The NHLs are a heterogeneous group of lympho-proliferative malignancies, with distinct causes and showing distinctive patterns of behavior and responses to treatment. NHL consists of many subtypes, each with distinct epidemiology, etiology, and morphologic, immunophenotypic, and clinical features [1]. It is not a single cancer, but rather a wide group of cancers, each with a district geographical distribution, development path, age profile and prognosis. NHL is the 8th most commonly diagnosed cancer in men and the 11th in women. In terms of incidence, the disease accounts for 5.1% of all cancer cases and 2.7% of all cancer deaths [2]. In India, as per the estimates, there are approximately 23,718 new NHL cases reported each year [3]. NHL is more common in developed areas, with the highest incidence rates found in North America; Australia/New Zealand; and Northern, Western, and Southern Europe. The lowest rates are found in South-Central and Eastern Asia and the Caribbean [4].
The causes of NHL are largely unknown. Severe immunodeficiency, various infectious agents, familial aggregation, blood transfusion, and occupational exposure to pesticides and solvents have been consistently reported to increase the risk for NHL. A few studies suggest that some of these risk factors may be more strongly associated with specific subtypes of NHL [5]. However, none of these factors explain the majority of the cases [3].
The World Health Organization (WHO) classification, published in 2001 and updated in 2008, represents a worldwide consensus on the diagnosis of these tumors, accepted for use by pathologists, clinicians, and basic scientists. These principles in the 2001 WHO classification were based on the Revised European-American Classification of Lymphoid Neoplasms (REAL) published by the International Lymphoma Study Group in 1994 [6]. This classification system includes not only lymphoid neoplasms, but also myeloid, histiocytic, and mast cell neoplasms. REAL doesn’t grade these neoplasmas as high or low, as it defines that each disease entity exhibits its own peculiar clinicopathologic and immunogenetic features, and provides a framework for both clinical practice and the generation of new knowledge [7]. It broadly divides lymphoma into Hodgkin lymphoma (HL) and NHL. NHL is further subclassified based on the stage of maturation (immature vs mature) and cell of origin (B cell, T cell, or natural killer cell [NK cell]) [8].
Better understanding of the pathogenesis of lymphomas has become possible with the help of IHC and its careful utilization aids identification and the characterization of immunophenotype in most of the lymphomas [9]. The panel of markers is decided based on morphologic differential diagnosis (no single marker is specific) which includes leukocyte common antigen (LCA), B-cell markers (CD20 and CD79a), T-cell markers (CD3 and CD5) and other markers like CD23, bcl-2, CD10, cyclinD1, CD15, CD30, ALK-1, CD138 (based on cytoarchitectural pattern). No antibody is lymphoma specific hence interpretation of marker studies must be based on a panel and knowledge of a particular antigen’s expression in normal, reactive, and neoplastic conditions [8].
The current study was undertaken to ascertain frequency of Non- Hodgkin’s lymphoma subtypes, based on WHO/REAL classification system, by immunophenotypic findings.
Materials and Methods
Seventy seven cases of Lymphoma were diagnosed in the Department of Pathology, Sri Guru Ram Das Institute of Medical Sciences and Research, Amritsar (Punjab), over a period of one year (between April 2012 and April 2013). Patients were informed about the importance of the study and consent was taken in all the cases. The clinical information regarding age, sex and site of the biopsy were taken into account on routine haematoxyline and eosin stained sections.
Of the total of cases of lymphoproliferative disorders, cases diagnosed provisionally as NHL on light microscopy, were taken up for Immunophenotyping with IHC studies. There was 100 % concordance between the light microscopy and IHC studies.
The individual NHL cases were classified according to the WHO/REAL classification according to the positive or relevant negative immonophenotypic expression and tabulated to ascertain the morphological spectrum of NHL in this part of the country.
IHC Panel Employed in the Study
The panel for antibodies used for immunohistochemistry included monoclonal anibodies to CD2, CD5,CD7,CD10, CD15, CD19, CD20, CD22, CD23, CD30, CD43,CD45, CD45RO, CD56, CD68 CD117, CD1A, BCL-2, BCL-6, Cyclin D1, Ki-67, MUM1, FOXP1, SOX11, GCET-1, ALK-1 and polyclonal antibodies to CD3 and Tdt. Panel of antibodies used in a given case was dependent on the morphological evaluation and varied from 5 to 11. Immunohistochemistry was performed according to avidin-biotin peroxidase complex method, after pretreatment of antigen retrieval, by heating in microwave oven in 0.01M citrate buffer (p H-6.0). The results were tabulated and recorded individually.
Results
Of 77 cases, 30 cases (39 %) were of HL and 47 cases (61%) were of NHL. Cervical Lymph Nodes were most common site of biopsy (31 cases).
Males outnumbered females as (61%) cases were of male patients and 39% were females. Maximum incidence of NHL including both sexes was seen in age group 31-40: (21.3%) followed by age group 61-70 (19%) [Table/Fig-1].
Incidence of B cell and T cell lymphoma according to age group and sex.
| B cell lymphomas’ incidence | T cell lymphoma’s incidence | |
|---|
| AGE GROUP | MALE (%) | FEMALE (%) | MALE (%) | FEMALE (%) | TOTAL |
|---|
| 0 - 10 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 (0%) |
| 11 - 20 | 1 | 2.1 | 0 | 0 | 3 | 6.4 | 0 | 0 | 4 (8.5%) |
| 21 -30 | 1 | 2.1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 (2.1%) |
| 31 -40 | 6 | 12.8 | 4 | 8.5 | 0 | 0 | 0 | 0 | 10 (21.3%) |
| 41 - 50 | 5 | 10.6 | 2 | 4.3 | 0 | 0 | 1 | 2.1 | 8 (17%) |
| 51 - 60 | 6 | 12.8 | 2 | 4.3 | 0 | 0 | 0 | 0 | 8 (17%) |
| 61 - 70 | 3 | 6.4 | 6 | 12.8 | 0 | 0 | 0 | 0 | 9 (19%) |
| 71 - 80 | 3 | 6.4 | 2 | 4.3 | 1 | 2.1 | 0 | 0 | 6 (12.8%) |
| 81 - 90 | 0 | 0 | 1 | 2.1 | 0 | 0 | 0 | 0 | 1 (2.1) |
| 91 - 100 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0s | 0 |
B-cell lymphomas formed 89.3%, whereas T-cell lymphomas formed 10.7% of the NHLs. B cell lymphoma cases outnumbered T-cell lymphoma cases [Table/Fig-2].
Incidence rate of B-cell and T-cell lymphoma in various studies
| Authors name (year) | B-cell lymphoma | T-cell lymphoma |
|---|
| Rao A et al., (2013) [13] | 54% | 38% |
| Padhi S et al., (2012) [15] | 96% | 4% |
| Mushtaq S et al., (2008) [17] | 86% | 24% |
| Kalyan K et al., (2006) [11] | 72% | 22.5% |
| Naresh KN (2000) [18] | 79.1% | 16.2% |
| Current study | 89.3% | 10.7% |
DLBCL was the most common subtype (46.8% of all NHLs). B-cell small lymphocytic lymphoma, MCL, marginal zone B-cell lymphomas (including MALT lymphomas), Diffuse, mixed small cleaved cell and large-cell type and Follicular centre-cell lymphomas amounted to 17%, 12.8%, 2.1%, 2.1% and 4.3%, respectively. Among the T-cell lymphomas, T-cell lymphoblastic lymphoma, anaplastic large-cell lymphomas of T/null-cell type, and AITL accounted for 6.4%, 2.1%, and 2.1% of all NHL cases, respectively.
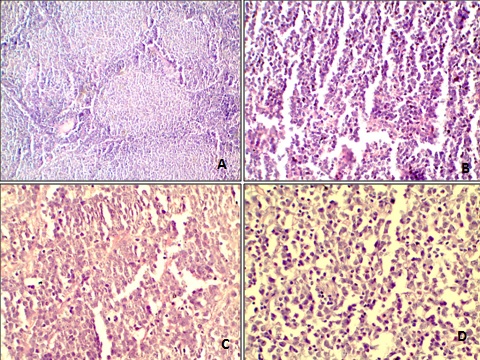
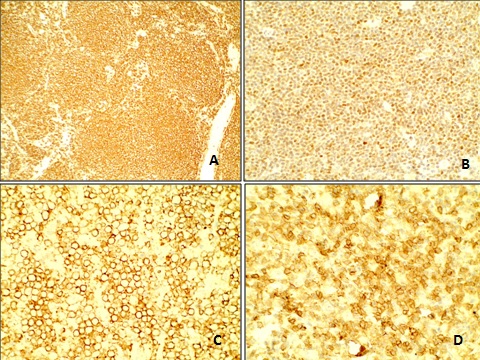
Classification of the cases in B and T-cell type & further sub-classification based upon WHO/ REAL classification system, after evaluation of results of immunohistochemistry, is represented in [Table/Fig-3 and 4]. Light microscopic findings in various NHL 1A– Folliclular Lymphoma [H & E 200X]; 1B- mantle Cell Lyphoma [H & E 200 X]; 1C- Diffuse large B Cell Lymphoma [H & E 400 X]; 1D- Angioimmunoblastic T- Cell Lymphoma [Table/Fig-5].Correseponding IHC immuno-positive markers of NHL shown in [Table/Fig-6]. 2A- CD 45 positivity in Follicular lymphoma; 2B- Bcl-2 positivity in Mantle Cell Lymphoma; 2 C- CD20 positivity in Diffuse large B Cell Lymphoma; 2 D- CD 3 positivity in Angioimmunoblastic T Cell Lymphoma.
| Lymphoma Subtypes | Number | % age |
|---|
| A | Precursor B-cell lymphoma: | 1 | 2.1 |
|---|
| B | Mature B- cell Neoplasms | | |
|---|
| 1 | B-cell chronic lymphatic leukaemia/small lymphocytic lymphoma | 08 | 17 |
| 2 | B-cell prolymphocytic leukaemia | 0 | - |
| 3 | Lymphoplasmacytic lymphoma/immunocytoma | 0 | - |
| 4 | Mantle-cell lymphoma | 06 | 12.8 |
| 5 | Follicular lymphoma | | |
| (a) Folliular grade 1 | 0 | - |
| (b) Follicular grade 2 | 1 | 2.1 |
| (c) Follicular grade 3 | 2 | 4.3 |
| 6 | Diffuse, predominantly small cleaved cell type | 0 | - |
| 7 | Diffuse, mixed small cleaved cell and large-cell type | 1 | 2.1 |
| 8 | Marginal zone B-cell lymphoma of mucosa associated lymphoid tissue (MALT) type | 01 | 2.1 |
| 9 | Nodal marginal zone B-cell lymphoma + / -monocytoid B cells | 0 | - |
| 10 | Splenic marginal zone B-cell lymphoma | 0 | - |
| 11 | Hairy-cell leukaemia | 0 | - |
| 12 | Diffuse large B-cell lymphoma | 22 | 46.8 |
| 13 | Primary mediastinal (thymic) B-cell lymphoma | 0 | - |
| 14 | Burkitt lymphoma | 0 | - |
| 15 | Plasmacytoma/myeloma | 0 | - |
| 16 | High-grade (aggressive) B-cell lymphoma -NOS | 0 | - |
| 17 | Low-grade (indolent) B-cell lymphoma - NOS | 0 | - |
| 18 | Low-grade (indolent) B-cell lymphoma - NOS | 0 | - |
| 19 | B-cell non-Hodgkin's lymphoma - NOS | 0 | - |
| TOTAL | 42 | 89.3 |
| No. | Lymphoma Subtypes | Number | % age |
|---|
| A | Precursor T-cell lymphoblastic lymphoma/leukaemia | 3 | 6.4 |
|---|
| B | Mature T-cell and NK-cell neoplasms | | |
|---|
| 1 | T-cell prolymphocytic leukaemia | 0 | - |
| 2 | Extranodal NK/T-cell lymphoma - nasal | 0 | - |
| 3 | Mycosis fungoides/Sezary syndrome | 0 | - |
| 4 | Angioimmunoblastic T-cell lymphoma (AITL) | 1 | 2.1 |
| 5 | Peripheral T-cell lymphoma (unspecified) | 0 | - |
| 6 | Systemic anaplastic large-cell lymphoma (ALCL) (T- and null-cell types) | 1 | 2.1 |
| 7 | Systemic anaplastic large-cell lymphoma, Hodgkin type | 0 | - |
| 8 | Primary cutaneous CD30+ lymphoproliferative disorders | 0 | - |
| 9 | Subcutaneous panniculitis-like T-cell lymphoma | 0 | - |
| 10 | Hepatosplenic g-d T-cell lymphoma | 0 | - |
| 11 | Low-grade (indolent) NHL | 0 | - |
| 12 | High-grade (aggressive) NHL | 0 | - |
| 13 | NHL - no further classification (NOS) | 0 | - |
| 14 | TOTAL | 5 | 10.63 |
Light microscopic findings in various NHL 1A- Folliclular Lymphoma [H & E 200X]; 1B- mantle Cell Lyphoma [H & E 200 X]; 1C- Diffuse large B Cell Lymphoma [H & E 400 X]; 1D- Angioimmunoblastic T- Cell Lymphoma
Correseponding IHC immuno-positive markers of NHL shown in Figure-1. 2A- CD 45 positivity in Follicular lymphoma; 2B- Bcl-2 positivity in Mantle Cell Lymphoma; 2 C- CD20 positivity in Diffuse large B Cell Lymphoma; 2 D- CD 3 positivity in Angioimmunoblastic T Cell Lymphoma
Discussion
Immunohistochemistry is applied in 3 circumstances: To completely phenotype the abnormal population detected by morphology, to further characterize an abnormal population identified by flow cytometry, or to screen ostensibly “reactive” tissue to determine if a subtle abnormal population is present [8]. This identification of type of lymphomas, in given study, is done by REAL/WHO classifications system with the use of multiple parameter based on clinical, morphologic, and biologic features of disease entities. The results of study conducted by Aggarwal D et al., shows advantage of REAL classification system over working formulation classification of NHL [10] while Kalyan K et al., preffered WF system over REAL/WHO [11].
The occurrence of NHL is higher in men [worldwide age-standardized rate (ASR) 6.1/100 000] then women (ASR 4.2/100 000)(3).In given study too males outnumbered females as (29/47, 61%) cases were of male patients and (18/47, 39%) were females. This male preponderance has been reported in other studies too [11–16].
NHL is more common in older adults than younger adults, hence age presents to be strong risk factor for this disease. Incidence data obtained from the United States National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) Program accounted that the incidence of total lymphoid neoplasms increased monotonically with age in all race and sex subgroups. Steep increases in incidence with age were observed for most subtypes [12]. But in current study maximum incidence of Non Hodgkin Lymphoma including both sexes was seen in age group 31-40: (10/47, 21.3%) followed by age group 61-70 (9/47,19%). Results of study conducted by Roy et al., was in agreement with other studies. It reported that 63.6% NHL occurred after the age of 40 years with a peak between 51 and 60 [13]. Similarly, in a study conducted by Vallabhajosyula et al., the median age of study population was 55.5 years (interquartile range 41-67 years) [14]. Padhi et al., too reported that peak incidence was during the 4th to 5th decade of life [15].
Age and gender not only serve as risk factor for NHL and its subtypes but also effect treatment outcome of disease and survival rate of patients.
B-cell lymphoma cases outnumbered T-cell lymphoma cases. Similar results have also been reported by other studies too.
DLBCL is the most common of the aggressive NHLs and constitutes 30%–58% of it [17]. This was observed in given study as well as studies reported by several other authors, worldwide. In current study 46.8% of all NHLs were found to be DLBCL. In two different studies reported from Mumbai, India, in year 2000 [18] and 2011 [16], incidence rate of DLBCL was found to be 34% and 42% respectively. Similarly, various studies conducted in South India also reported high incidence of DLBCL. Roy et al., [13], and Kalyan et al., [15] too observed DLBCL to be the most common subtype comprising 29.3% [13] and 26% [11] of cases respectively. While Padhi et al., reported incidence to be high as 69%. Tilly and Dreyling [17] reported incidence in the European Union to be 3–4/100 000/year. The incidence increases with age from 0.3/100 000/year (35–39 years) to 26.6/100 000/year (80–84 years). Among all cases of primary gastrointestinal non-Hodgkin lymphoma (GI NHL) in a North American population, Howell et al., reported 47% DLBCL [19]. Mushtaq et al., reported 76% incidence of DLBCL in a study in Pakistan [20].
FL is the second most common subtype of lymphoma and represents about 20% to 25% of cases of NHL in the U.S. and Europe. Its incidence is compartively lower in some parts of the world such as Asia [21]. In Given study B-cell small lymphocytic lymphoma, mantle-cell lymphoma, Follicular centre-cell lymphomas, and marginal zone B-cell lymphomas (including MALT lymphomas) amounted to 17%, 12.8%, 4.3%, and 2.1%, respectively. Roy et al., reported 6.8% of FL, 2.8% of marginal zone lymphoma (MZL), 4% of MCL, 3.7% of chronic lymphocytic lymphoma/small lymphocytic lymphoma (CLL/SLL) [13]. Incidence of Follicular centre-cell lymphomas, B-cell small lymphocytic lymphoma, MCL, and marginal zone B-cell lymphomas (including MALT lymphomas) amounted to 12.6%, 5.7%, 3.4%, and 8.2%, respectively in study by Naresh et al., [18]. Howell et al., reported 8% follicular and 5% mantle cell lymphoma in GI NHL cases [20]. MCL cases represent between 2 and 10% of all NHL. In their analysis Aschebrook-Kilfoy and coworkers illustrated that the MCL incidence is increasing more rapidly in elderly persons, particularly in white males [22].
Among the T-cell lymphomas, T-cell lymphoblastic lymphoma, anaplastic large-cell lymphomas of T/null-cell type, and AITL accounted for 6.4%, 2.1%, and 2.1% of all cases, respectively. Lymphoblastic lymphoma is rare, accounting for 1% to 2% of all NHL and is of T-cell phenotype in 90% of cases [23]. Roy et al., reported 10.5% (34 cases) of anaplastic large cell lymphoma, 1.85% (6 cases) of AITL and 0.9% (3 cases) of adult T-cell lymphoma/leukemia (ATLL) [13]. Sagner et al., reported 9%, anaplastic large-cell lymphomas-alk-positive and 6%, anaplastic large-cell lymphoma-alk-negative and 18% T-lymphoblastic lymphomas [16]. Naresh et al., observed incidence of T-cell lymphoblastic lymphoma, anaplastic large-cell lymphomas of T/null-cell type to be 6% and 4.3% respectively [18]. While Kalyan K et al., [11] reported incidence of T lymphoblastic lymphoma (15%) and peripheral T cell angioimmunoblastic lymphoma (6%). In a study conducted on 1314 patients in Italy, Federico M diagnosed 18.5% cases with AITL and defined it as a rare clinicopathologic entity characterized by an aggressive course and dismal outcome with current therapies [24].
Conclusion
Incidence of Non-Hodgkin’s lymphoma is increasing worldwide and this has been observed in India too.
The distribution of NHL subtypes in India shows important differences with those from the rest of the world. FL and MCL are less common in India compared to Europe and the USA. While T-cell lymphoblastic lymphoma and anaplastic large T/null cell lymphoma are more prevalent in India.
Immunohistochemistry is a useful and necessary diagnostic aid and helps in sub-typing different types of NHL.
Limitation of study is that it had small number of cases as they were taken over a year only. Subsequently we plan to increase the cases over coming years and also to follow these cases to see the behavior and growth of these NHL subtypes.