Auricular Prosthesis-A Case Report
Rajyalakshmi Ravuri1, Bheemalingeshwarrao2, Suchita Tella3, Kiran Thota4
1Reader, Department of Prosthodontics,Kamineni Institute of Dental Sciences, Narketpally-508254, Nalgonda, Andhra Pradesh, India.
2Reader, Department of Prosthodontics,Vishnu Dental College, Bhimavaram, Andhra Pradesh, India.
3Reader, Department of Prosthodontics,Kamineni Institute of Dental Sciences, Narketpally-508254, Nalgonda, Andhra Pradesh, India.
4Reader, Department of Prosthodontics,Kamineni Institute of Dental Sciences, 508254, Nalgonda, Andhra Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rajyalakshmi Ravuri, H.No. 22-23/1, Plot no- 45,V V Nagar, Chaitanyapuri, Dilshuknagar, Hyderabad, India.
Phone: 9441476294,
E-mail: rajuravuri@yahoo.co.in
Loss of facial organs in an individual may be developmental anomalies or acquired. The missing parts of the face ear, eyes and nose are considered as maxillofacial defects which can be rehabilitated by the prosthesis and/or cosmetic surgeries. This art of science has developed into a more reliable and predictable process due to ever increasing development of materials and equipments used in the procedure. This article describes a simple technique to rehabilitate patients with auricular defects which are both aesthetically acceptable and economical for the individual.
Maxillofacial defects, Auricular prosthesis, Facial rehabilitation, Spectacle retention
Case Report
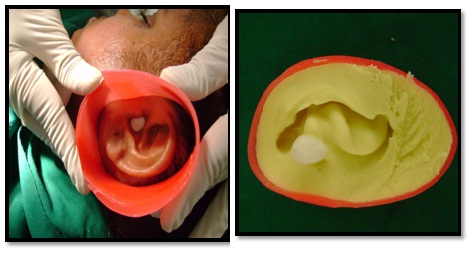
A 35-year-old female patient reported to the department of prosthodontics with a history of congenitally missing right ear [Table/Fig-1]. The surrounding facial skin and hair near the defect and contra-lateral ear was protected by applying petrolatum gel. The external auditory canal was blocked with gauze to prevent entry of impression material. Three lines were marked from the right side to left side of the face taking the superior, middle and inferior border of the natural ear on left side as reference [1] [Table/Fig-2a,b,c]. The outline is marked with a marker pen on the defect side and these markings were transferred on to the working cast [Table/Fig-2c]. These lines were of value in assessing the proper orientation of the prosthesis. Elastomeric impression material of putty consistency was used to make the impression of the defect side which was boxed and supported by pouring quick setting plaster [2] [Table/Fig-3a,b]. Similarly the impression of the natural ear on the left side was made using irreversible hydrocolloid impression material [Table/Fig-3c,d] and a stone cast was obtained which was used as a guide to sculpt the wax pattern [Table/Fig-4a]. The prosthesis can be sculpted from the beginning or ‘donor technique’ may be used. For this patient sculpting was done from the beginning. It was done by dividing the cast of the normal ear into equal sections so that contours are more easily verified [Table/Fig-4c] [3]. The wax prosthesis was tried on the patient and evaluated for the correct fit on the tissue, correct horizontal alignment with the contra lateral ear, projection of the ear in relation to the side of the head and integrity of the margins during simple jaw movements was checked [Table/Fig-4c,d]. The wax pattern was invested in the denture flask using irreversible hydrocolloid impression material [4] [Table/Fig-5a,b]. After the material was set, the wax pattern was retrieved. A mixture of tooth coloured, pink and clear self curing acrylic resin was used to make the prosthesis. Colour was incorporated in the monomer incrementally to achieve desired skin tone. Small increments of polymer and monomer were mixed and tried against the patients face or contra-lateral ear in every stage [Table/Fig-9]. Once the required shade was obtained, adequate amount of polymer and monomer were mixed to fill the mould. The resin was allowed to polymerize completely [Table/Fig-5c]. After trimming, the prosthesis was tried on the patients face. The prosthesis was attached to the spectacle frame using cyanoacrylate. A separating sheet was placed between the skin and prosthesis to avoid any tissue damage by cyanoacrylate [Table/Fig-7a]. Characterization of the ear prosthesis was done by addition of ear ring to the prosthesis [Table/Fig-7b]. Thus lost facial structure was restored to patient’s satisfaction in a manner that was both aesthetically acceptable and cost effective [Table/Fig-8a,b].
Discussion
Loss of external ear can be congenitally missing or acquired due to accidental trauma or malignant disease. Congenital anomaly of the external ear may be termed as “Microtia”. It includes a spectrum of deformities from a grossly normal but small ear to the absence of the entire external ear. These deformities account for three in every 10,000 births, with bilaterally missing ears seen in fewer than 10% of all cases [5]. The patient presented in this article had a unilateral congenitally missing ear. Leading life with this kind of a physical deformity is very stressful and often depressing for the patient. It directly affects the patient’s mental, social and psychological well being. Acceptable aesthetics in restoring a prominent facial defect, such as malformed ear is a challenging task for maxillofacial prosthodontist. Surgical reconstruction of ear results in morphology that is less similar to opposite side because of its complex nature and it is considered to be one of the most demanding challenges for the plastic surgeons [6]. Prosthesis fabrication is the most conservative method of correcting the ear deformity [4]. The commonly followed technique in making the wax pattern is to make impression and cast of the contra-lateral ear to be used as reference while sculpting the wax pattern. In the literature various techniques have been suggested for sculpting the pattern [7-9]. Recent advances in the field of maxillofacial prosthetics for the wax pattern fabrication like 3D rapid prototyping had enabled the clinicians to provide quality health care to patients in need [10,11]. There are acrylics and silicone based materials available for the fabrication of the maxillofacial prosthesis but traditionally acrylic resin had been the material of choice for fabrication of ear prosthesis, as it is economically viable treatment option [4].
The patient was willing for implant retained auricular prosthesis but was apprehensive of the surgical procedure and the final prosthesis. So we planned a temporary prosthesis to use for short time and then decide on the definitive one. Considering this, irreversible hydrocolloid material was used to invest the wax pattern rather than dental plaster by which the wax pattern was preserved for future needs [4]. In literature to preserve wax pattern combination of dental stone and putty polyvinyl siloxane had been suggested for investing [12]. The various options available to retain the ear prosthesis are- implant retained, [13,14] adhesive retained, magnet retained, [15] hair band retained and spectacle retained prosthesis [16]. Implant retained is though superior, patient was apprehensive of the surgical procedure and so we opted for a spectacle frame and hair band retained prosthesis. The external ear is missing for the individual hence spectacle frame alone would be difficult for orientation of the prosthesis. Also this method is cost effective and aesthetically acceptable for patients who decline or postpone implant retained prosthesis reconstruction. The spectacle frame is the most commonly used mode of retention for ear prosthesis as it is easy to attach, require less chair side time, cost effective and can be placed and removed at the will of the patient. Among the newer avenues for rehabilitation of microtia is tissue engineering. This is the science in which a group of high density functional dissociated cells are seeded onto synthetic biocompatible, biodegradable polymers, which are then transplanted into the animal model for generation of functional tissue. Tissue engineering studies done in animal models have opened many possibilities of potential clinical applications [17,18].
Extraoral view of the defect

Markings for the extension of the ear

Putty impression of the defect

Alginate impression of the contra-lateral ear
Wax pattern of the ear prosthesis
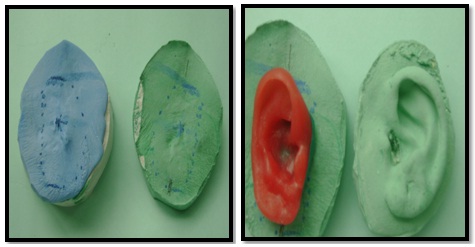

Investing the pattern in alginate



Spectacle retained ear prosthesis with external characterization

Final ear prosthesis in position improving the self confidence of the individual

Summary
Communication and education is the key factor for the acceptance of the prosthesis. Patient acceptance, aesthetics, compatibility, durability and prosthetic considerations like availability of materials, ease of processing, ease of duplication lead to success of treatment and making the prosthesis look life like and giving the patient social confidence.
[1]. DN Shah, CJ Chauhan, Auricular prosthesis – the overlooked skill in prosthodonticsThe Journal of Ahmedabad Dental College and Hospital 2010 1:37-40. [Google Scholar]
[2]. JC Lemon, S Kiat Ammay, L Gettleman, JW Martin, Facial prosthetic rehabilitation: pre-prosthetic surgical techniques and biomaterials.Cure Opin Otolaryngol Head Neck Surg 2005 13:255-62. [Google Scholar]
[3]. SS Mantra, RU Thombre, Prosthetic rehabilitation of a patient with bilateral auricular deformity.J Adv Prosthodont 2011 3:101-5. [Google Scholar]
[4]. R Madhan , Sanjna Prosthetic management of a patient with Treacher Collins syndromeInd J Dent Res 2006 17:78-81. [Google Scholar]
[5]. PS Kumar, RC Savadi, Bilateral implant - retained auricular prosthesis for a patient with congenitally missing ears. A clinical reportJ Prosthodont 2012 21:322-27. [Google Scholar]
[6]. RR Wang, CJ Andres, Hemifacial microstomia and treatment options for auricular replacement: a review of literature.J Prosthet Dent 1999 82:197-204. [Google Scholar]
[7]. LM Sykes, AM Parrot, P Owen, Applications of rapid prototyping technology in maxillofacial prostheticsInt J Prosthodont 2004 17:454-89. [Google Scholar]
[8]. JC Nusinov, WD Gay, A method for obtaining the reverse image of an earJ Prosthet Dent. 1980 44:68-71. [Google Scholar]
[9]. JC Lemon, MS Chambers, PJ Wesley, JW Martin, Technique for fabricating a mirror image prosthetic earJ Prosthet Dent 1996 75:292-93. [Google Scholar]
[10]. L Peter, G Jonathan, R Noorberto, Designing and manufacturing an auricular prosthesis using computed tomography, 3- dimensional photographic imaging and additive manufacturing: a clinical report.J Prosthet Dent 2011 105:78-82. [Google Scholar]
[11]. Thotapalli Suman , Fabrication of mirror image prosthetic ears - a short reviewAnaplastology 2013 120:2-23. [Google Scholar]
[12]. ES Asher, JH Evans, RF Wright, JJ Wazen, Fabrication and use of a surgical template for placing implants to retain auricular prosthesisJ Prosthet Dent 1999 81:228-233. [Google Scholar]
[13]. Singh Ajay, G Shounak, Sumankar Ahmed Imran, Silicone prosthesis for a patient with unilateral ear defect: a clinical case reportEur J Gen Dent 2013 2:315-19. [Google Scholar]
[14]. HG EL Charkawi, AG EL Sharkawi, A simplified technique for orientation of a bone anchored auricular prosthesis: a clinical report.J Oral Maxillofac Res 2012 3:1-7. [Google Scholar]
[15]. Chung Robin WC, Siu Adam SC, Chu Frederick CS, Chow Tak W, Magnet retained auricular prosthesis with an implant supported composite bar: a clinical report.J Prosthet Dent 2003 89:446-49. [Google Scholar]
[16]. Mohamed Kasim, V Anand Kumar, Mani Umamaheshwari, B Yadharth, TV Padmanabhan, Rehabilitation of an auricular defect using spectacle retained silicone ear prosthesis and ear stentInt J Prost Rest Dent 2012 2:29-33. [Google Scholar]
[17]. L Nayyer, KH Patel, A Esmaeili, Tissue engineering: revolution and challenge in auricular cartilage reconstructionPlast Reconst Surg 2012 129:1123-37. [Google Scholar]
[18]. A Sterodimas, J de Faria, WE Correa, I Pitanguy, Tissue engineering and auricular reconstruction: A reviewJ Plast Reconstr Aesthet Surg 2009 62(447):52-58. [Google Scholar]