic disease formation and may contribute significantly to the excess risk of CAD in type 2 diabetes patients [11]. Early therapeutic interventions, aiming to stabilize blood glucose levels along with reduction in TG and LDL and to increase HDL, significantly reduce cardiovascular events and mortality in patients with type 2 diabetes [12].
So control of blood glucose level may improve the lipid profile and thus reduce the risk of CAD in type 2 diabetic patients. We aimed to compare lipid profiles between uncontrolled (HbA1c>9%), moderately controlled (6%<HbA1c<9%) and controlled (HbA1c<6%) diabetic subjects to explore the association of glycemic status with CAD risk factor.
Materials and Methods
This is a retrospective study comprising of a total of 130 type 2 diabetic patients who visited the M S Ramaiah Medical College and Teaching Hospitals, Bangalore, Karnataka, India. Ethical Clearance was obtained from the Institutional ethical committee for human research to conduct the study. The sample consisted of 94 males and 36 females. The age mean ± standard deviation of male and female subjects was 53.52 ± 11.68 years (Range 22 - 85 years) and 51.53 ±10.85 years (Range 22-77 years), respectively. All the patients were categorized into three age groups: <40 years (18 patients), 41– 60 years (85 patients), > 60 (27 patients).
Venous blood samples from all the subjects were collected in serum separator tubes after overnight fasting. The venepuncture was done in the cubital vein. Torniquet was used but was released just before sampling to avoid artificial increase in the concentration of serum lipids. Serum was separated within 2 hours of collection to prevent artificial changes in concentration of HDL. The blood was centrifuged at 5,000 rpm for 10 minutes. The supernatant clean serum was then pipetted out using dry piston pipettes with disposable tips and stored in dry thin walled vials at -200C until further analysis. Care was taken to exclude the hemolysed samples. The sera were analyzed for HbA1c, FBS, TC, TG and HDL using an auto analyzer (Roche Modular P-800, Germany). The level of LDL cholesterol was determined using the Friedewald formula: LDL = (cholesterol—TG)/ (2.2 HDL) [13].
The impact of glycemic control on various parameters was evaluated by categorizing all the patients into three categories on the basis of HbA1c levels; < 6% good glycemic control, 6–9% poor glycemic control and 9% worse glycemic control. The selection of these cutoff values of HbA1c was based on earlier studies [14].
Statistical Analysis
The data were analyzed by SPSS version 10. Pearson’s correlation test was performed to examine various correlations. Independent samples Student’s t-test was used to compare the means of different parameters between males and females. One-way analysis of variance (ANOVA) and post-hoc Dunnett’s multiple comparison tests was used to examine the significance levels for various biochemical parameters in age-categorized groups. Univariate analysis was performed to evaluate the effects of gender, age and glycemic control on serum lipid profile. p-value of ≤0.05 was considered as statistically significant.
Results
Our study results showed that female diabetic patients had poorer glycemic control with significant higher HbA1c (p=0.004) level when compared to males. The FBS levels were slightly higher in females as compared to male, but it was not statistically significant. Also the TC and HDL were significantly higher in females. The levels of TGs were lower and LDL was higher in females than males [Table/Fig-1]. There was a significant increase in HbA1c in the 41-60 years age group. Also an inverse relationship was noticed between age and glycemic control among females [Table/Fig-2]. Older patients had lower FBS, cholesterol, TGs and LDL levels though not statistically significant in comparison with the other two groups [Table/Fig-2].
Serum biochemistry categorized by patient’s gender
| Parameter | Gender of patients |
|---|
| Male (n=94 ) | Female (n=36 ) |
|---|
| HbA1c (%) | 7.323±2.1793 | 8.598±2.2844* |
| FBS (mg/dL) | 142.515±52.8370 | 159.511±67.5262 |
| Cholesterol(mg/dL) | 166.102±32.8445 | 181.425±39.5944* |
| TGs (mg/dL) | 152.888±100.6199 | 136.578±65.8616 |
| HDL (mg/dL) | 40.490±7.9651 | 46.147±8.0834*** |
| LDL (mg/dL) | 96.867±27.3643 | 104.286±25.0143 |
*p <0.05, ***p<0.001
Serum biochemistry categorized by patient’s age
| Parameter | Age of patient |
|---|
| < 40 years (n=18 ) | 41-60 years (n=85 ) | >61years (n=27 ) |
|---|
| HbA1c (%) | 6.969±2.1464 | 8.071±2.3129* | 6.881±1.9444 |
| FBS (mg/dL) | 147.428±72.9540 | 151.329±58.1229 | 134.152±42.2646 |
| Cholesterol (mg/dL) | 169.044±34.195 | 173.687±35.9477 | 160.693±33.6184 |
| TGs (mg/dL) | 139.200±88.4943 | 159.782±100.4195 | 118.563±56.6857 |
| HDL (mg/dL) | 40.009±8.0814 | 43.563±10.1492 | 42.05±8.3620 |
| LDL (mg/dL) | 101.339±21.6729 | 101.173±28.7033 | 90.2222±22.5328 |
*p <0.05, ***p<0.001
Diabetic patients with poor and worse glycemic control had significantly higher levels of FBS (F = 28.387, p <0.001), TGs (F = 11.705, p < 0.001), TC (F = 11.881, p< 0.001), LDL (F = 6.301, p < 0.001) and lower levels of HDL (F = 1.555, p= 0.215) as compared to patients with good glycemic control (HbA1c≤ 6%). Serum HDL decreases with poor glycemic control among males unlike females. However, no significant difference between HbA1c (F = 1.55, p = 0.215) as well as HDL among the patients of different age groups [Table/Fig-3,4 and 5a-f].
Serum biochemistry categorized by patient’s glycemic control (HbA1c) *p <0.05, ***p<0.001
| Parameter | Percentage (n=17) |
|---|
| < 6 % (n=36 ) | >6 to < 9% (n=59 ) | > 9 % (n=35 ) |
|---|
| Good Control | Poor Control | Worse Control |
|---|
| FBS(mg/dL) | 115.258±46.4726 | 136.858±26.3565 | 197.569±72.5643*** |
| Cholesterol (mg/dL) | 163.656±25.4143 | 160.808±33.1163 | 193.303±38.2209*** |
| TGs(mg/dL) | 113.978±64.6142 | 134.915±62.1494 | 206.431±128.2124*** |
| HDL(mg/dL) | 43.869±8.6782 | 40.790±6.8359 | 42.329±10.08549 |
| LDL(mg/dL) | 94.581±25.2015 | 93.725±23.9519 | 112.146±29.2434** |
Univariate analysis of variance model to evaluate the effects of gender, age, HbA1c and their interaction on serum lipid profile ANOVA F and p-values have been shown with the level of significance has been kept at p≤0.05
| Parameter | Cholesterol | TG | HDL | LDL |
|---|
| df | F | p | F | p | F | p | F | p |
|---|
| Gender | 1 | 5.04 | 0.026 | 0.811 | 0.370 | 13.02 | 0.00 | 2.00 | 0.159 |
| Age | 2 | 1.04 | 0.249 | 2.18 | 0.12 | 0.972 | 0.381 | 1.812 | 0.17 |
| HbA1c | 2 | 11.88 | 0.000 | 11.70 | 0.000 | 1.555 | 0.21 | 6.301 | 0.002 |
Comparison of HbA1c levels in males and female diabetic patients with respect to various parameters like age, FBS, TC, TGL, LDL and HDL depicted in Fig a-f respectively
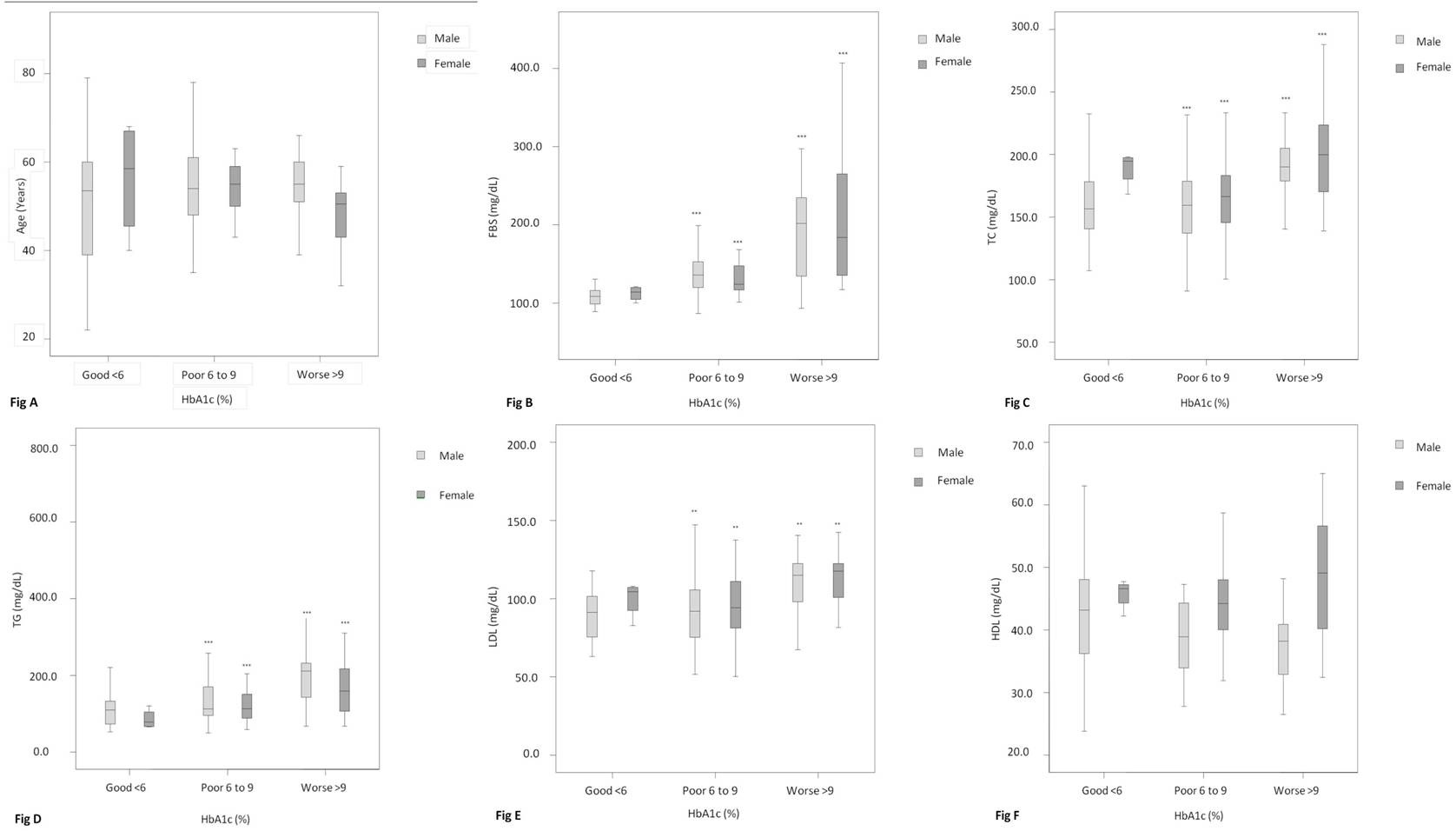
The results of univariate analysis addressed the impact of patient gender, age and HbA1c in influencing serum lipids [Table/Fig-4]. Patients’ gender was significantly associated with lipid parameters in decreasing magnitude in the following manner: HDL (F = 13.02), cholesterol (F = 5.04) and TGs (F = 0.811). HbA1c appeared to be a good predictor of cholesterol (F = 11.88), followed by TGs (F = 11.70), LDL (F = 6.301) and HDL (F = 1.56).
Discussion
Approximately 50-75% of deaths in patients with diabetes are attributable to cardiovascular diseases [15]. Elevated HbA1c has been regarded as an independent risk factor for CAD in subjects with or without diabetes [16]. The Diabetes Complications and Control Trial (DCCT) established HbA1c levels <7% appropriate for reducing the risk of vascular complications and also as the gold standard of glycemic control [15]. Each 1% reduction in HbA1c was associated with reduction in risk of 21% for any end point related to diabetes, 21% for deaths related to diabetes, 14% for myocardial infarction, and 37% for micro vascular complications. Thus reduction in HbA1c is associated with reduction in diabetes related risk complication [15]. Type 2 diabetic patients are at a much higher risk of cardiovascular diseases than the non-diabetic. Thus the risk of cardiovascular events in diabetics can be reduced by improving the glycemic control [17].
Significant dyslipidemia has been encountered among type 2 diabetic subjects. Very few investigators have reported significant correlations between HbA1c and lipid profiles [18] and suggested the importance of glycemic control in normalizing dyslipidemia [19,20]. Also many studies have shown the beneficial effects of reducing lipids on cardiovascular system [21,22].
In our study we found that HbA1c has direct and significant correlations with FBS, TC, TG and LDL similar to many other reports [19,20]. Diabetic patients with poor and worse glycemic control had significantly higher levels of FBS, TG , TC, LDL, TG similar to other studies [19,21,22]. However these patients had a lower level of HDL cholesterol when compared to patients with good glycemic control. It has been reported that HDL cholesterol is inversely, and non-HDL cholesterol directly, associated with CAD risk in diabetes patients [23]. The cause of dyslipidaemia in type 2 diabetes mellitus may be due to impaired liver apolipoprotein production which in turn regulates the enzymatic activity of lipoprotein lipase and cholesterol ester transport protein [24]. Old subjects showed low levels of FBS, TC, TG and LDL [25] levels where as young type 2 diabetic patients with poor glycemic control showed significantly higher TC, TG and LDL similar to other studies [26].
The levels of HbA1c were significantly higher in female patients when compared to males [Table/Fig-1]. Diabetes confers markedly increased risk of cardiovascular complications among both males and females [27]. However, women with diabetes are more susceptible to increased cardiovascular mortality [28]. They are subject to more adverse changes in coagulation, vascular function and cardiovascular risk factors than diabetic men. Serum HDL decreased with poor glycemic control among males unlike females. The results of lipid profile showed that female diabetic patients had significantly higher levels of HDL cholesterol, which is in agreement with earlier reports [22,29]. This may be attributed to the effects of sex hormones on body fat distribution, leading to differences in altered lipoproteins [30].
Glucose lowering is essential for the prevention of micro vascular complication, and improvement in cholesterol is central to reducing cardiovascular disease in these patients [21]. A significant correlation between dyslipidemia (increased LDL) has been observed in type 2 diabetics, suggesting their increased susceptibility to vascular disease [31]. It is likely that the combination of hyperglycemia, dyslipidemia, insulin resistance and hypertension as in metabolic syndrome produces an enhanced atherogenic environment within the circulation [32]. Changes occurring in diabetic dyslipidaemia include quantitative and qualitative changes. Quantitative changes include increase in LDL levels and decrease in HDL levels, due to increase in hepatic lipase activity and decrease in VLDL clearance. Qualitative changes include size difference in lipid parameters , non enzymatic glycosylation of LDL and susceptibility of LDL cholesterol to form peroxides, thus increasing risk of atherosclerosis and cardiovascular complications among diabetic patients [33].
Hyperglycaemia increases complications in diabetes mellitus by generating reactive oxygen species, resulting on oxidative stress. Increased lipid peroxidation causes crosslink formation between single molecules of amino acids and LDL particles. In metabolically poorly controlled diabetic patients, glycation of LDL increases with hyperglycemia [34]. This elevated level of LDL is explained by decreased catabolism of LDL, decreased activity of cholesterol ester transfer protein and lipoprotein lipase activity [21,34]. It has been suggested that non enzymatic glycosylation of the LDL particle itself result in its increased incorporation in the arterial wall [35]. Further glycosylation of lysine groups on apolipoprotein B causes inhibition of the ability of LDL to interact with the LDL receptor. This in turn inhibits the ability of LDL to be metabolized by the LDL receptor pathway. Thus plasma LDL levels are high and atherosclerosis occurs very early in life [35]. Because of its critical importance in atherogenesis, LDL cholesterol is a focus of current guidelines for determination of the risk of cardiovascular diseases. The above discussion clearly indicates the clinical significance of various lipid parameters in predisposing diabetic patients to cardiovascular complications. Significant correlations between HbA1c and all lipid parameters and a linear relationship between HbA1c and dyslipidemia point towards the usefulness of HbA1c for screening diabetic patients at high risk of developing CAD.
Limitations
Even though our sample comprised only patients with type 2 diabetes, a population with well known high risk for CAD, other important variables were not considered in the model. Further this is a retrospective study with a small number of patients. Thus a prospective study with a large number of patients is further warranted to clearly suggest that HbA1c can be used as marker of circulating lipids. We have also not mentioned the VLDL results in this study as we did not get the required sample of VLDL tests during the study to statistically analyze them [36] as there have been studies which have proven that VLDL is the fundamental cause of atherogenesis in diabetes. We have not tested the effect of glycemic control on various lipid ratios as study of these ratios have proven to be useful as markers for insulin resistance and CVD risk in T2D patients [37].
Conclusion
The findings of the study ensures HbA1c predicts serum lipid profile. It provides valuable supplementary information about the extent of circulating lipids besides its primary role in monitoring long-term glycemic control. Thus, dual biomarker capacity of HbA1c (glycemic control as well as lipid profile indicator) may be utilized for screening high-risk diabetic patients for timely intervention with lipid lowering drugs and thus preventing adverse cardiovascular events.
*p <0.05, ***p<0.001
*p <0.05, ***p<0.001
[1]. Bulatao RA, Stephens PW, Global estimates and projections of mortality by cause 1992 Washington DCPopulation, Health and nutrition Department; World Bank; pre-working paper 1007 [Google Scholar]
[2]. Enas EA, Jacob S, Coronary artery disease in Indians in the USA. In: Sethi K, edCoronary artery disease in Indians - A Global Perspective 1998 MumbaiCardiological Society of India:32-43. [Google Scholar]
[3]. Ader DJ, Effect of insulin resistance, dyslipidemia, and intra-abdominal adiposity on the development of cardiovascular disease and diabetes mellitusAm J Med 2007 120(3 Suppl 1):S12-8. [Google Scholar]
[4]. Khan HA, Clinical significance of HbA1c as a marker of circulating lipids in male and female type 2 diabetic patientsActa Diabetol 2007 44:193-200. [Google Scholar]
[5]. Giansanti R, Rabini RA, Romagnoli F, Fumelli D, Sorichetti P, Boemi M, Coronary heart disease, type 2 diabetes mellitus and cardiovascular disease risk factors: a study on a middle-aged and elderly populationArch Genontol Geriatr 1999 29(2):175-82. [Google Scholar]
[6]. Ravipati G, Aronow WS, Ahn C, Sujata K, Saulle LN, Weiss MB, Association of hemoglobin A(1c) level with the severity of ischemic heart disease in patients with diabetes mellitusAm J Cardiol 2006 97(7):968-9. [Google Scholar]
[7]. America Diabetes AssociationStandards of medical care in diabetesDiabetes care 2004 27(Suppl 1):S15-S35. [Google Scholar]
[8]. Wilson PWF, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB, Prediction of coronary heart disease using risk factor categoriesCirculation 1998 97(18):1837-47. [Google Scholar]
[9]. The Lipid Research Clinics Coronary Primary Prevention Trial results. I. Reduction in incidence of coronary heart diseaseJAMA 1984 251(3):351-64. [Google Scholar]
[10]. Frick MH, Elo O, Haapa K, Heinonen OP, Heinsalmi P, Helo P, Helsinki heart study: primary-prevention trial with gemfibrozil in middle-aged men with dyslipidemia. Safety of treatment, changes in risk factors, and incidence of coronary heart diseaseN Engl J Med 1987 317(20):1237-45. [Google Scholar]
[11]. Garg A, Grundy SM, Management of dyslipidemia in NIDDMDiabetes Care 1990 13(2):153-69. [Google Scholar]
[12]. Jones PH, Clinical significance of recent lipid trials on reducing risk in patients with type 2 diabetes mellitusAm J Cardiol 2007 99(4A):133B-140B. [Google Scholar]
[13]. Warnick GR, Knopp RH, Fitzpatrick V, Branson L, Estimating low-density lipoprotein cholesterol by the Friedewald equation is adequate for classifying patients on the basis of nationally recommended cutpointsClin Chem 1990 36(1):15-9. [Google Scholar]
[14]. Rosediani M, Azidah AK, Mafauzy M, Correlation between fasting plasma glucose, post prandial glucose and glycated haemoglobin and fructosamineMed J Malaysia 2006 61(1):67-71. [Google Scholar]
[15]. DCCT Research GroupThe absence of a glycemic threshold for the development of long-term complications: the perspective of the diabetes control and complications trialDiabetes 1996 45(10):1289-98. [Google Scholar]
[16]. Selvin E, Coresh J, Golden SH, Brancati FL, Folsom AR, Steffes MW, Glycemic control and coronary heart disease risk in persons with and without diabetes: the atherosclerosis risk in communities studyArch Intern Med 2005 165(16):1910-16. [Google Scholar]
[17]. Avogaro A, Giorda C, Maggini M, Mannucci E, Raschetti R, Lombardo F, Incidence of coronary heart disease in type 2 diabetic men and women: impact of microvascular complications, treatment and geographic locationDiabetes Care 2007 30(5):1241-7. [Google Scholar]
[18]. Smellie WS, Hypertriglyceridaemia in diabetesBMJ 2006 333(7581):1257-60. [Google Scholar]
[19]. Ladeia AM, Adan L, Couto-Silva AC, Hiltner A, Guimaraes AC, Lipid profile correlates with glycemic control in young patients with type 1 diabetes mellitusPrev Cardiol 2006 9(2):82-8. [Google Scholar]
[20]. Chan WB, Tong PC, Chow CC, So WY, Ng MC, Ma RC, Triglyceride predicts cardiovascular mortality and its relationship with glycemia and obesity in Chinese type 2 diabetic patientsDiabetes Metab Res Rev 2005 21(2):183-8. [Google Scholar]
[21]. Huang ES, Meigs JB, Singer DE, The effect of interventions to prevent cardiovascular diseases in patients with type-2 diabetes mellitusAm J Med 2001 111(8):633-42. [Google Scholar]
[22]. Hanefeld M, Fischer S, Julius U, Schulze J, Schwanebeck U, Schmechel H, Risk Factors for myocardial infarction and death in newly detected NIDDM: the Diabetes intervention study, 11-year follow-upDiabetologia 1996 39(12):1577-83. [Google Scholar]
[23]. Eshaghian S, Horwich TB, Fonarow GC, An unexpected inverse relationship between HbA1c levels and mortality in patients with diabetes and advanced systolic heart failureAm Heart J 2006 151(1):91 [Google Scholar]
[24]. Goldberg IJ, Lipoprotein lipase and lipolysis: central roles in lipoprotein metabolism and atherogenesisJ Lipid Res 1996 37(4):693-707. [Google Scholar]
[25]. Kalofoutis C, Piperi C, Zisaki A, Singh J, Harris F, Phoenix D, Differences in expression of cardiovascular risk factors among type 2 diabetes mellitus patients of different ageAnn N Y Acad Sci 2006 1084:166-77. [Google Scholar]
[26]. Petitti DB, Imperatore G, Palla SL, Daniels SR, Dolan LM, Kershnar AK, Serum lipids and glucose control: the SEARCH for Diabetes in Youth studyArch Pediatr Adolesc Med 2007 161(2):159-65. [Google Scholar]
[27]. Haffner SM, Lehto S, Ronnemaa T, Pyorala K, Laakso M, Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarctionN Engl J Med 1998 339(4):229-34. [Google Scholar]
[28]. Gu K, Cowie CC, Harris MI, Diabetes and decline in heart disease mortality in US adultsJAMA 1999 281(14):1291-7. [Google Scholar]
[29]. Esteghamati A, Abbasi M, Nakhjavani M, Yousefizadeh A, Basa AP, Afshar H, Prevalence of diabetes and other cardiovascular risk factors in an Iranian population with acute coronary syndromeCardiovasc Diabetol 2006 5:15 [Google Scholar]
[30]. Sibley SD, Thomas W, de Boer I, Brunzell JD, Steffes MW, Gender and elevated albumin excretion in the Diabetes Control and Complications trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) cohort: role of central obesityAm J Kidney Dis 2006 47(2):223-32. [Google Scholar]
[31]. Nasri H, Yazdani M, The relationship between serum LDL-cholesterol, HDL-cholesterol and systolic blood pressure in patients with type 2 diabetesKardiol Pol 2006 64(12):1364-8.discussion. 1369-71 [Google Scholar]
[32]. Nasri H, Yazdani M, The relationship between serum LDL-cholesterol, HDL-cholesterol and systolic blood pressure in patients with type 2 diabetesKardiol Pol 2006 64(12):1364-8.discussion 1369-71 [Google Scholar]
[33]. Arora M, Koley S, Gupta S, Sandhu JS, A study on lipid profile and body fat in patients with diabetes mellitusAnthropologist 2007 9(4):295-8. [Google Scholar]
[34]. Taylor KG, John WC, Mathews KA, Wright AD, A prospective study on the effect of 12 months treatment on serum lipids and apolipoproteins A-I, A-II and B in type II (non insulin dependent)Diabetologia 1982 23(6):507-10. [Google Scholar]
[35]. Witztum JL, Mahoney EM, Branks MJ, Fisher M, Elam R, Steinberg D, Nonenzymatic glucosylation of low-density lipoprotein alters its biologic activityDiabetes 1982 31(4 Pt 1):283-91. [Google Scholar]
[36]. Kissebah AH, Alfarsi S, Evans DJ, Adams PW, Integrated regulation of very low-density lipoprotein triglyceride and apolipoprotein-B kinetics in non-insulin-dependent diabetes mellitusDiabetes 1982 31(3):217-25. [Google Scholar]
[37]. Tangvarasittichai S, Poonsub P, Tangvarasittichai O, Association of serum lipoprotein ratios with insulin resistance in type 2 diabetes mellitusIndian J Med Res 2010 131:641-8. [Google Scholar]