TB-DOTS Outcome in Relation to HIV Status: Experience in a Medical College
Chennaveerappa P.K.1, Jayashree Nagaral2, Nareshkumar M.N.3, Praveen G.4, Halesha B.R.5, M.V. Vinaykumar6
1 Associate Professor, Department of Pulmonary Medicine, Hassan Institute of Medical Sciences, Hassan, Karnataka, India.
2 Assistant Professor, Department of Pharmacology, Hassan Institute of Medical Sciences, Hassan, Karnataka, India.
3 Junior Resident, Department of Pulmonary Medicine, Hassan Institute of Medical Sciences, Hassan, Karnataka, India.
4 Assistant Professor, Department of Community Medicine, Hassan Institute of Medical Sciences, Hassan, Karnataka, India.
5 Assistant Professor, Department of General Medicine, Hassan Institute of Medical Sciences, Hassan, Karnataka, India.
6 Assistant Professor, Department of ENT, Hassan Institute of Medical Sciences, Hassan, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Chennaveerappa P.K., Associate Professor, Department of Pulmonary Medicine, SC Hospital, Hassan Institute of Medical Sciences, Hassan-573201, Karnataka, India.
Phone: 919480303972,
E-mail: drchennamd@yahoo.com
Background and Objective: There is scarce information regarding TB associated with Human Immunodeficiency Virus (HIV) infection treated under routine program conditions in medical colleges of India. This study evaluates the clinical profile and outcome of TB-DOTS treatment by HIV status.
Methods: Total two hundred and eighty TB patients registered under Revised National Tuberculosis Control Program Revised National TB Control Program (RNTCP) during January 2011 and December 2012 in a teaching hospital of South India were enrolled in the study. The demographic profile, treatment related data of these patients was obtained from RNTCP treatment card and the DOTS outcome of all enrolled cases depending on their HIV status was evaluated. Data was analysed using descriptive statistics and chi-square test.
Results: Among 280 TB patients enrolled 41 were HIV positive patients and 239 HIV negative. About 21% patients were retreatment patients. Over all, pulmonary TB was still the commonest form of TB among the registered patients. However, Extra Pulmonary (EPTB) was high among HIV positive TB patients. Treatment success among HIV positive TB patients was lower than HIV negative TB patients (61% vs. 79%). Further, 19.5% HIV positive and 8.3% HIV negative patients died. The proportions of defaulters and failures were similar in HIV positive and HIV negative patients.
Conclusion: HIV co-infected TB patients responded poorly to DOTS as evidenced by lower success rates and higher mortality than HIV negative TB patients. A significant proportion of retreatment patients in our study is the matter of concern.
Human Immunodeficiency Virus (HIV), Directly Observed Treatment Short Course (DOTS), Tuberculosis, Revised National TB Control Program (RNTCP) ligament
Introduction
The worldwide spread of HIV infection has undermined human defence against Mycobacterium tuberculosis (Mtb). HIV infection is the strongest risk factor for the progression of latent Mtb infection to active disease [1,2]. People living with HIV who are also infected with TB are much more likely to develop TB disease than those who are HIV negative [3].
HIV infection is also associated with unusual clinical presentations of TB, increase in extra-pulmonary and acid-fast bacilli (AFB) smear negative pulmonary disease, and atypical findings on chest radiography, all making the diagnosis of HIV associated TB problematic [4].
RNTCP in India uses a fully intermittent thrice weekly rifampicin containing regimen for all TB patients including those who are HIV infected [5].
The treatment success in TB patients is a major challenge in TB programmes, which is influenced by number of factors including HIV co-infection [6]. The mortality rate from HIV associated TB in developing countries is high, it is due to failure of anti TB treatment or complications of HIV [7]. Yet, there is limited information on impact of HIV co-infection on TB treatment outcome from a Directly Observed Treatment Short Course (DOTS) centre of a medical college. This study was conducted to evaluate the clinical profile and outcome of DOTS in relation to HIV status.
Materials and Methods
This prospective observational study was conducted at a tertiary care teaching hospital of South India. A total of 280 patients registered under RNTCP during January 2011 and December 2012 were enrolled in the study. The study group comprised of 41 HIV positive and 239 HIV negative patients and informed consent was taken from all the patients. All the enrolled patients were treated following RNTCP guidelines and followed up for 6-8 months and those HIV co-infected TB patients were treated at Anti Retroviral Therapy (ART) centre of the hospital as per National AIDS Control Program (NACO) guidelines. The demographic profile, type of TB, HIV status, treatment outcome of DOTS at the end of the treatment was recorded from TB treatment card. All enrolled patients were stratified depending on various age groups, gender, type of TB and HIV status. Treatment outcomes of all the cases were in accordance with RNTCP definitions and classified as cured, treatment success, defaulters, treatment failure and deaths. Data was analysed to evaluate various types of TB and the outcome of DOTS in relation to HIV status of the enrolled cases.
Statistical Analysis
Data was entered into Microsoft excel and analysis was done using Graph pad Instat statistical software. Descriptive statistics was used for calculating proportions. The Chi-square test or alternatively Fisher’s Exact test was used to determine if there were associations between categorical variables. All tests were evaluated at a significance level of 0.05.
Results
Among 280 TB patients included during the period of study, 41 (14.6%) were HIV positive and 239 (85.4%) were HIV negative. Their demographic characteristics are given in [Table/Fig-1]. Majority of the patients were males in the age group 15-44 years.
Baseline characteristics and treatment outcome of all registered TB cases by HIV status
| Characteristics | Total (n) | % | HIV Positive (n) | % | HIV Negative (n) | % |
|---|
| Overall | 280 | | 41 | 14.6 | 239 | 85.4 |
| Gender |
| Male | 182 | 65 | 28 | 68.3 | 154 | 64.4 |
| Female | 98 | 35 | 13 | 31.7 | 85 | 35.6 |
| Age at registration |
| <14 | 18 | 6.4 | 1 | 2.4 | 17 | 7.1 |
| 15-29 | 87 | 31.1 | 5 | 12.2 | 82 | 34.4 |
| 30-44 | 93 | 33.2 | 22 | 53.7 | 71 | 29.7 |
| 45-59 | 55 | 19.6 | 12 | 29.3 | 43 | 17.9 |
| >60 | 27 | 9.7 | 1 | 2.4 | 26 | 10.9 |
| Type of TB |
| New cases |
| New smear positive | 93 | 42.1 | 9 | 29.1 | 84 | 44.2 |
| New smear negative | 48 | 21.7 | 6 | 19.3 | 42 | 22.1 |
| Extrapulmonary | 80 | 36.2 | 16 | 51.6 | 64 | 33.7 |
| Re-treatment cases |
| Smear positive | 45 | 76.3 | 4 | 40 | 41 | 83.7 |
| Smear negative | 9 | 15.3 | 2 | 20 | 7 | 14.3 |
| EPTB | 5 | 8.4 | 4 | 40 | 1 | 2 |
| Overall Type of TB |
| Overall pulmonary | 195 | 69.6 | 21 | 51.2 | 174 | 72.8 |
| Overall extrapulmonary | 85 | 30.4 | 20 | 48.7 | 65 | 27.2 |
| Treatment outcome |
| Treatment Success | 214 | 76.4 | 25 | 60.98 | 189 | 79.1 |
| Cured | 89 | 64.49 | 7 | 53.8 | 82 | 66.6 |
| Died | 28 | 10 | 8 | 19.5 | 20 | 8.3 |
| Default | 20 | 7.14 | 3 | 7.3 | 17 | 7.1 |
| Failure | 15 | 5.36 | 2 | 4.8 | 13 | 5.4 |
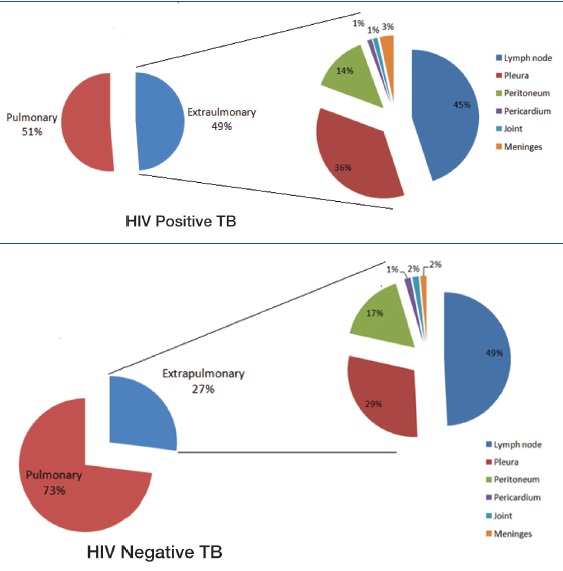
About 24.4% HIV positive and 20.5% HIV negative were retreatment patients. EPTB was higher among HIV positive (48.7%) as compared to HIV negative patients. [Table/Fig-1]. Lymph node involvement was most common in both HIV positive and negative patients (45% and 49%) [Table/Fig-2]. Over all smear positivity was lower in HIV positive as compared to HIV negative patients (61.9% vs 71.8%) [Table/Fig-1].
Type and form of TB in relation to HIV status
The lower treatment success rate and higher death rate observed in HIV positive compared to HIV negative patients was not statistically significant (p>0.05). But, the treatment outcome by smear status showed significant results (p<0.05) [Table/Fig-3].
Treatment Outcome of Pulmonary TB Patients in Relation to Sputum Smear
| Treatment Outcome | | HIV positive pulmonary TB | HIV negative pulmonary TB |
|---|
| n | Smear Positive n(%) | Smear Negative n(%) | Smear Positive n(%) | Smear Negative n(%) |
|---|
| Cured | 89 | 7(53.84) | 0 | 82(65.6) | 0 |
| Treatment completed | 52 | 0 | 5(62.5) | 0 | 47(96) |
| Death | 22 | 3(23.07) | 3(37.5) | 14(11.2) | 2(4) |
| Default | 18 | 2(15.38) | 0 | 16(12.8) | 0 |
| Failure | 14 | 1(7.69) | 0 | 13(10.4) | 0 |
| Total | 195 | 13 | 8 | 125 | 49 |
Discussion
Our study evaluated the clinical profile and treatment outcome of DOTS by HIV status of patients. This study reports a maximum prevalence of HIV-TB co-infection in the economically productive age group of 15-44 years with male preponderance which was also observed in earlier Indian studies [8,9].
The proportion of retreatment TB patients observed in the study was higher than the RNTCP norms. In HIV-infected patients, the risk of recurrent disease is higher, and previous work has demonstrated that this can be due to treatment failure, emergence of drug resistance during therapy or reinfection with a new strain of Mtb [10]. The reasons for higher proportions of retreatment cases among HIV negative patients need to be further evaluated.
In HIV positive TB patients pulmonary TB is the commonest form of TB [11]. Similar finding was observed in our study. The lower sputum positive detection rate and increasing frequency of EPTB (49%) in HIV positive patients might be due to unrecognized mycobacteremia in severely immunocompromised patients. The level of immunosuppression among HIV positive patients was not assessed in this study. Unrecognised TB in patients with HIV disease has far reaching consequences including delayed diagnosis, unacceptable therapeutic delay and even rapid progression to untreatable TB [8]. It has been observed that presence of a cough for more than three weeks is not sensitive enough on its own as a symptom of TB in HIV infected persons [12]. Mycobacterial culture is the gold standard for TB diagnosis and is now routinely recommended to assist the diagnosis of TB in HIV infected persons, although it is slow and costly [13].
The treatment success rate of all registered patients was lower than the RNTCP norms, district average [14] and national average for the corresponding year. The study revealed lower success rate among HIV positive compared to HIV negative TB patients (61% vs 79%) but, higher compared to other recent studies [15–17]. Lower success rate may be attributable to high mortality and default rate reported among HIV positive patients. The high mortality associated with HIV co-infected TB is also observed in several studies [9, 17] and closer to state average [3]. The reason for this could also be due to other opportunistic infections among HIV patients. Our analysis showed almost similar default and failure rates among HIV positive and HIV negative patients.
Our results should be viewed in the light of certain limitations which was a single site study that may not be representative of the average standard of care in other resource limited areas. Using patient treatment card as a primary source may limit the accuracy of information. The potential factors like clinical manifestations, staging of HIV, occurrence of other opportunistic infections, duration of ART, which are likely to influence the outcome of DOTS, were not dealt with. The exact cause of death could not be ascertained. Despite these limitations, the study findings are useful to inform policy and programmes to improve management of TB/HIV in patients.
Conclusion
The study showed overall treatment success rate of DOTS was lower than RNTCP norms for the corresponding year irrespective of HIV status. The higher proportion of retreatment patients in study population is a matter of concern. The lower success rate among HIV positive patients compared to HIV negative TB patients observed might be due to atypical presentation, delayed diagnosis and drug resistant TB. The results of the study demonstrate that there is a need to strengthen the DOTS in our study area.
Recommendations
Early diagnosis and access to faster diagnostic methods of TB in seropositive patients.
Decentralization of ART centres like DOTS centre.
Referral and linkage services should be improved and strengthened for enhanced treatment adherence.
[1]. Barnes PF, Bloch AB, Davidson PT, Snider DE Jr, Tuberculosis in patients with human immunodeficiency virus infectionN Engl J Med 1991 324:1644-50. [Google Scholar]
[2]. Hopewell PC, Impact of human immunodeficiency virus infection on the epidemiology, clinical features, management, and control of tuberculosisClin Infect Dis 1992 15:540-7. [Google Scholar]
[3]. World Health OrganizationGlobal Tuberculosis report 2012 [Google Scholar]
[4]. Lucas S B, De Cock K M, Hounnou A, Contribution of tuberculosis to slim disease in AfricaBMJ 1994 308:1531-33. [Google Scholar]
[5]. TB India 2012. Revised National TB Control Program: Annual Status Report http://tbcindia.nic.in p 49-50 [Google Scholar]
[6]. Banerjee A, Moyo S, Salaniponi F, Harries A, HIV testing and tuberculosis treatment outcome in a rural district in MalawiTrans R Soc Trop Med Hyg 1997 91:707-08.doi: 10.1016/S0035-9203(97)90533-2 [Google Scholar]
[7]. Central TB Division, Ministry of Health and Family Welfare, India. TB India 2006: RNTCP Status Report. 2006. New Delhi, India. http.Org/documents.asp Published March 2006 [Google Scholar]
[8]. Rajasekaran S, Mahilmaran A, Annadurai S, Kumar S, Raja K, Manifestation of tuberculosi in patients with human immunodeficiency virus. A large Indian studyAnn Thirac Med 2007 2:58-60. [Google Scholar]
[9]. Sanchez M, Bartholomay P, Arakaki-Sanchez D, Enarson D, Bissell K, Outcomesof TB HIV status in National Recording Systems in Brazil, 2003-2008PLoS ONE 2012 7(3):33129doi:10.1371/journal.pone.0033129 [Google Scholar]
[10]. Richard EC, Gavin JC, Recurrent Tuberculosis—Relapse, Re-infection and HIVJ Infect Dis 2010 March 201(5):653-655. [Google Scholar]
[11]. World Health Organization. TB/HIV A Clinical Manual Geneva. (WHO/HTM/TB/2004.329) [Google Scholar]
[12]. Reid MJ, Shah NS, Approaches to tuberculosis screening and diagnosis in people with HIV in resource-limited settingsLancet Infect Dis 2009 9:173-84. [Google Scholar]
[13]. World Health Organization. Improving the diagnosis and treatment of smear-negative pulmonary and extrapulmonary tuberculosis among adults and adolescents: Recommendations for HIV-prevalent and resource-constrained settings. Geneva: Switzerland 2010 [Google Scholar]
[14]. RNTCP Karnataka (all Quarters 2011), State TB Cell, Karnataka, Bangalore. 2011 [Google Scholar]
[15]. Vijay S, Kumar P, Chauhan LS, Narayan Rao SV, Vaidyanathan P, Treatment Outcome and mortality at one and half year follow-up of HIV Infected TB Patients Under TB Control Programme in a District of South IndiaPLoS ONE 2011 6(7):e21008doi:10.1371/Journal.pone.0021008 [Google Scholar]
[16]. van den Broek J, Mfinanga S, Moshiro C, Impact of human immunodeficiency virus infection and outcome of treatment and survival of tuberculosis patients in Mwanza, TanzaniaInt J Tuberc Lung Dis 1998 2(7):547-552. [Google Scholar]
[17]. Upasna A, Amitabh K, Digamber B, Profile of HIV associated tuberculosis at a tertiary Institute in setting of freeAnti-Retroviral Therapy 2009 57:685-90. [Google Scholar]